
- Antibiotics reduce symptomology
- Antibiotics reduce the rate of suppurative complications
- Antibiotics reduce the rate of non-suppurative complications (primarily Rheumatic Heart Disease).
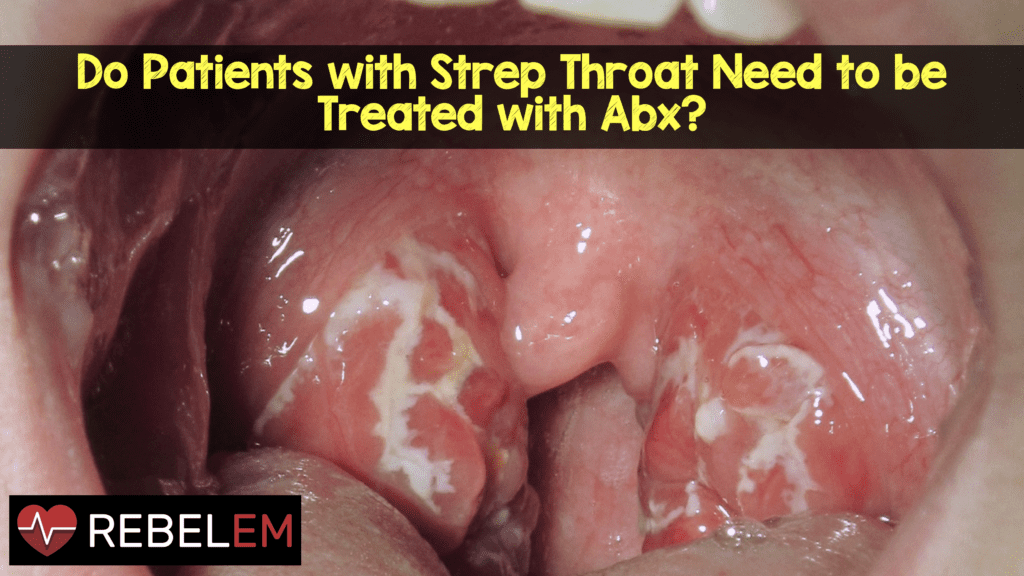
So, do patients with strep throat need to be treated with antibiotics?
While treatment of strep throat seems relatively benign, there are significant harms that need to be considered:
- 1 in 10 patients will develop antibiotic associated diarrhea (some of these will be C. diff)
- Severe allergic reactions occur in 0.24% of patients
This means that out of 10 million patients treated with antibiotics, as many as 24,000 of them will have fatal or near-fatal allergic reactions.
Thus, it’s important to determine if the benefits of antibiotic treatment outweigh the risks.
Argument #1: Antibiotics reduce symptomology
The most important thing to recognize is that in the vast majority of patients, strep throat is a self limited disease that will get better in about 7 days with no treatment (this includes supportive care). The addition of antibiotics provides a modest benefit in terms of symptomology resolution (12-16 hours) (Del Mar 2006). This benefit, however, is in comparison to placebo, which is not standard care. Supportive therapies including acetaminophen and NSAIDs may affect symptom improvement but there are no good studies on this. Finally, we must not forget about the potential additional side effects associated with antibiotics (i.e. diarrhea).
One therapy that has shown remarkable benefits in terms of symptoms is the use of corticosteroids. Hayward et al showed that corticosteroids increased the rate of symptom resolution at 24 hours with an NNT = 4 (Hayward 2012).
Bottom Line: If we are interested in making the patient’s symptoms resolve faster, corticosteroids are our best bet. I typically give 10 mg of decadron IM.
Argument #2: Antibiotics reduce the rate of suppurative complications.
There are a number of potential complications associated with strep throat including acute otitis media (AOM), sinusitis and peritonsilar abscess (PTA).
| Yeh 2005 | Del Mar 2006 | |
| AOM | NNT = 25 | NNT > 200 |
| Sinusitis | NNT = infinity | Not Reported |
| PTA | NNT = 28 | NNT = 55 – 225 |
A more recent study demonstrated an overall suppurative complication rate of 1.3% and no difference in patients who received antibiotics versus those that did not (Little 2013).
Bottom Line: It appears that we would have to treat 100’s of patients to prevent one PTA; an easily treatable entity.
Argument #3: Antibiotics reduce the rate of non-suppurative complications.
The two major non-suppurative complications are: Post-strep Glomerulonephritis (PSGN) and rheumatic fever (RF). No study has ever shown that PSGN can be prevented and so, we are left with RF.
However, we must ask the question of whether these studies apply to our patients today. The rate of RHD in the westernized world is exquisitely low. In fact, the CDC stopped tracking the incidence in 1995 when it fell below 1 per million. Numerous RCTs in
developed countries have shown no cases of RF or RHD in patients treated with placebo (Middleton 1988, De Meyere 1992, Dagnelie 1996, Little 1997, Zwart 2003).
Based on the current incidence of RF in the US, we would need to treat about 2 million patients with strep throat in order to prevent a single case of RF. In addition, only 1 out of every 3 patients who develops RF will subsequently develop RHD. Treating millions of patients with pharyngitis in the pursuit prevention of single digit cases of RHD in the western world makes no sense.
Many physicians argue that the reason for the decline in RF and RHD is because we treat every patient with pharyngitis for strep. However,epidemiologic data speaks against this. The incidence of streptococcal diseases fell long before the advent of antibiotics but fell concurrently with improvements in public health. It is a far more likely scenario that improvements in sanitation have led to shifts in the serotype of Group A beta-hemolytic streptococcus that causes strep throat in developed countries.
Clinical Bottom Line:
We are far more likely to harm patients with strep pharyngitis by giving antibiotics than to help them in developed countries. This does not apply to developing countries with poor public health (See this post from Casey Parker about treatment in developing areas).
Finally, let’s see what one of the core texts in EM has to say on the topic:
“acute pharyngitis should not typically be treated with antibiotics. The great majority of cases are viral in origin, and suppurative complications following streptococcal infection are both easily treated and too rare to justify routine use of antibiotics. In particular, antibiotics were beneficial in reducing rheumatic fever only during a single military epidemic in the mid-twentieth century, and the decline of rheumatic fever is unrelated to trends in antibiotic use.” (Rosen’s 2014)
Related Posts
- Newman D. Treatment of Acute Pharyngitis. SMART EM.
- Washington University EM: Antibiotics for Strep Pharyngitis – The Pediatric Perspective
- Edmund Kwok at CanadiEM: The (Real) Battle Against Strep Throat
Bibliography
- Barnett, ML, Linder JA. Antibiotics prescribing to adults with sore throat in the United States, 1997-2010 Research Letter. JAMA Int Med 2013; 174(1): 138-40. PMID: 24091806
- Del Mar CB, Glasziou PP, Spinks AB. Should sore throats be treated with antibiotics? (Review). Cochrane Database of Systematic Reviews 2006 Issue 4. CD000023 PMID: 15106140
- Hayward G et al. Corticosteroids as standalone or add-on treatment for sore-throat (Review). Cochrane Database Syst Rev 2012. CD 008268 PMID: 23076943
- Yeh B., Eskin B. Should Sore Throats Be Treated with Antibiotics? Ann of EM 2005; 45: 82-4. PMID: 15635315
- Little P et al. Predictors of suppurative complications for acute sore throat in primary care: prospective clinical cohort study. BMJ 2013; 347: f6867. PMID: 24277339
- Denny FW, Wannamaker LW, Brink WR. Prevention of rheumatic fever. Treatment of the preceding streptococcic infection. JAMA. 1950;143(2):151-3. PMID: 15415234
- Wannamaker LW et al. Prophylaxis of acute rheumatic fever by treatment of the preceding streptococcal infection with various amounts of depot penicillin. Am J Med. 1951;10:673-94. PMID: 14837911
- Chamovitz R et al. Prevention of rheumatic fever by treatment of previous streptococcal infection. NEJM, 1954. 251: p. 466-71. PMID: 13194096
- Siegel EE, Stollerman GH. Controlled studies of streptococcal pharyngitis in a pediatric population. NEJM. 1961;265:559-65. DOI: 10.1056/NEJM196109212651202
- Middleton DB et al. Standardized symptomatic treatment versus penicillin as initial therapy for streptococcal pharyngitis. Ped Rheum Ther 1988; 113: 1089-94. PMID: 3057159
- De Meyere M et al. Effect of Penicillin on the clinical course of streptococcal pharyngitis in general practice. Eur J Clin Pharmacol 1992; 43: 581-5. PMID: 1493837
- Dagnelie CF et al. Do patients with sore throat benefit from penicillin? A randomized double-blind placebo controlled clinical trial with penicillin V in general practice. Brit J Gen Pract 1996; 46: 589-93. PMID: 8945796
- Little P et al. Reattendance and complications in a randomised trial of prescribing strategies for sore throat: the medicalising effect of prescribing antibiotics. BMJ 1997; 315(7104): 350-2. PMID: 9270458
- Zwart S et al. Penicillin for acute sore throat in children: randomised, double blind trial. BMJ 2003; 327(7427): 1324-8. PMID: 14658641
The post Do Patients with Strep Throat Need to Be Treated with Antibiotics? appeared first on REBEL EM - Emergency Medicine Blog.
