
Article: Janz DR et al. Effect of a fluid bolus on cardiovascular collapse among critically ill adults undergoing tracheal intubation (PrePARE): a randomised controlled trial. Lancet Respir Med 2019. PMID: 31585796
Clinical Question: Does administration of a fluid bolus to critically ill patients undergoing intubation reduce the risk of cardiovascular collapse?
Population: Critically ill patients > 18 years of age undergoing tracheal intubation in six medical ICUs, one trauma ICU, one neuro ICU and one emergency department.
Outcomes:
- Primary: Composite outcome of cardiovascular collapse (new SBP < 65 mm Hg, new or increased vasopressor use) between induction and 2 minutes after intubation or cardiac arrest or death within 1 hour of tracheal intubation
- Secondary: Each individual component of the composite primary outcome, any additional fluids given, lowest SBP, change in SBP, number of laryngoscopy attempts, number of vent-free days, number of ICU-free days and in-hospital mortality within 28 days.
- Safety Outcomes: lowest O2 saturation, highest fraction of inspired O2, and highest PEEP in the 24 hours after intubation, cumulative diuretic dose and cumulative IVF administration from enrollment to 3 days after enrollment
Intervention: 500 ml of 0.9% saline IV administered prior to induction of anesthesia
Design: Multi-center, randomized, unblinded trial
Excluded: Awake intubation planned, intubation could not wait for randomization, if treating clinicians felt fluid bolus was required or contraindicated for optimal care or if the patient was a prisoner or pregnant.
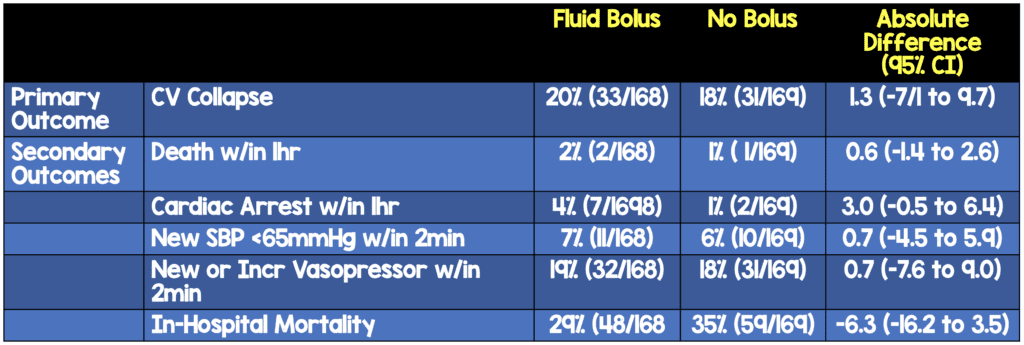
Primary Results:
-
- Enrolled: 337 out of a proposed 500 planned enrollment
- 168 randomized to fluid bolus: 165/168 received a bolus
- 167 randomized to no fluid bolus: 2/167 received a bolus
- 537 patients screened for enrollment
- Approximately 20% of patients had septic shock
- Trial was stopped early due to futility after an interim analysis
- Enrolled: 337 out of a proposed 500 planned enrollment
Critical Findings:
Strengths:
- Asks an important clinical question that has not been addressed well to date
- Funders of study had no role in conception, design, conduct of study, data collection, management, analysis, interpretation or preparation/approval of manuscript
- Protocol compliance was high: Only 1% (5/337) patients had protocol violations
- Baseline characteristics were comparable in terms of active diagnoses, indication for intubation and vasopressor use
- Minimal exclusion criteria increasing the generalizability of the findings
- Study endpoints were collected by independent observers (ICU providers) who were present in patient’s room, but did not participate in the procedure
- Agreement between independent observer and study investigator for primary outcome was 100% in a convenience sample (n = 38) of patients
Limitations:
- Primarily an ICU study (8/9 sites) and applicability to the ED setting is limited
- Primary outcome is a composite where each component is not clinically equal (death or cardiac arrest vs new SBP < 65 mm Hg)
- In a convenience sample (n = 38) of patients observed for volume of fluid infused prior to induction, the median volume of infusion was only 200 ml. thus, study may not really be assessing impact of a 500 ml fluid load\
- Incidence of primary outcome was lower than in previous studies, possibly due to 17% of patients screened being excluded
- Lower-than-planned sample size limits power to exclude an effect of a fluid bolus in patient subgroups with non-significant interactions
- The volume of IVF received prior to enrollment was not recorded, therefore it is unknown if this was balanced between groups or why there was no benefit seen with IVF
Discussion:
- Just as with any intervention, one size does not fit all. Will all patients benefit from a fluid bolus? Probably not but, there may be a subset who would benefit. Perhaps patients known to be volume depleted or those with a flat IVC on POCUS. However, those patients in which the clinician believed would benefit were excluded and this may dilute the effect
- Only one of the included sites (out of 9) was an emergency department setting. Since most patients were in the ICU, fluid status may have already been optimized decreasing the potential impact of this intervention. A future study looking at early presentation of patients would be useful,
- Only a small percentage of patients (~ 1.5%) between both groups were hemodynamically unstable as the indication for intubation. This group may not have been the optimal one to study for benefit of a fluid bolus.
- There are a number of issues regarding the IV fluids given:
- It is unclear how much fluids were administered prior to induction in the fluid bolus group. In those observed, the median was only 200 ml but the overall volume may have been less (or it may have been the same or more)
- The volume of 500mL of crystalloid might be inadequate to influence patient hemodynamics during intubation
- Timing of fluid bolus beginning before induction and infusing through induction and laryngoscopy might have produced different results
- Hypothesis generating finding in this study is patients who received positive pressure ventilation before induction (i.e. BVM or NIV) and received a fluid bolus had decreased risk of CV collapse, however patients not receiving positive pressure ventilation (i.e. HFNC, NC) and a fluid bolus appeared to increase the risk of CV collapse
Authors Conclusions:
“Administration of an intravenous fluid bolus did not decrease the overall incidence of cardiovascular collapse during tracheal intubation of critically ill adults compared with no fluid bolus in this trial.”
Our Conclusions: In this mixed etiology, primarily ICU trial, initiation of a fluid bolus did not appear to decrease the risk of cardiovascular collapse peri-intubation. However, this data is not conclusive due to methodological issues.
Potential to Impact Current Practice: Our prior understanding of the physiology of intubation and peri-intubation decompensation tells us that universal administration of a fluid bolus is unlikely to benefit patients. This study does not change this understanding.
Bottom Line: It is unlikely that universal fluid bolus administration prior to induction of anesthesia for intubation would benefit patients. However, there is likely a group that will benefit. The administration of fluids peri-intubation should continue to be based upon the clinician’s assessment of the individual patient
References:
- Jaber S, Jung B, Corne P, et al. An intervention to decrease complications related to endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Intensive Care Med 2010; 36: 248–55. PMID: 19921148
- Umobong EU, Mayo PH. Critical care airway management. Crit Care Clin 2018; 34: 313–24. PMID: 29907267
For More on This Topic Checkout:
- PulmCrit: Do Fluid Boluses Before Intubation Help? (PREPARE Trial)
- 5 Minute Airway: PREPARE Trial with Dave Janz
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post PrePARE: Effect of Fluid Bolus on CV Collapse During RSI appeared first on REBEL EM - Emergency Medicine Blog.
