

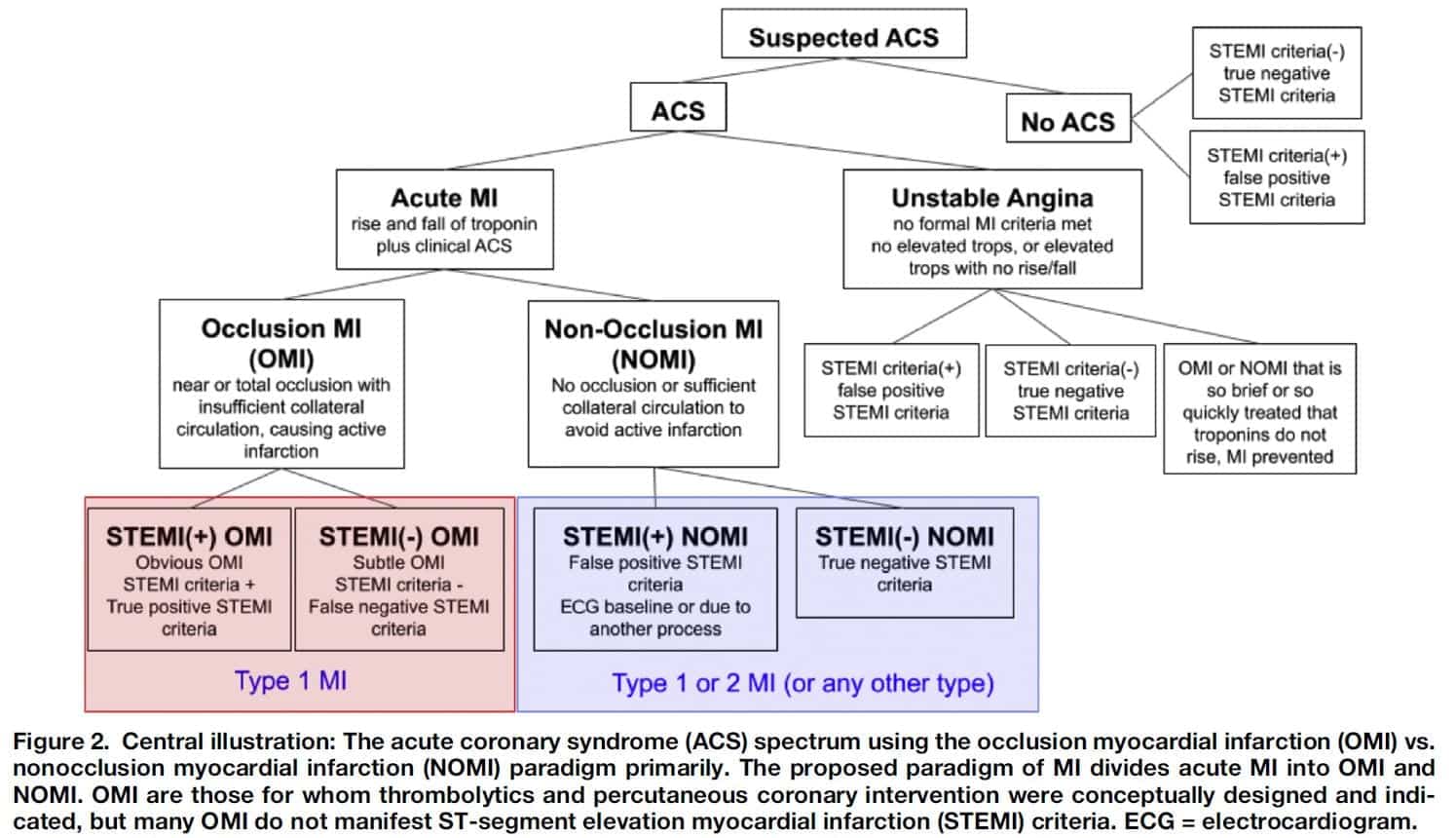
In the Reperfusion Era of the late 20th century, many large trials showed the benefits of emergent reperfusion therapy, with even greater benefit in the subgroup of patients with undefined ST elevation. As the best idea available, the STEMI-NSTEMI paradigm replaced the Q-wave vs. non-Q-wave MI paradigm in 2000. STEMI-NSTEMI has been a primary determinant of cath lab activations, hospital metrics, and many other patient factors and outcomes. However, the STEMI criteria fail us frequently, missing upwards of 30% of acute coronary occlusion. Additionally, the STEMI/NSTEMI paradigm is dependent on ST segment elevation defined by millimeter criteria, however many occlusion myocardial infarctions (OMI), have no ST segment elevation at all. To many of us, this idea is not new; we are often taught about STEMI equivalents and “subtle STEMI” that also deserve aggressive management.
Over the last 15 years, there has been increased interest in identifying which patients would benefit most from emergent reperfusion therapy. Occlusion myocardial infarction (OMI) vs non-occlusion myocardial infarction (NOMI) is a new paradigm that emerged a few years ago (courtesy of Dr. Stephen Smith, Dr. Pendell Myers, and Dr. Scott Weingart) that might change the way we think about acute myocardial infarction. Their OMI Manifesto is an incredible document (which I highly recommend you read) outlining the historical, clinical, and academic perspectives of why the STEMI-NSTEMI paradigm should be replaced by the OMI-NOMI paradigm. OMI is defined as acute coronary occlusion or near occlusion with insufficient collateral circulation where without emergent catheterization and reperfusion myocardium will undergo necrosis. Patients with OMI are the only ones who benefit from emergent reperfusion therapy, and these patients can present with or without ST elevation on ECG.
Paper: Myers HP et al. Comparison of the ST-Elevation Myocardial Infarction (STEMI) vs. NSTEMI and Occlusion MI (OMI) vs. NOMI Paradigms of Acute MI. Journal of Emergency Medicine 2020. PMID: 33308915 .2
Clinical Question: What differences exist between STEMI(+) OMI patients and STEMI(-) OMI patients in terms of time to catheterization and outcomes?
What They Did:
Study Design:
- Retrospective review of prospectively collected data exploring the differences between two classification systems: STEMI(+) OMI and STEMI(-) OMI
- Substudy of the Diagnosis of Occlusion MI and Reperfusion by Interpretation of the Electrocardiogram in Acute Thrombotic Occlusion (DOMI ARIGATO)
Population:
- Consecutive patients presenting with possible ACS at a suburban, academic hospital
- Two databases
- All consecutive patients admitted to cardiology with possible ACS and scheduled for urgent or emergent cardiac catheterization
- All consecutive patients for whom the cardiology interventionalist is called for ED consultation of possible emergent PCI
- 6 month period during 2017
- Patients without an ECG in the EMR were excluded
Intervention:
- Charts were reviewed by 4 EM residents with training from primary and senior authors
- Collected and managed data using REDCap site
- One blinded investigator reviewed all available transfer, prehospital, and the first pre-cath study site ECG for the presence of formal STEMI criteria according to fourth universal definition of MI 3
- Diagnosis of OMI vs NOMI was determined by angiography (“confirmed OMI”) or “presumed OMI with significant cardiac outcome” as defined by:
- Angiogram showing acute but nonocclusive culprit lesion with highly elevated biomarkers
- Highly elevated biomarkers and new or assumed new regional wall motion abnormality on echo
- ECG positive for STEMI with death before emergent cath
Outcomes:
- Primary outcomes:
- Infarct size (as estimated by peak troponin)
- Time from presentation to cardiac cath
- Exploratory analyses on the presence of wall motion abnormalities, medication administration, and adverse outcomes between groups
Results:
- 467 unique patient encounters
- 234 patients had AMI present (50.1%)
- 108 patients met OMI criteria (23.1%)
- 67 STEMI(+)
- 41 STEMI(-) – 38% of all OMIs
- Peak Troponin T values
- STEMI(+) OMI: 5.36ng/mL
- STEMI(-) OMI: 4.44ng/mL
- No occlusion: 0.12ng/mL
- *P<0.001 for both STEMI(+) OMI and STEMI(-) OMI compared to no occlusion
- *P=0.021 between STEMI(+) OMI and STEMI(-) OMI
- Angiographic outcomes
- Of the STEMI(+) OMI patients: 82% had TIMI 0-2, 18% had TIMI 3 but with highly elevated biomarkers (one of the “presumed OMI” criteria)
- Of the STEMI(-) OMI patients: 71% had TIMI 0-2, 27% had TIMI 3 but with highly elevated biomarkers (one of the “presumed OMI” criteria)
- Interventions
- 67 of 67 patients in STEMI(+) OMI and 40 of 41 STEMI(-) OMI had cath performed during the index hospitalization
- Median time from arrival to cath lab:
- STEMI(+) OMI: 41 min (Range: 23 to 86min)
- STEMI(-) OMI: 437 min (Range: 85 to 1590min)
- STEMI(+) was more likely to undergo cath in less than 90 min (76% vs 28%; *p<0.001)
- Similar rates of new or presumed new wall motion abnormality: 86% vs 75%, p=0.19
- Number of potential regional wall motion abnormalities: 2.76 vs 2.29
- Number of potential regional wall motion abnormalities in NOMI group: 0.62
- Similar rates of cardiac arrest prior to catheterization: 10.4% vs 9.8%
- 13 patients suffered in-hospital mortality
- 4 STEMI(+) OMI
- 1 STEMI(-) OMI
- 8 no occlusion
- Composite outcome of cardiac arrest, in-hospital mortality, or survival with discharge to hospice
- 18% STEMI(+) OMI
- 15% STEMI(-) OMI
- 6% no occlusion
*considered statistically significant by the authors
Strengths:
- Prospectively collected data of consecutive patients
- ECG reviewer was blinded to the outcomes
- All cases meeting OMI criteria were reviewed for the presence of STEMI criteria by a cardiology fellow also blinded to the outcome and the study goals (This is important as ED physician may be biased to call STEMI(-) OMI in borderline cases, but having a cardiologist review the cases showed that more cases of STEMI(-) OMI were identified by cardiology)
- 87% agreement between two reviewers (k = 0.735; 95% CI 0.607 to 0.863)
- Used a quantifiable primary objective (troponin elevation) that has been linked to infarct size in multiple studies
- Appears to be a pretty typical representative cardiac population: Obesity 49.3%, HTN 72.6%, HLD 61.2%, Diabetes Type 2 34.7%, Known CAD 45.4%
- The more conservative ECG reader’s classifications were used (67 out of 108 cases vs 59 out of 108 cases)
- STEMI(+) OMI rate matches that of a recent large, prospective study by a separate author group5
- Inclusion criteria provided a high-risk cohort of suspected ACS patients
Limitations:
- Relatively small, single-center study; limits generalizability
- Retrospective chart review looking at final diagnosis of AMI from the medical record which means patients could have been missed if ACS unrecognized
- Few deaths making it difficult to draw conclusions on mortality
- Analysis limited to surrogate markers (troponin T elevation) of patient-centered outcomes (congestive heart failure, mortality, etc…)
- Of the 612 subjects that were initially identified, 85 were excluded prior to chart review: nearly 14%
- Unable to obtain follow-up data beyond the index visit
- Diagnosis of AMI was collected from the final diagnosis in the medical record, which would have led to misclassifications.
Discussion:
- This is the beginning of a new era in reperfusion therapy! For years, we have relied on the STEMI-NSTEMI paradigm to make decisions for complex patient presentations. Cardiologists and emergency physicians clashed over which patients to take to the cath lab. With a name that rolls off the tongue and promises action and excitement, the term “STEMI” is a cognitive roadblock that prevents us from looking for other signs of occlusion MI. We are starting to find emerging data that shows we are consistently missing a subset of occluded coronary arteries. This was first covered on RebelEM in this post about the DIFOCCULT Trial .
- In a large 2009 trial4, NSTEMI patients were randomized to early vs. routine cardiac cath. The investigators found no difference in composite outcome of death, MI, or stroke at 6 months; however, the median time to cath lab in the early group was 16 hours (not really early…) and sicker patients (GRACE score >140) benefitted more from early cath. Furthermore, the composite secondary outcome of death, myocardial infarction, or refractory ischemia was improved in the early intervention group. Other studies also corroborate that early intervention is associated with better outcomes.
- This image from Myers paper says it all:
- In this study, STEMI(-) OMIs appeared to be similar to STEMI(+) OMIs in terms of highly elevated troponins, higher likelihood of and higher mean number of, wall motion abnormalities. However, their time to catheterization was significantly longer. What could have been their outcomes had there been less delay, or even no delay? The STEMI(-) OMI patients could have had better outcomes compared to the STEMI(+) OMI patients if they had cardiac cath sooner.
- Multiple studies have shown that NSTEMI patients have higher long-term mortality than STEMI patients. It is challenging to determine exactly why this is the case, but this is a population in which we have room for improvement. By classifying acute MI patients in a new paradigm, perhaps we can better identify who is at greater risk.
- The results of this study are only hypothesis generating; further studies are needed to recommend practice changes.
Author Conclusions:
“STEMI(-) OMI patients had significant delays to catheterization but adverse outcomes more similar to STEMI(+) OMI than those with no occlusion. these data support the OMI/NOMI paradigm and the importance of further research into emergent repercussion for STEMI(-) OMI.”
Clinical Take Home Point:
The STEMI-NSTEMI paradigm still misses a significant number of acute coronary occlusion events that could benefit from emergent invasive intervention and a new model could improve our ability to identify them more accurately. Additionally, the OMI-NOMI paradigm would move us away from depending solely on ST elevation millimeter criteria for rapid treatment.
These results support that OMI-NOMI (rather than STEMI-NSTEMI) criteria can identify more patients with ACS that have emergently salvageable myocardium that would benefit from emergent invasive intervention and at the same time identify patients where emergent invasive intervention is of minimal benefit. STEMI(-) OMI are an under identified subgroup of ACS patients and this is now the second paper published that really helps push the needle to a OMI-NOMI paradigm shift.
References:
- Meyers HP, Weingart SD, Smith SW. The OMI Manifesto. Dr. Smith’s ECG Blog 2018. Full manifesto HERE .
- Meyers HP et al. Comparison of the ST-Elevation Myocardial Infarction (STEMI) vs. NSTEMI and Occlusion MI (OMI) vs. NOMI Paradigms of Acute MI. Journal of Emergency Medicine 2020. PMID: 33308915 .
- Thygesen et al. Fourth Universal Definition of Myocardial Infarction (2018). Journal of the American College of Cardiology 2018. PMID: 30153967 .
- Mehta SR et al. Early versus delayed invasive intervention in acute coronary syndromes. NEJM 2009. PMID: 19458363 .
- Hillinger et al. Prospective Validation of Current Quantitative Electrocardiographic Criteria for ST-Elevation Myocardial Infarction. Int J Cardio 2019. PMID: 31056411
For More Thoughts on This Topic Check Out:
- Smith’s ECG Blog: Pretty much everything on Smith’s ECG Blog is important and worth a read
- LITFL: OMI – Replacing the STEMI Misnomer
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post OMI-NOMI: Time for a Paradigm Shift appeared first on REBEL EM - Emergency Medicine Blog.
