

Salim R. Rezaie, MD
Blog: REBEL EM
Podcast: REBEL Cast
Twitter: @srrezaie
Facebook: REBEL EM
Instagram: rebelem2013
Study Summaries:
- Submassive PE is a Spectrum of Disease [1]: The original PEITHO randomized clinical trial showed a 3 fold decrease in hemodynamic compromise, but at the expense of a 5 fold increase in extracranial hemorrhage and a 10 fold increase in intracranial hemorrhage in submassive PE patients receiving thrombolysis. In the 2 – 3 year follow up study we saw no difference in long term mortality, but unfortunately the conclusion of this trial should have been that thrombolysis did not improve long term mortality in an undifferentiated population of patients with submassive PE. Thrombolysis in submassive PE should only be considered in patients with signs of submassive PE and who appear to be at the brink of massive PE (pale, diaphoretic, tachycardia = “sick”).
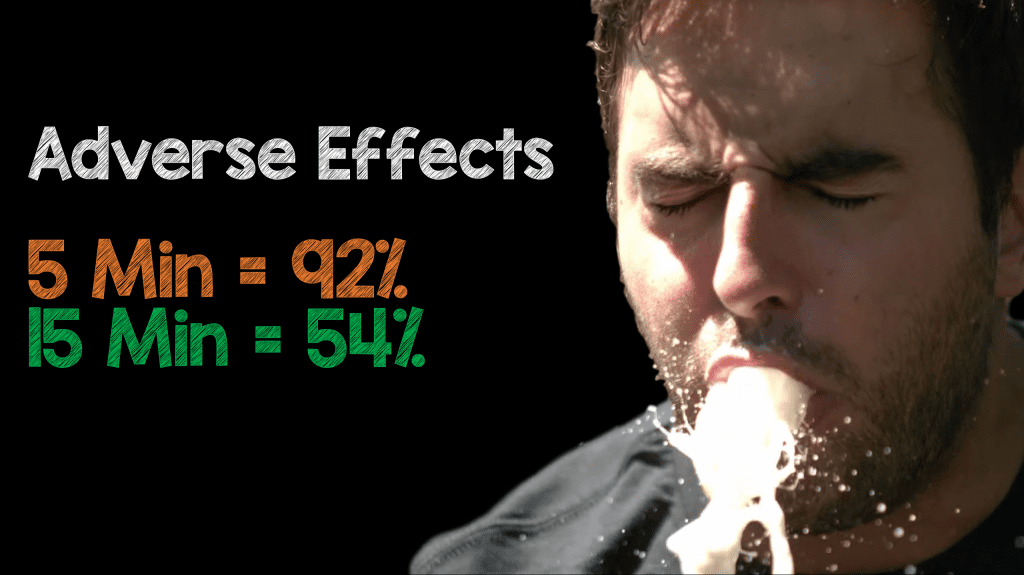
- Low Dose Ketamine Infusion for Pain Control [2]: Low dose ketamine of 0.3mg/kg, mixed into 100mL of Normal Saline given over slow infusion (15 minutes) has a decreased side effect profile (i.e hallucinations or dizziness) and equal analgesic profile when compared to IV push (5 minutes) low dose ketamine.
- Dosing of Ketorolac [3]: In this single center RCT of 240 patients, 10 – 15 mg of ketorolac IV is equivalent to 30 mg of ketorolac IV for acute pain in the ED with the potential for less side effects (i.e. renal toxicity). Additionally, there was no difference in the need for rescue analgesia between groups.
- Consider Haloperidol in Gastroparesis [4]: To be fair this was a retrospective study of 52 patients with diabetic gastroparesis, not exactly the highest level of evidence on the EBM pyramid. However, 5mg IV or IM Haldol helped decrease rates of admission and amounts of opioids administered in patients with diabetic gastroparesis. There were zero cases of dystonia, akathisia, excessive sedation, or cardiovascular complications.
- PERC Decreases Imaging [5]: This is the first RCT comparing usual care to PERC + usual care. In this non-inferiority trial of ≈2000 patients, in a “low risk” patient population, use of PERC over usual care, was non-inferior in both diagnosis and mortality associated with PE. An added benefit of using PERC is a 10% decrease in imaging and 40min decrease in ED LOS.
- Steroids Reverse Shock Faster in Sepsis [6]: This is the largest RCT looking at 3800 patients with septic shock. In patients with septic shock, admitted to the ICU on mechanical ventilation and requiring ≥4 hours of vasopressors/inotropes, hydrocortisone infusion (200mg/d) compared to placebo, does not make a difference in 90 day mortality, however there were some improved secondary outcomes including: shock reversal, ventilator free days, and LOS in the ICU
- Octreotide Improves Clinically Important Outcomes in Undifferentiated UGIB [8]: The best evidence to support the use of octreotide in undifferentiated upper GIB comes from a meta-analysis published in 1997. Only two trials including ≈300 patients compared octreotide alone to placebo. Octreotide in undifferentiated UGIB reduced bleeding (NNT = 16) and need for surgery (NNT = 67). We don’t have outcomes for mortality
- Post Contrast AKI NOT Contrast Induced Nephropathy: This was a systematic review and meta-analysis of contrast enhanced vs non-contrast enhanced CTs including 28 studies with > 107,000 patients. Unfortunately, there were no RCTs included in this analysis as none exist. While a prospective, multi center RCT would put this question of acute kidney injury after IV contrast to rest, it’s unlikely to be feasible to perform. Based on the best available evidence, use of IV low- and iso-osmolar contrast media does not appear to be associated with increased risk of AKI, need for renal replacement therapy, or mortality. Early contrast agents used mono-iodinated rings and ionic monomers making hyperosmolor solutions (1500mOsm) relative to serum, which is a severe irritant and more likely to cause vasodilation, increased capillary permeability, mast cell degranulation, and AKI. Newer agents are lower and iso-osmalr (290 – 800mOsm) using di- and try-iodinated rings with non-ionic monomers (90 – 95% of contrast used in the US), and much less likely to be an irritant or causing AKI. Many studies fail to account for patients’ other risk factors for development of acute kidney injury, including sepsis, dehydration, end-organ dysfunction, or administration of nephrotoxic medications.
- There is Nothing NORMAL About Normal Saline [9]: The SALT-ED (Non-Critically Ill) and SMART (Critically Ill) RCTs were single center studies with >13,000 patients each. In the SALT-ED trial compared Normal Saline was compared to Lactated Ringers (>95% of balanced fluids used) in non-critically ill patients. There was no difference in their primary outcome of median number of hospital free days, but there was a difference in MAKE 30 (Major Adverse Kidney Events at 30 Days), which was defined as a composite outcome of doubling of creatinine, new art, and death (NNT = 111). The composite outcome of this study was driven by doubling of creatinine not new RRT or death. In the subset of patients with baseline serum creatinine ≥1.5mg/dL and serum Cl ≥110, there appeared to be the largest benefit of using balanced crystalloids over normal saline for avoiding MAKE30 and AKI. The SMART trial was a single center study of >15,000 patients comparing normal saline to balanced crystalloid (Plasma-Late and LR). The primary outcome of MAKE30 was reduced with balanced crystalloids with a NNT = 91. In the subset of patients with sepsis, is where the biggest difference was seen with a decrease in 30d mortality (NNT = 24) and MAKE30 (NNT = 20). In this trial the composite outcome of MAKE30 was driven by a mortality reduction not doubling of creatinine or new RRT. We now have the strongest evidence to date supporting the use of balanced crystalloids over normal saline in both critically ill and non-critically ill patients admitted to the hospital requiring > 1 – 2 liters.
- There is Still a Role for ApOx in the ED [10]: This is the first RCT of apneic oxygenation (AO) in the ED (200 patients randomized to AO vs no AO). The authors found that in patients who receive proper pre-oxygenation (3min with flush 100% O2), apneic oxygenation may be a superfluous intervention, however it is important to remember that AO is not a complicated procedure, it’s inexpensive, and has not been shown to be harmful. Additionally, the absence of benefit (Most intubations were completed by 100 seconds) here doesn’t mean there is no group who won’t benefit (i.e. prolonged apnea times and crash intubations) but, it is nearly impossible to make accurate prospective predictions as to which patients will benefit the most.
- Femoral Nerve Blocks Improve Outcomes in Geriatric Hip Fractures [7]: This was a randomized trial of ≈160 patients, over the age of 60 with hp fractures. Patients were randomized to usual pain control with IV opioids vs femoral nerve blocks (20mL of 0.5% bupivacaine + continuous fascia Iliaca Block with 15mL of 0.2% ropivacaine followed by a continuous infusion of 02% ropivacaine at 5mLhr through post operative day 3). In patients 60 years of age or older, presenting to the ED with hip fractures, femoral nerve blocks with 20mL of 0.5% bupivacaine not only improved pain, but also increase mobility and functional outcomes with significantly less medication side effects when compared to IV opioid agents
References:
- PEITHO Long-Term Follow Up Trial: Konstantinides SV et al. Impact of Thrombolytic Therapy on the Long-Term Outcome of Intermediate-Risk Pulmonary Embolism. J Am Coll Cardiol 2017. PMID: 2833583
- REBEL EM Critical Appraisal: Episode 38 – Do All Submassive PE’s Require Treatment with Thrombolysis?
2. Ketamine Infusion for Pain: Motov S et al. A Prospective Randomized, Double-Dummy Trial Comparing Intravenous Push Dose of Low Dose Ketamine to Short Infusion of Low Dose Ketamine for Treatment of Moderate to Severe Pain in the Emergency Department. Am J Emerg Med 2017. PMID: 28283340
- REBEL EM Critical Appraisal: Low-Dose Ketamine for Acute Pain in the ED – IV Push vs Short Infusion?
3. Ketorolac Dosing: Motov S et al. Comparison of Intravenous Ketorolac at Three Single-Dose Regimens for Treating Acute Pain in the Emergency Department: A Randomized Controlled Trial. Ann Emerg Med 2017. PMID: 27993418
- REBEL EM Critical Appraisal: The Ketorolac Analgesic Ceiling
4. Gastroparesis Treatment: Ramirez R et al. Haloperidol Undermining Gastroparesis Symptoms (HUGS) in the Emergency Department. Am J Emerg Med 2017. PMID: 28320545
- REBEL EM Critical Appraisal: Diabetic Gastroparesis Needs HUGS
5. PERC RCT: Feund Y et al. Effect of the Pulmonary Embolism Rule-Out Criteria on Subsequent Thromboembolic Events Among Low-Risk Emergency Department Patients: The PROPER Randomized Clinical Trial. JAMA 2018.PMID: 29450523
- REBEL EM Critical Appraisal: Is it PROPER to PERC it Up?
6. Steroids in Sepsis: Venkatesh B et al. Adjunctive Glucocorticoid Therapy in Patients with Septic Shock. NEJM 2018. [NEJM Link HERE]
- REBEL EM Critical Appraisal: The ADRENAL Trial – Steroids in Septic Shock
7. Regional Nerve Blocks for Hip Fractures:Morrison RS et al. Regional Nerve Blocks Improve Pain and Functional Outcomes in Hip Fracture: A Randomized Controlled Trial. J Am Geriatr Soc 2016. PMID: 27787895
- REBEL EM Critical Appraisal: REBEL Cast Ep 43 – Pain control and Opioid Sparing Options in the ED
8. Octreotide in Undifferentiated UGIB:Thomas F et al. Somatostatin or Octreotide Compared with H2 Antagonists and Placebo in the Management of Acute Non-Variceal Upper GI Hemorrhage: A Meta-Analysis. Ann Intern Med 1997. PMID: 9412308
9. Balanced vs Unbalanced Crystalloids In Critically Ill:Semler MW et al. Balanced Crystalloids Versus Saline in Critically Ill Adults (SMART). NEJM 2018. [NEJM Link HERE]
- REBEL EM Critical Appraisal: Is the Great Debate Between Balanced vs Unbalanced Crystalloids Finally Over?
- Balanced vs Unbalanced Crystalloids in Non-Critically Ill:Self WH et al. Balanced Crystalloids Versus Saline in Noncritically Ill Adults (SALT-ED). NEJM 2018. [NEJM Link HERE]
- REBEL EM Critical Appraisal: Is the Great Debate Between Balanced vs Unbalanced Crystalloids Finally Over?
10. RCT of Apneic Oxygenation in the ED:Caputo N et al. emergency Department use of Apneic Oxygenation Versus Usual Care During Rapid Sequence Intubation: A Randomized Controlled Trial (ENDAO). Acad Emerg Med 2017. PMID: 28791755
- REBEL EM Critical Appraisal: The ENDAO Trial – Is Apneic Oxygenation a Futile Intervention in ED RSI?
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post Keeping Up in EM at Cook County Grand Rounds appeared first on REBEL EM - Emergency Medicine Blog.
