
What They Did:
- Systematic review and meta-analysis comparing the prognostic accuracy of qSOFA vs SIRS for prediction of mortality in patients with suspected infection in the ICU, ED, or hospital wards
Outcomes:
- Primary: Obtain summary estimates of diagnostic performance of qSOFA for prediction of mortality in patients with suspected infection
- Secondary: Obtain summary estimates of diagnostic performance of SIRS for prediction of mortality in patients with suspected infection
Inclusion:
- English language abstracts and full-text articles
- Retrospective and prospective observational studies
- Randomized and quasi-randomized controlled studies
- Adult patients age ≥16 years with suspected infection
- Conducted in the ED, hospital wards, or ICU
- Application of qSOFA for prediction of mortality
Exclusion:
- Studies evaluating all-cause mortality ≥30 days or uspecified follow-up periods
- Case reports, case series, animal studies, pediatric studies
- Studies evaluating qSOFA for a composite outcome
Results:
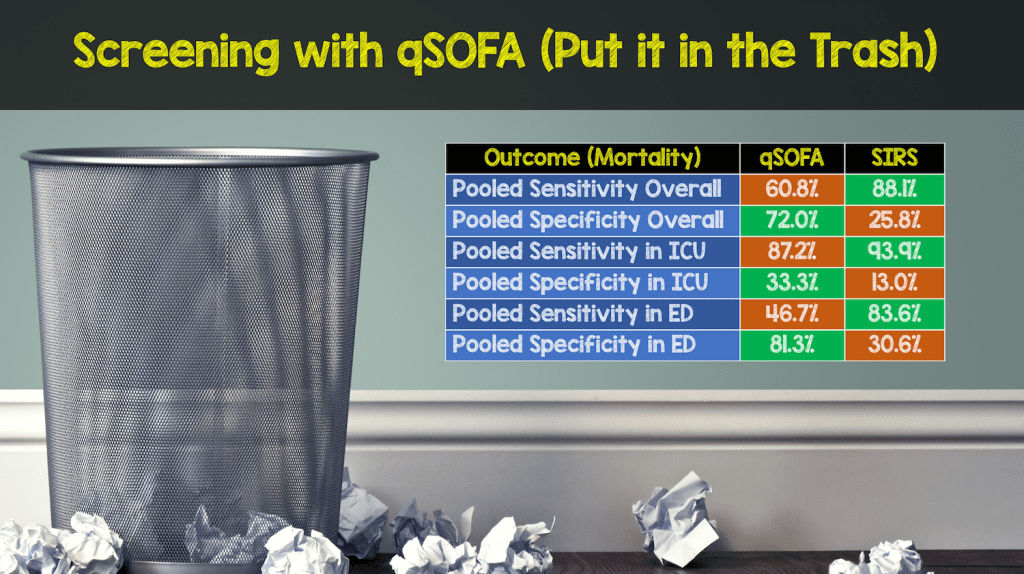
- 38 studies with >385,000 patients were included in the study
Strengths:
- Used a structured criteria for the systematic review – PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) and Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy
- Risk of bias was assessed by using QUADAS-2 (Quality Assessment of Diagnostic Accuracy Studies 2)
- Subgroup analyses were used in ICU patients to assess for heterogeneity of studies included
- Overall confidence of pooled results was assessed using the GRADE (Grading of Recommendations Assessment, Development, and Evaluation) Tool
- Comprehensive search of multiple databases with clear inclusion/exclusion criteria
Limitations:
- Risk of bias in included studies due to qSOFA interpretation and patient selection
- Many studies do not mention if qSOFA was calculated by providers blinded to the outcomes
- Several studies only applied qSOFA to specific populations (i.e. neutropenic fever, pneumonia, etc..)
- The definition of suspected infection is heterogeneous among studies
Discussion:
- The authors of this paper state: “The sensitivity of qSOFA for predicting mortality was poor, and use of this tool for screening would likely miss many cases.”
- It is important to remember that the addition of qSOFA to SIRS was designed as a an early warning risk stratification tool for patients with higher risk for death, not a screening tool
- Performance of qSOFA varies depending on the population with which it is applied (i.e. more sensitive in ICU patients than non-ICU patients)
Author Conclusion: “qSOFA had poor sensitivity and moderate specificity for short-term mortality. The SIRS criteria had sensitivity superior to that of qSOFA, supporting their use for screening of patients and as a prompt for treatment initiation.”
Clinical Take Home Point: At this time, SIRS criteria + clinical judgment should continue to be used for screening patients outside the ICU (i.e. In the ED and Hospital Wards) while the addition of qSOFA can help predict the patients with the highest risk of deterioration and death.
References:
- Fernando SM et al. Prognostic Accuracy of the Quick Sequential Organ Failure Assessment for Mortality in Patients With Suspected Infection: A Systematic Review and Meta-Analysis. Ann Intern Med 2018. PMID: 29404582
- Kaukonen KM et al. Systemic Inflammatory Response Syndrome Criteria for Severe Sepsis. NEJM 2015. PMID: 26308693
For More Thoughts on This Topic Checkout:
- Paul Marik at EMCrit: iSepsis – Sepsis 3.0 – Flogging a Dead Horse
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami)
The post The SIRS & qSOFA Confusion in Sepsis appeared first on REBEL EM - Emergency Medicine Blog.
