Tick Borne Illness
Tick Borne Illness
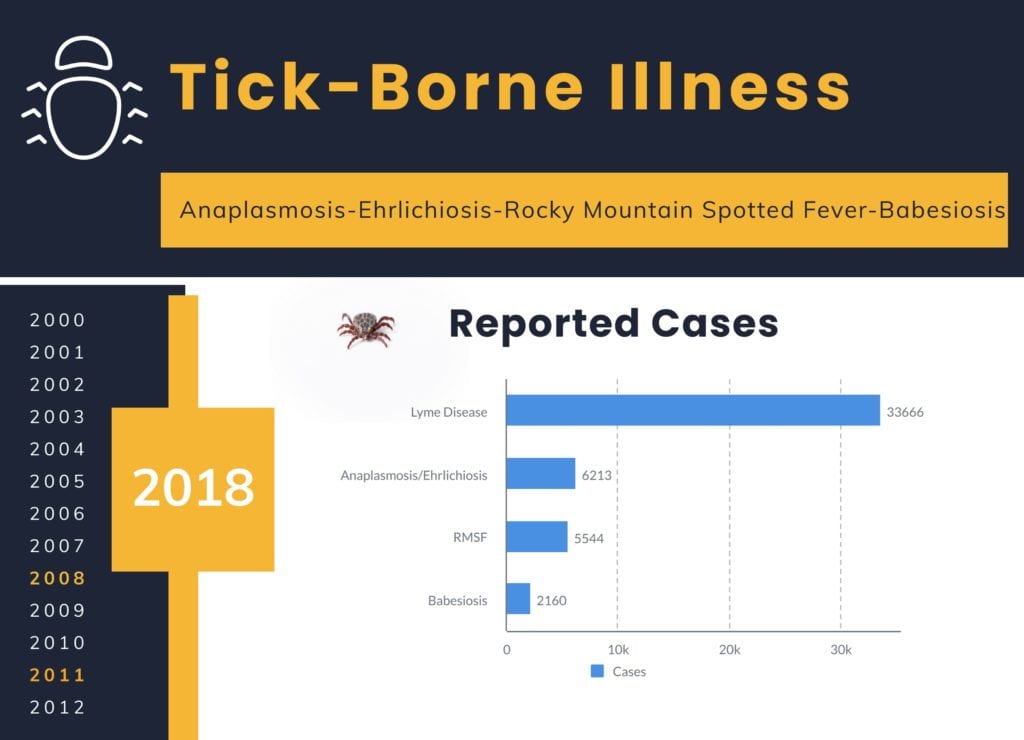
Tick-borne disease surveillance studies have shown increasing prevalence, transmission, and disease burden over the last decade. Tick-borne illnesses remain a public health threat and the true incidence remains unknown and is thought to be underrepresented. Although Lyme Disease is the most frequently reported tick-borne disease in the United States, the incidence of four other tick-borne diseases is noted to be increasing in the United States:
- Anaplasmosis (Nov 3rd, 2020)
- Ehrlichiosis (Nov 4th, 2020)
- Rocky Mountain Spotted Fever (Nov 5th, 2020)
- Babesiosis (Nov 6th, 2020)
In this five-part post, we will review the salient features of these other emerging tick-borne illnesses to increase recognition of these disease entities.
This overview will serve to lay a foundation and summarize shared features of tick-borne illnesses prior to diving into each specific disease.
History and Physical:
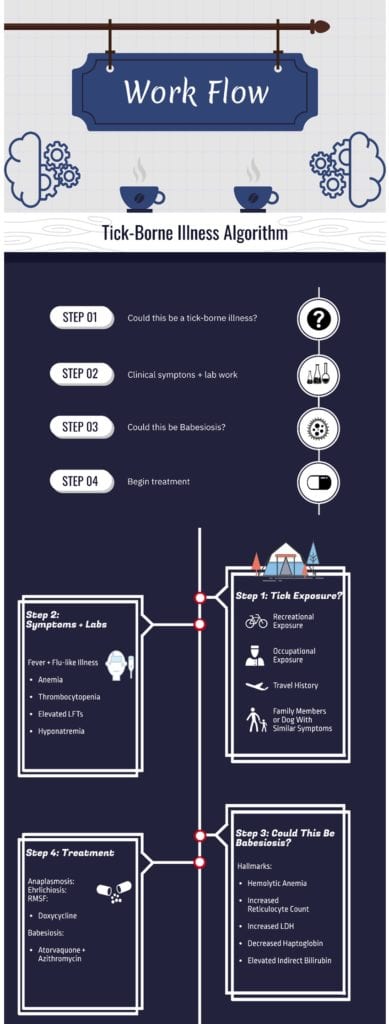
A thorough history should inquire about the following in order to help make a presumptive diagnosis:
- Recent Tick Exposure
- Recreational or Occupational History/Exposure
- Travel History
- Occurrences of Similar Symptoms in Family Members, Coworkers, and Animals (dogs)
-
 Absence of a recognized tick bite does not rule out the consideration of tick-borne illness in the right clinical context
Absence of a recognized tick bite does not rule out the consideration of tick-borne illness in the right clinical context
Poor Prognostic Factors:
- Increased Age
- Immunocompromised States
- Delays in Diagnosis and Treatment
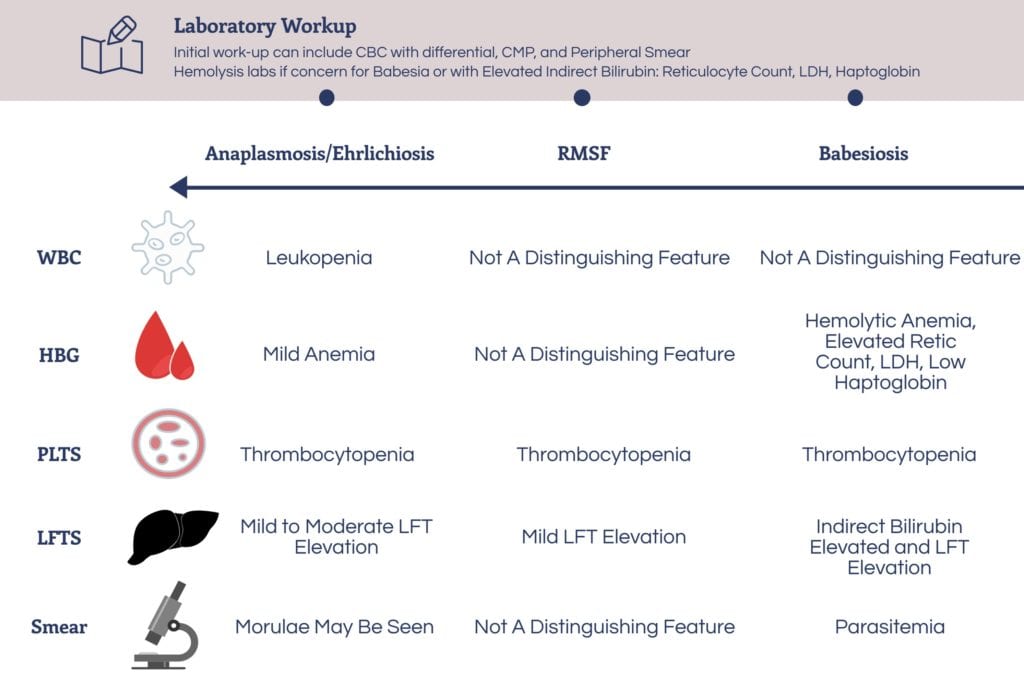
Signs/Symptoms and Laboratory Work-Up:
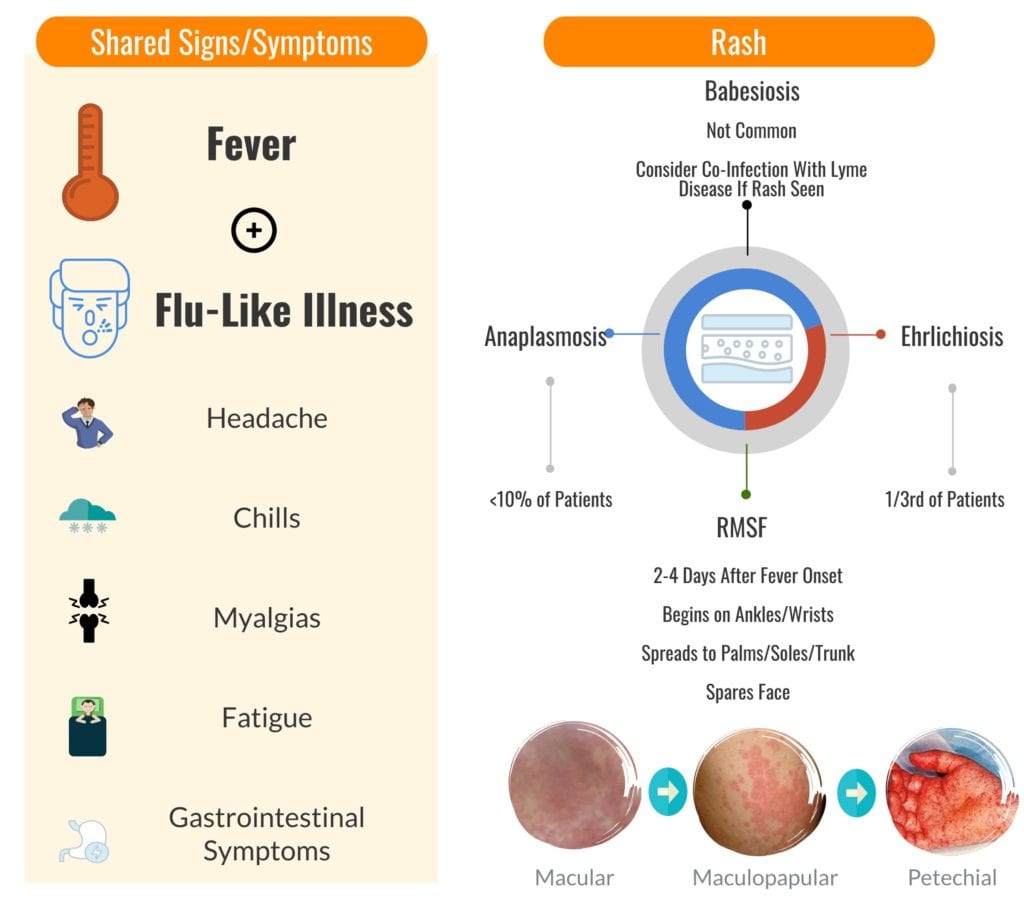
Tick-borne diseases have several shared signs, symptoms, and laboratory findings.
- A simplified way to approach tick-borne illnesses is to look for the presence of unexplained fever along with non-specific flu-like symptoms
- These clinical symptoms along with thrombocytopenia and transaminitis should clue the clinician into further exploring tick-bore illnesses as an etiology of the patient’s symptoms
Management of Tick-Borne Illnesses
Anaplasmosis-Ehrlichiosis-Rocky Mountain Spotted Fever:
Doxycycline is the drug of choice in both pediatric and adult patients (Biggs 2016)
- 100 mg orally or intravenously twice daily for 10 days
- 2 mg/kg (not to exceed 100 mg/dose) twice daily for 10 days in children
- Response to therapy is rapid and failure to improve within 48 hours of treatment suggests possibility of alternative diagnosis.
- The American Academy of Pediatrics and the CDC recommend doxycycline in the pediatric population as the risks of dental staining stem from older tetracycline-class drugs that bound more readily to calcium than newer agents such as doxycycline (Biggs 2016).
- Studies have shown a tooth discoloration rate of 0% in children less than 8 years of age treated with doxycycline (Biggs 2016, Todd 2015, Volovitz 2007).
Rifampin: Possible alternative agent for Anaplasmosis or Ehrlichiosis in those with severe doxycycline allergy or mild infection in the pregnant patient.
- 300 mg orally twice daily for adults for 10 days
- 10 mg/kg (not to exceed 300mg/dose) twice daily for 10 days in children
Chloramphenicol: Possible alternative agent for Rocky Mountain Spotted Fever
- 50-75 mg/kg intravenously every 6 hours for 7-19 days
Babesiosis:
Doxycycline does not cover Babesia species
Mild to Moderate Disease: Atorvaquone plus Azithromycin
- Atorvaquone: 750 mg orally twice daily for 7-10 days
- Azithromycin: 500 mg orally on day 1 followed by 250 mg orally once daily for 7-10 days
Severe Disease: Clindamycin plus Quinine
- Clindamycin: 300-600 mg intravenously every 6 hours for 7-10 days
- Quinine: 650 mg orally every 6 hours for 7-10 days
Exchange Transfusion
- Indications: Parasitemia > 10%, Severe Anemia, Pulmonary, Liver, or Renal Impairment
Take Home Approach:
Guest Post By:

Akash Ray, DO
PGY-2 Emergency Medicine Resident Inspira Medical Center
Vineland, NJ
Twitter: @_kashray
References:
- Biggs H et al. Diagnosis and Management of Tickborne Rickettsial Diseases: Rocky Mountain Spotted Fever and Other Spotted Fever Group Rickettsioses, Ehrlichioses, and Anaplasmosis – United States. MMWR Recomm Rep. 2016. PMID: 27172113
- Todd S et al. No visible dental staining in children treated with doxycycline for suspected Rocky Mountain Spotted Fever. J Pediatr. 2015. PMID: 25794784
- Volovitz B et al. Absence of tooth staining with doxycycline treatment in young children. Clin Pediatr (Phila). 2007. PMID: 17325084
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post Emerging Tick-Borne Illnesses: Not Just Lyme Disease Part 1 appeared first on REBEL EM - Emergency Medicine Blog.