
 Background: Just a few months ago the surviving sepsis campaign published their international guidelines for management of sepsis and septic shock [1]. There has been a lot of talk in the FOAM world about sepsis 3.0 and this is the first update since the introduction. This was a 67 page document that made a total of 93 statements on the early management and resuscitation of patients with sepsis or septic shock. 1/3 of the statements were strong recommendations and just over 1/3 were weak recommendations. Instead of going through every component of this document, we thought we would discuss one of the potentially biggest components of sepsis care that would affect clinical practice for those of us on the front lines.
Background: Just a few months ago the surviving sepsis campaign published their international guidelines for management of sepsis and septic shock [1]. There has been a lot of talk in the FOAM world about sepsis 3.0 and this is the first update since the introduction. This was a 67 page document that made a total of 93 statements on the early management and resuscitation of patients with sepsis or septic shock. 1/3 of the statements were strong recommendations and just over 1/3 were weak recommendations. Instead of going through every component of this document, we thought we would discuss one of the potentially biggest components of sepsis care that would affect clinical practice for those of us on the front lines.
One of the main reasons we have seen a mortality decrease in sepsis overtime is due to the proactive nature health care professionals have taken in sepsis management. The so called ABC’s of sepsis management: Early identification, Early fluids, and Early antibiotics. One of the biggest components of this is early identification of these patients.
Episode 37 – Definitions and Identification of Sepsis: Sepsis 2.0 vs Sepsis 3.0
Click here for Direct Download of Podcast
Lets Start with Some Basic Definitions:
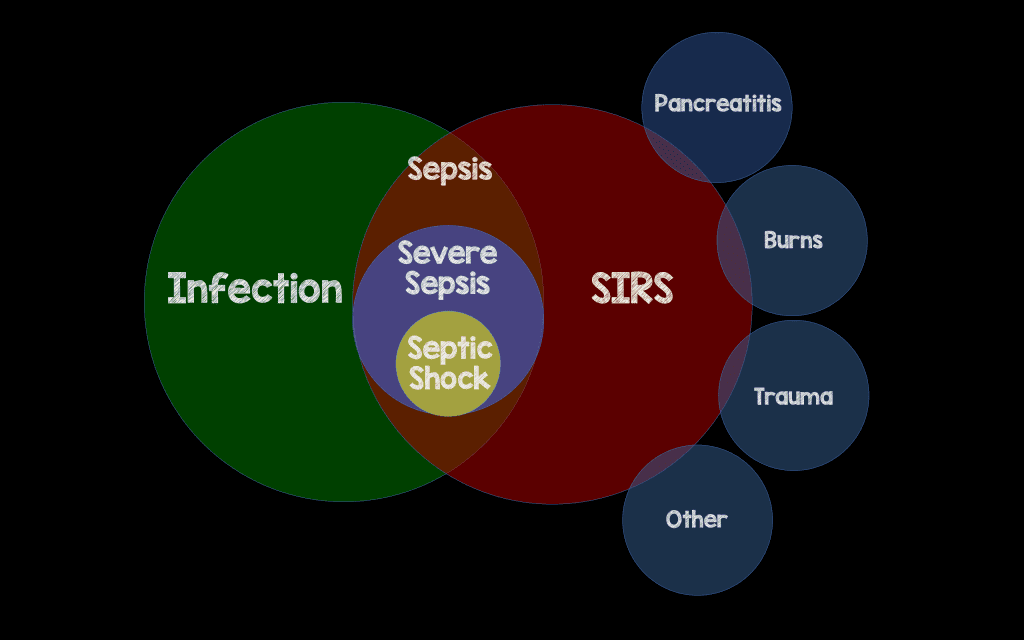
Sepsis 2.0 Definitions
- SIRS
- Temp > 100.4 or < 95.0
- RR > 20 or PaCO2 < 32mmHg
- HR > 90/min
- WBC >12k or <4k or Band > 10%
- Sepsis = 2 SIRS criteria + infection
- Severe Sepsis = sepsis + organ dysfunction
- Septic Shock = severe sepsis + persistent hypotension after 30cc/kg IVF resuscitation
- The biggest issue with these definitions is infection isn’t the only thing that can cause SIRS (poor specificity, but, maybe, poor sensitivity as well.
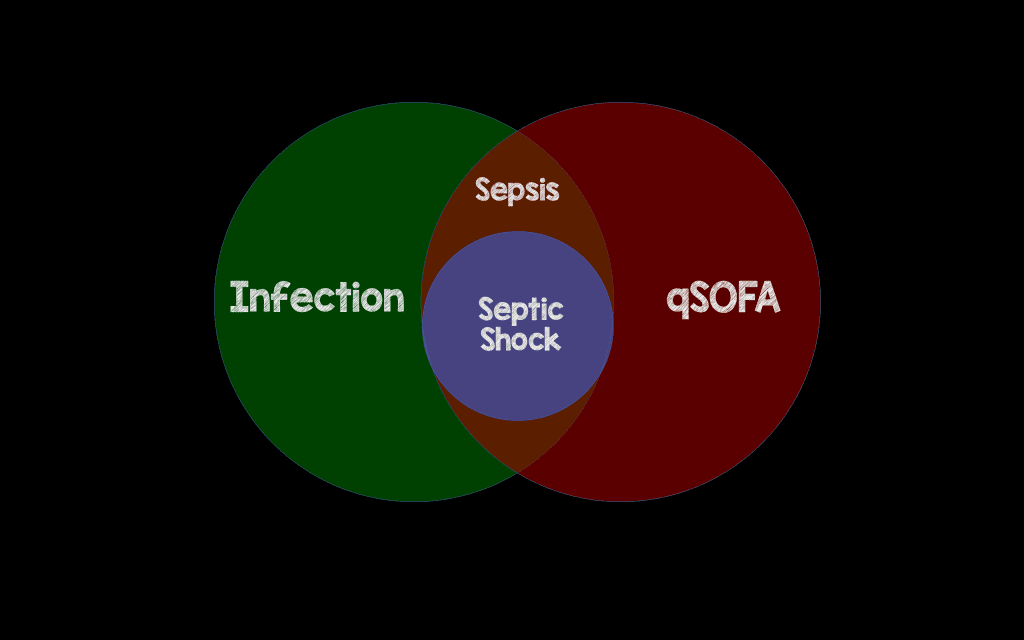
Sepsis 3.0 Definitions
- Quick Sepsis-related Organ Failure Assessment (qSOFA)
- Hypotension: SBP < 100mmHg
- Altered Mental Status
- Tachypnea: RR > 22/Min
- Score of ≥2 Criteria Suggests a Greater Risk of a Poor Outcome (i.e. Increased Mortality)
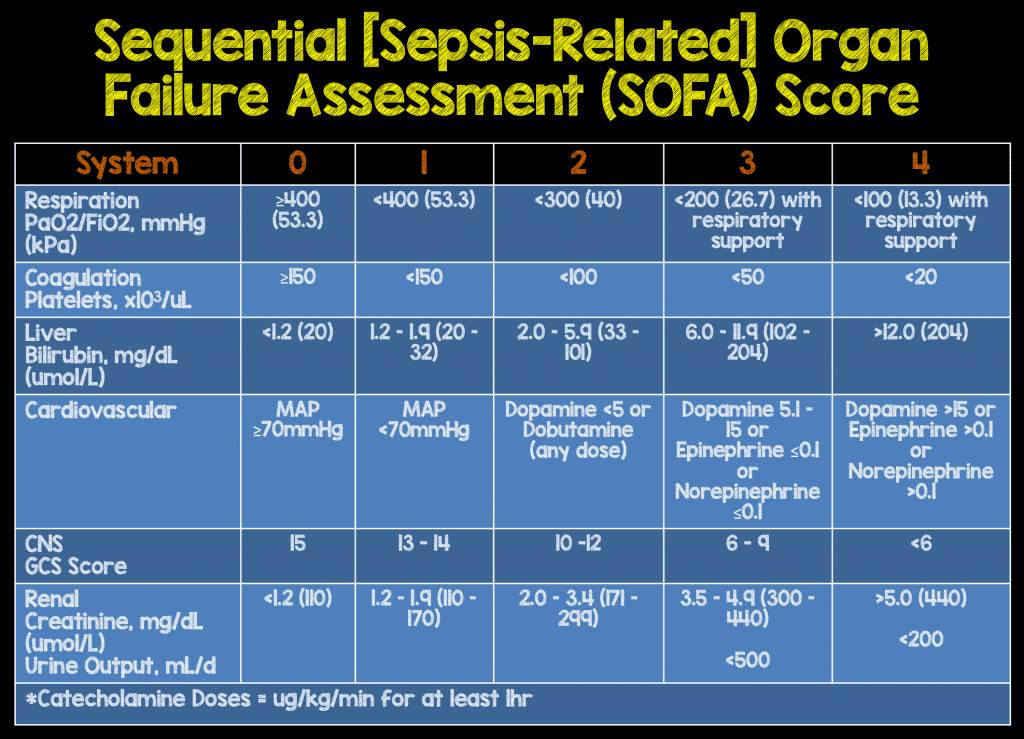
- Sepsis = “Life-threatening organ dysfunction due to a dysregulated host response to infection.”
- There is No More Severe Sepsis
- Septic Shock = “Subset of sepsis where underlying circulatory and cellular/metabolic abnormalities are profound enough to substantially increase mortality.”
- Needing vasopressors for a MAP ≥ 65mmHg
- An increase in lactate > 2 mmol/L, despite adequate fluid resuscitation
- The biggest issue with these definitions is they were derived in the ICU setting and helped increase specificity, but, in the process, decreased sensitivity
Sepsis 2.0 vs Sepsis 3.0
There have been several studies that have evaluated the usefulness of qSOFA compared to SIRS. We handpicked 3 papers just to help get our point across. Not a deep dive of the papers like we usually do, but instead just a simple review of results.
Paper #1: Churpek MM et al. qSOFA, SIRS, and Early Warning Scores for Detecting Clinical Deterioration in Infected Patients Outside the ICU. Am J Respir Crit Care Med 2016 [2].
- >30,000 patients admitted from the ED or transferred from the wards had a qSOFA, SIRS, Modified Early Warning Score (MEWS), and the National Early Warning Score (NEWS) compared for predicting death and ICU transfer.
- Discrimination for in-hospital mortality from best to worst:
- NEWS (AUC 0.77)
- MEWS (AUC 0.73)
- qSOFA (AUC 0.69)
- SIRS (AUC 0.65)
- Bottom Line: Early warning scores are more accurate than qSOFA & SIRS for predicting death and ICU transfer in non-ICU patients
Paper #2: Raith EP et al. Prognostic Accuracy of the SOFA Score, SIRS Criteria, and qSOFA Score for IN-Hospital Mortality Among Adults With Suspected Infection Admitted to the Intensive Care Unit. JAMA 2017 [3].
- This was an external validation via a retrospective cohort analysis of >184,000 patients with infection-related primary admission in 182 ICUs. Their main goal was to evaluate the discriminatory capacity of increases in SOFA ≥2 points, qSOFA ≥2, and SIRS ≥2 for in-hospital mortality.
- Discrimination for in-hospital mortality from best to worst:
- SOFA (AUC 0.753)
- qSOFA (0.607)
- SIRS (0.589)
- Bottom Line: Among adult patients with suspected infection admitted to an ICU increase in SOFA ≥2 had greater prognostic accuracy for in-hospital mortality than SIRS and qSOFA
Paper #3: Freund Y et al. Prognostic Accuracy of Sepsis-3 Criteria for In-Hospital Mortality Among Patients With Suspected Infection Presenting to the Emergency Department. JAMA 2017 [4].
- This was an external validation via a prospective cohort analysis of >800 patients from 30 EDs with suspected infection. And what they did was measure qSOFA, SOFA, and SIRS to determine in-hospital mortality.
- Prediction of in-hospital mortality from best to worst:
- qSOFA (AUC 0.80)
- SOFA (0.77)
- SIRS/Severe Sepsis (AUC 0.65)
- But this what at the cost of sensitivity. Sensitivity from best to worst:
- SIRS 93%
- SOFA 73%
- qSOFA 70%
- Bottom Line: qSOFA had a greater prognostic accuracy for in-hospital mortality than did either SIRS of severe sepsis, and although this is an important endpoint, it does not help with screening for those cryptic septic patients in the ED.
2016 Surviving Sepsis Guidelines
The newest Surviving Sepsis Guidelines don’t really make any comment or recommendation on use of qSOFA. Neither score is perfect, and the truth of the matter is, the reality is probably somewhere in the middle. Sepsis is truly a spectrum of disease that is difficult to compartmentalize. Patients can quickly change from better to worse or worse to better within minutes to hours of presentation. If the patient looks sick, you don’t need a score to tell you that.
Clinical Bottom Line: Neither score is perfect. On one hand, Sepsis 2.0 has a better sensitivy for screening but at the cost of specificity as so many other things can cause SIRS. On the other hand, Sepsis 3.0 has a better specificity for prediciton of mortality when compared to Sepsis 2.0, but there maybe other scores out there that may do a better job.
References:
- Rhodes A et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock. Crit Care Med 2017 [epub ahead of print] PMID: 28101605
- Churpek MM et al. qSOFA, SIRS, and Early Warning Scores for Detecting Clinical Deterioration in Infected Patients Outside the ICU. Am J Respir Crit Care Med 2016. [epub ahead of print]. PMID: 27649072
- Raith EP et al. Prognostic Accuracy of the SOFA Score, SIRS Criteria, and qSOFA Score for IN-Hospital Mortality Among Adults With Suspected Infection Admitted to the Intensive Care Unit. JAMA 2017; 317(3): 290 – 300. PMID: 28114553
- Freund Y et al. Prognostic Accuracy of Sepsis-3 Criteria for In-Hospital Mortality Among Patients With Suspected Infection Presenting to the Emergency Department. JAMA 2017; 317(3): 301 – 308. PMID: 28114554
- Henning DJ et al. An Emergency Department Validation of the SEP-3 Sepsis and Septic Shock Definitions and Comparison With 1992 Consensus Definitions. Ann Emerg Med 2017. S0196-0644(17): 30023 -9. PMID: 28262318
The post Episode 37 – Definitions and Identification of Sepsis: Sepsis 2.0 vs Sepsis 3.0 appeared first on REBEL EM - Emergency Medicine Blog.
