
What They Did:
- Observational cohort study from the Swedish national quality register for sepsis
- 30 ICU’s in Sweden
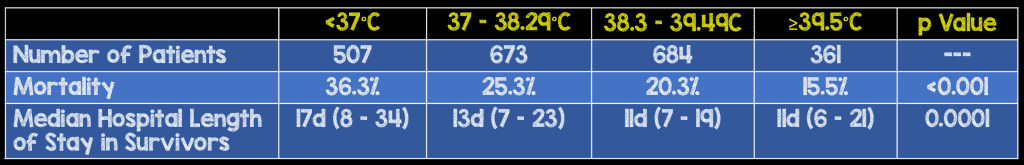
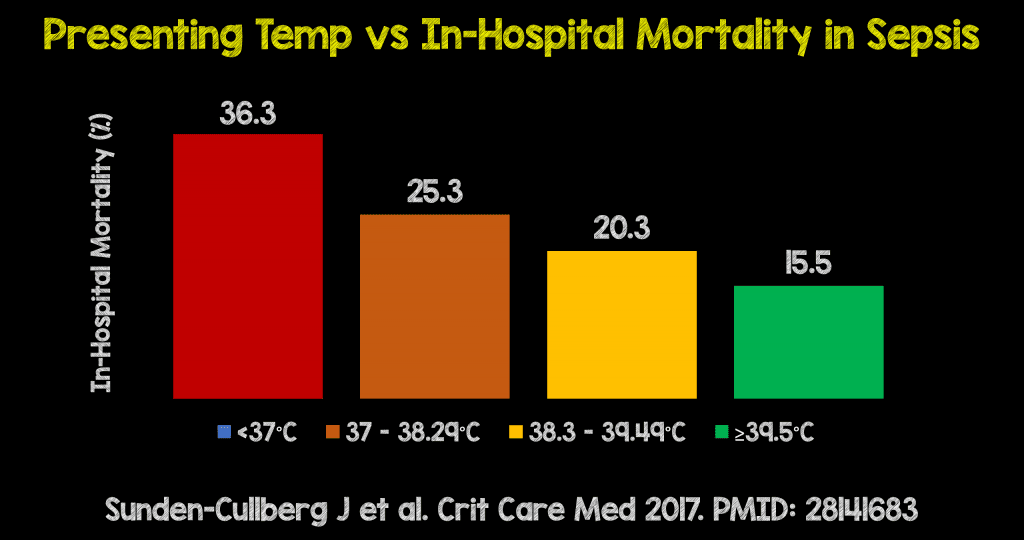
- Divided patients into four categories
- <37 C
- 37 – 38.29 C
- 3 – 39.5 C
- ≥39.5 C
Outcomes:
- Primary: In-hospital Mortality
Inclusion:
- Enrolled in the Swedish National Quality Sepsis Register (NQSR)
- >17 years of age
- Admitted to the ICU with a diagnosis of severe sepsis or septic shock within 24 hours of arrival to the ED
Results:
- 2,225 adults admitted to the ICU within 24 hours of hospital arrival with a diagnosis of severe sepsis or septic shock
- Overall mortality: 25%
CRITICAL RESULTS:
- In-hospital mortality decreased >5% for every increase by °C from 35°C up to >41°C
- Of the clinical signs, body temperature had the highest predictive value for in-hospital mortality followed by respiratory rate >heart rate > O2 saturation > systolic blood pressure
- Difference persisted despite variance in compliance with sepsis guidelines reflecting a possible lower quality of care.
Strengths:
- Multicenter study
- Evaluated the relationship between body temperature and in-hospital mortality stratified by age, lactate level, bacterial etiology, or sepsis bundle achievement
- 1st study to investigate the prognostic significance of fever upon ED arrival in patients subsequently admitted to the ICU for sepsis
- Lack of severity scores (i.e. SOFA) not allowing to adjust for disease severity
- Information about antipyretics or immune-modifying drugs prior to arrival to ED were also lacking
- Analyses were adjusted for quality of care, but it is possible that other differences in treatment were not captured in the database
- The Swedish NQSR does not capture all eligible patients in Sweden and only comprises hospitals where infectious disease physicians are present
Limitations:
- Lack of a uniform way to measure temperature (TM, Oral, Rectal) could have resulted in measurement errors
- A large proportion of patients in this study had missing data (Only 58% of patients had complete information on all variables)
- Almost 10% of the population did not have temperature documented
- Missing values were more prevalent in patients without fever (i.e. lower quality of care)
Discussion:
- Quality of care, measured by sepsis bundle achievement improved with rising temperatures. Treatment limitations were almost twice as common in the lowest compared with the highest temperature category. The authors of this paper however adjusted for sepsis bundle achievement and still found a statistically significant difference in mortality associated with temperature (i.e. better care alone did not explain fever-mortality association)
- At this time, it is unclear if treating fever with antipyretic medications is beneficial or harmful in critically ill patients. The HEAT Trial, which included 700 ICU patients with probable infection randomized patients to IV acetaminophen or placebo and showed no differences in ICU-free days or 30d mortality.
- Currently, researcher Paul Young (The lead author of the HEAT Trial) has just initiated the Randomised Evaluation of Aggressive Control of Temp vs. ORdinary temp mngmt (REACTOR) Trial. In the REACTOR trial patients will be randomized to active prophylaxis and treatment of fever vs standard care. #REACTORtrial
Author Conclusion: “Contrary to common perceptions and current guidelines for care of critically ill septic patients, increased body temperature in the emergency department was strongly associated with lower mortality and shorter hospital stays in patients with severe sepsis or septic shock subsequently admitted to the ICU.”
Clinical Take Home Point: It is the patients with severe sepsis and septic shock who DO NOT have fever, that we must pay more attention to. Currently, the qSOFA score does not use temperature as a predictor of mortality and in this study, temperature was the vital sign that had the best prediction of in-hospital mortality.
References:
- Sunden-Cullberg, J et al. Fever in the Emergency Department Predicts Survival of Patients with Severe Sepsis and Septic Shock Admitted to the ICU. Crit Care Med 2017. 45: 591 – 99. PMID: 28141683
For More Thoughts on This Topic Checkout:
- ScanCrit: Is Fever the Normal Temperature of Sepsis?
- Ken Milne at The SGEM: SGEM#195 – Some Like it Hot – ED Temperature and ICU Survival
Post Peer Reviewed By: Matt Astin (Twitter: @mastinmd)
The post Is Fever the New Hotness in Sepsis? appeared first on REBEL EM - Emergency Medicine Blog.
