
- Is this digoxin toxicity?
- Do I need to start pressors?
- If the patient’s bradycardia does not respond to Atropine, what should I do next?
- What other tests need to be considered immediately?
What is Digoxin?
- Digoxin is a cardioactive glycoside that was derived from the foxglove plant Digitalis Purpurea.
- Digoxin was first approved by the FDA in 1954 for the treatment of atrial flutter (Aflutter), atrial fibrillation (Afib) and heart failure (HF).
What kind of patients are on Digoxin?
- Digoxin has shown beneficial effects on patients with heart failure with reduced ejected fraction, usually <40% (Fu 2020)
- It has also been used for rate control in AFib and Aflutter that is refractory to traditional medication
Pathogenesis of Digoxin Toxicity (Smith 1988 , David 2020 ):
-
- Digoxin has a narrow therapeutic index
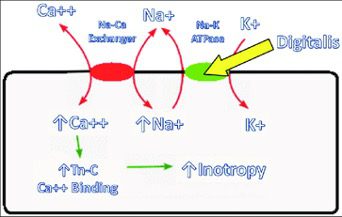
- Primarily works on the Na+/K+ pump of the cardiac myocyte
- Digoxin inhibits the Na+/K+ pump
- Leads to an increased Intracellular Na+ and decreased Intracellular K+
- It is the Na+/K+ in the skeletal muscles that cause hyperkalemia (Kashani 2005) as skeletal muscle is the largest reservoir for potassium in the body
- Increased intracellular Na+ prevents the Na+/Ca2+ channel leading to increased intracellular Ca2+
- Intracellular calcium within the cardiac myocytes results in increased inotropy
- This will cause increased irritability of cardiac myocytes leading to tachy/brady dysrhythmias (Smith 1988, Ershad 2020)
Factors Contributing to Digoxin Toxicity (Gheorghiade 2004):
-
- Increased drug in the body
- Intentional/Unintentional overdose
- Ingestion of plants or animals containing cardiac glycosides
- Digitalis, foxglove, red quill, lily of the valley, oleander, yellow oleander, pong pong, cerbera manghas, dogbane, aconite, bufo toads, Colorado river toad
- Decreased elimination
- Renal insufficiency: prolongs the half-life and increases volume of distribution
- Metabolic disturbances
- Hypokalemia: can sensitize myocardium to digoxin, diuretics
- Hypomagnesemia: can sensitize myocardium to digoxin and increases activity of cardiac glycosides
- Hypernatremia
- Hypercalcemia: predisposes patient to toxicity
- Acid-base disturbance: can cause electrolytes changes
- Polypharmacy: Diuretics, medication that affects the renal function
- Increased drug in the body
Serum Levels (Heart Failure Society of America 2010):
-
- Ideal therapeutic levels should be maintained between 0.8-2.0 ng/ml
- May take up to 7 days to reach steady state (Oncu 2018)
- Consider toxicity when levels start approaching >2 ng/ml
- Ideal therapeutic levels should be maintained between 0.8-2.0 ng/ml
Acute Symptomatology:
-
-
- GI: Nausea and vomiting usually in the first 2-4 hours
- CNS: Lethargy and confusion
- Cardiac: AV blocks, PVCs, Bradydysrhythmias, ventricular arrythmias
- Hyperkalemia
-
Chronic Symptomatology:
-
-
- Features are similar to acute intoxication
- Visual disturbances: green-yellow visual disturbances
- Low K+ levels may be secondary to concomitant use of diuretics (Kashani 2005)
-
ECG features demonstrating Digoxin Effect
-
-
- Shortened Atrial and Ventricular refractory periods leading to ECG morphology
- A classic ECG sign in digoxin effect is an ST segment depression in a concave manner (Ma 2001)
- Scooped ST (Dali) or Hockey stick
- Digoxin Effect does not imply Digoxin Toxicity
-
ECG features in Digoxin Toxicity:
-
-
- Digoxin can cause a large variety of EKG abnormalities (Richter 2009)
- PVCs is the most common arrythmia (Kashani 2005)
- Biphasic T wave: a prominent U followed by a flattened T
- Shortened QT interval
- Sinus Bradycardia
- Slow Afib (not Afib with RVR)
- AV blocks
-
- Digoxin primarily affects the level of the AV node, decreasing conduction there and increasing the refractory period
- With higher concentrations, Type I AV blocks may progress to a Type II Mobitz I pattern
- Mobitz II is highly unlikely to occur as it originates below the AV node
- A higher degree AV block in AFib will produce a junctional rhythm which can produce a regularized R-R pattern leading to a regular AFib pattern (figure 4).
-
- Ventricular Tachycardia
-
-
- Impulses from the lower AV node will go down the left and right bundle branches leading to a Bidirectional Ventricular Tachycardia (Richter 2009) (figure 5).
-
-
-
Management of digoxin toxicity:
- Acute
-
- ECG, cardiac monitor, IV access
- BMP and Serum Digoxin level
- Evaluate for elevated digoxin levels in acute toxicity
- For acute ingestions obtain levels on presentation and 6 hours after known ingestion
- Evaluate for hyperkalemia in acute toxicity as there is correlation with severity
- Evaluate for elevated digoxin levels in acute toxicity
- Digibind is your treatment of choice in hyperkalemia in the setting of Digoxin Toxicity
- If hyperkalemia is present treat with Insulin, albuterol, and Calcium or follow your institution’s hyperkalemia protocol
- These are temporizing measures at best
- Theoretical idea of stone heart has been disproven (Levine, 2011)
- Evaluate for life threatening arrythmias
- Give antidote if indicated
Indications for antidote (Ershad 2020):
-
-
- Any life-threatening digoxin related dysrhythmia
- Refractory hyperkalemia
- Digoxin level >15 at any time
- Digoxin level >10, 6 hours following ingestion
- Acute ingestion of >10mg in adults
- Acute ingestion of >4mg (>0.1 mg/kg) in peds
- Chronic elevation of digoxin concentration with AMS, cardiac dysrhythmia, or severe GI symptoms
- Do not wait for digoxin level if clinical presentation of digoxin toxicity is the likely cause
- Consider Atropine 0.5 mg IV in bradydysrhythmia or high degree AV block
- Transvenous pacer wires may cause myocardial irritability (Kashani 2005)
- ECMO
- Not well studied, not indicated for removal of digoxin (Mowry 2015)
-
- Chronic
- Serum digoxin Level can be misleading
- It does not have to be >2 to have toxic effects
- Patients may be symptomatic at therapeutic levels
- Check Electrolyte levels
- Potassium may be low secondary to concomitant use of diuretics which can potentiate toxic effect
- Replete magnesium levels as hypomagnesemia can potentiate digoxin toxicity
- Always check renal function
- Give antidote if indicated
- Consult your local poison control
- Activated charcoal is an adjunctive treatment. Consider if known ingestion time was < 1hr ago
- 1g/kg to a max of 50g
Contraindications for antidote:
-
-
- No absolute contraindications
- Caution in:
- Sinus node disease
- Patients with WPW as it could increase anterograde conduction leading to ventricular fibrillation
- ESRD
- Known hypersensitivity to digoxin or other digitalis derived products
-
Antidote (Digibind) Equation (Pincus 2016):
- Each vial contains 38 mg of antidote (Digibind) which will bind to 50 mcg of digoxin (Ershad 2020)
-
- If the quantity is known but not the dose
- number of vials required = 1.6 x (Ingested dose in milligrams)
- If the level of digoxin is known
- Number of vials required = (Serum Digoxin Level) x (Weight in kilograms)/100
- Pediatrics dose is 5 vials
- Acute ingestion
- 5 vials if patient is hemodynamically stable
- 10 vials if patient hemodynamically unstable
- 20 vials if patient is cardiac arrest
- Chronic ingestion
- If the quantity is known but not the dose
- Adults 3-6 vials
- Pediatrics 1-2 vials
- Pregnancy
- It is acceptable to give in pregnancy when necessary (pregnancy category C)
- Pregnancy
-
Take Home Points
- Although the overall prevalence of digoxin toxicity seems to be decreasing, one must think of this toxicity when facing a patient with bradycardia and “something else”
- Obtain a 12 lead EKG, serum electrolytes and serum digoxin level initially
- Digoxin toxicity may mimic several different EKG patterns
- “Scooped” ST segments signify that the patient is taking digoxin (“dig effect”) and is not an indication of digoxin toxicity
- Simple doses to remember for Digibind
- 5 vials in hemodynamically stable patients
- 10 vials in unstable patients
- 20 vials in the setting of cardiac arrest
- Of note: consult your pharmacy to see how many vials are available at your local hospital
Authors:
- Santiago Lopez, MD PGY3 , Good Samaritan Hospital
- Katrina D’Amore, DO, Good Samaritan Hospital
- John Kashani DO, FACMT, St. Joseph’s University Medical Center
Post Peer Reviewed By: Anand Swaminathan, MD (@EMSwami) and Salim R. Rezaie, MD (Twitter: @srrezaie)
The post Management of Digoxin Toxicity appeared first on REBEL EM - Emergency Medicine Blog.
