
 Background: Intraosseous (IO) access can play an important role in the resuscitation of the critically ill patient to help expedite delivery of critical medications (i.e. RSI). Much like with peripheral or central access, obesity can present a challenge to placement of an IO as accurate placement relies on use of landmarks which may not be palpable in this group. Additionally, increased soft tissue depth may render standard needles ineffective. IO needles require 5 mm of excess length from skin to bony cortex to ensure successful placement (i.e. maximal depth of 20 mm for a 25 mm needle). Studies investigating these questions are necessary in order to understand how reliable IO access will be in obese patients.
Background: Intraosseous (IO) access can play an important role in the resuscitation of the critically ill patient to help expedite delivery of critical medications (i.e. RSI). Much like with peripheral or central access, obesity can present a challenge to placement of an IO as accurate placement relies on use of landmarks which may not be palpable in this group. Additionally, increased soft tissue depth may render standard needles ineffective. IO needles require 5 mm of excess length from skin to bony cortex to ensure successful placement (i.e. maximal depth of 20 mm for a 25 mm needle). Studies investigating these questions are necessary in order to understand how reliable IO access will be in obese patients.
Article:
Kehrl T et al. Intraosseous access in the obese patient: assessing the need for extended needle length. Am J Emerg Med 2016; 34: 1831-4. PMID: 27344097
Clinical question: What is the relationship between body mass index (BMI), and the ability to palpate the tibial tuberosity (TT) and soft tissue depth at standard IO insertion sites?
Population: Obese patients (defined as BMI > 30 based on current height and weight entered in hospital EMR)
Intervention: Measurement of soft tissue depth by ultrasound at proximal humerus, proximal and distal tibia (3 most common IO placement locations). The investigator performing were ultrasound fellows who also evaluated whether the TT was palpable or non-palpable.
Outcome (primary): Soft tissue depth at IO insertion sites (defined as distance from skin surface to outer bony cortex in mm). Recorded both continuous variable and dichotomous variable (</= 20 mm or > 20 mm)
Outcomes (secondary): TT palpability
Design: Prospective, observational, convenience sample study of obese patients presenting to an urban ED.
Excluded: Any existing condition that might preclude IO access i.e. overlying infection, trauma, prior amputation) (authors state no exclusions encountered during study)
Primary Results:
- 75 patients enrolled
- Mean BMI = 47.2
Critical Results:
-
Mean soft tissue depth (primary outcome)
- Proximal Humerus: 29.6 mm (CI 27.5 – 31.7)
- Proximal Tibia: 11.0 mm (CI 8.9 – 13.0)
- Distal Tibia: 10.7 mm (CI 9.4 – 12.1)
-
TT palpability (secondary outcome)
- Palpable in 70 patients with average BMI = 45.7
- Non-palpable in 5 patients with average BMI = 67.2
- In patients with a non-palpable TT (n = 5) soft tissue depth exceeded 20 mm at all three IO sites
Strengths:
- Asks important question regarding IO use in an increasingly common patient population
Limitations:
- Study includes a small number of patients collected by convenience sample
- Did not have multiple operators perform soft tissue depth measurements to assess for inter-rater reliability
- Did not have multiple operators assess for palpability of TT to assess for inter-rater reliability
- Patients did not have IO placed to confirm failure or success of placement
- BMI extracted from most recent data in EMR. May not be accurate
- Unable to control for physical compression applied by US during measurement
- The lower limit of the interquartile range was a BMI of 39.7. The study result can not be extrapolated to obese patient with a lower BMI
Author’s Conclusions:
“In obese adults with a palpable TT or BMI ≤43 a 25mmIO needle is likely adequate at the proximal and distal tibial insertion sites. Empiric use of an extended 45mmIO needle is advisable at the proximal humeral insertion site in obese patients.”
Our Conclusions:
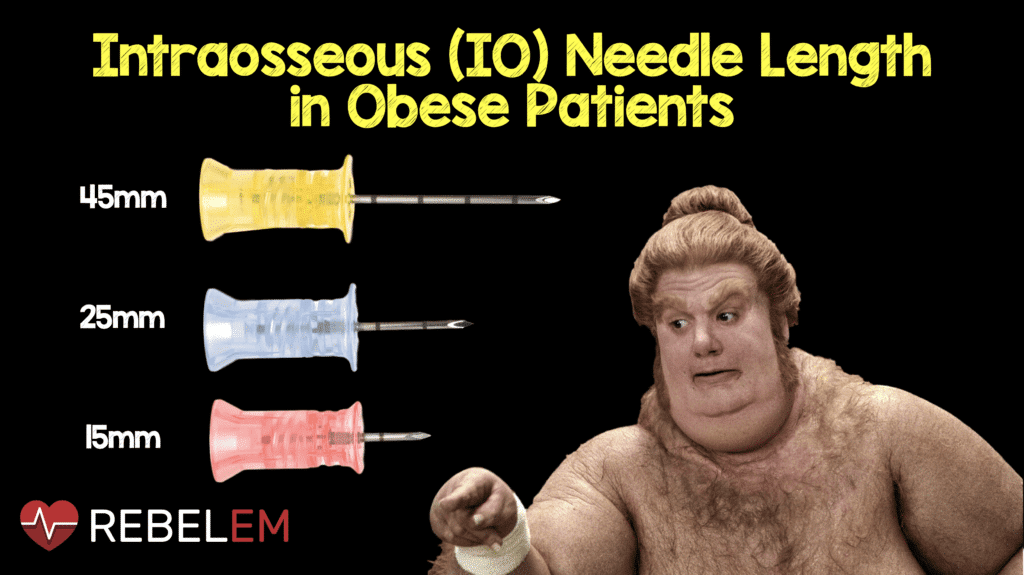
Obesity may limit the utility of the short (25 mm) IO needle for access. In obese patients, or in those with a non-palpable TT, employ the longer, 45 mm IO needle to increase the likelihood of successful IO placement.
Potential Impact to Current Practice:
In obese patients, it is reasonable to reach for the 45 mm IO needle instead of the 25 mm needle to ensure adequate length to obtain access. The 45 mm IO needles can be used at any site regardless of depth as long as the provider does not “bury the needle.” Placement until the needle penetrates the cortex (possibly leaving some portion of the needle protruding from the skin) will provide IO access at all three common sites.
Bottom Line:
The 25 mm IO needle may not provide proper length for obtaining IO access in obese patients. Consider reaching for the 45 mm IO needle in these patients particularly if you cannot palpate the tibial tuberosity.
Post Peer Reviewed By: Salim Rezaie (Twitter: @srrezaie)
The post Intraosseous (IO) Needle Length in Obese Patients appeared first on REBEL EM - Emergency Medicine Blog.
