
 Background: I received a text message from one of my colleagues inquiring about discharging a patient home with isolated traumatic subarachnoid hemorrhage and to be honest I had heard about this practice, but was not completely aware of the literature around it. Turns out from a PubMed search there was a meta-analysis published just this past year trying to answer this very question. When I was a resident, which is not that long ago, the standard practice was for patients to be assessed by neurosurgery for management which usually involved ICU admission or a trip to the OR with ICU admission. Isolated traumatic subarachnoid hemorrhage (itSAH) is typically defined as the presence of a SAH in the absence of any other traumatic radiographic intracranial pathology. So the question is, is it safe to discharge patients home with itSAH?
Background: I received a text message from one of my colleagues inquiring about discharging a patient home with isolated traumatic subarachnoid hemorrhage and to be honest I had heard about this practice, but was not completely aware of the literature around it. Turns out from a PubMed search there was a meta-analysis published just this past year trying to answer this very question. When I was a resident, which is not that long ago, the standard practice was for patients to be assessed by neurosurgery for management which usually involved ICU admission or a trip to the OR with ICU admission. Isolated traumatic subarachnoid hemorrhage (itSAH) is typically defined as the presence of a SAH in the absence of any other traumatic radiographic intracranial pathology. So the question is, is it safe to discharge patients home with itSAH?
What They Did: This was a systematic review and meta-analysis to evaluate the outcomes of patients with itSAH with a presenting GCS of 13 – 15.
Outcomes:
-
Primary:
- Need for neurosurgical intervention on presentation to hospital
- Need for neurosurgical intervention at any point following initial trauma
-
Secondary:
- Neurologic deterioration
- Radiographic progression
- All-cause mortality
- Death due to neurologic insult
Inclusion:
- Studies of any design, with the exception of review articles and small sample sizes (n <10)
- Radiographically confirmed (CT or MRI) intracranial injury limited to itSAH
- Initial GCS 13 – 15
- Data on one of the following outcomes: Need for neurosurgical intervention on presentation, neurologic deterioration, radiographic progression, eventual need for neurosurgical intervention, all-cause mortality, or death due to neurological insult
Exclusion:
- Studies prior to the year 2000 (2000 was the approximate time when high-resolution fifth-generation CT scanners became available)
Results:
- 13 studies reporting on 15,372 patients included in the review
- All but one study was retrospective
- All studies performed at Level 1 trauma centers
- Only 1 study outside the US
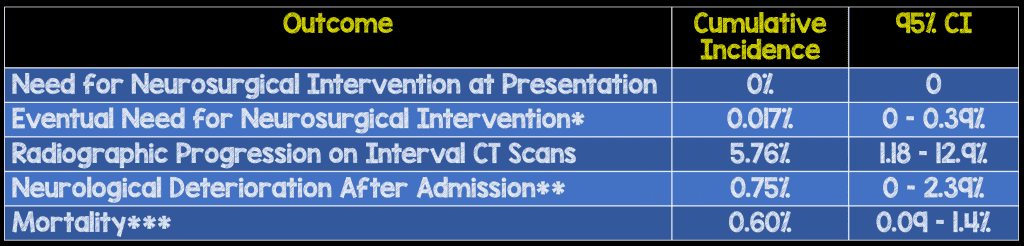
*Almost all patients for this outcome derived from one study with 197 out of 13,191 patients requiring neurosurgical intervention (Indications, details of neurosurgical intervention, or postoperative course not detailed)
**13 Patients with Neurological Deterioration (Key Bad Outcomes: 1 Bilateral SDH Requiring Evacuation & 1 ICH & Death from Herniation)
***Only one death could be determined to be from neurologic injury and this patient was on warfarin
Strengths:
- Asks a clinically important question
- First meta-analysis to examine the outcomes of patients with GCS 13 – 15 & itSAH
- The authors followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement and Meta-Analysis of Observational Studies in Epidemiology guidelines
- Data were verified for accuracy by a third author
- Discrepancies were resolved by discussion and consensus and when necessary, with review of a fourth author
Limitations:
- Funnel plots suggest a potential for publication bias when exploring need for neurosurgical intervention on presentation and eventual need for neurosurgical intervention as outcomes
- The authors were not able to conduct a subgroup analysis to determine if deaths were due to intracranial or extracranial injuries
- No randomized controlled trials in this meta-analysis meaning the quality of included studies was relatively low due to the retrospective nature of included trials
- Elderly, children, and alcohol-dependent patients were not studied in this meta-analysis making it impossible to draw any conclusions in these patient populations
- Only 3 studies in this meta-analysis published data regarding anticoagulant/antiplatelet use, which means we can’t really draw any conclusions in this patient population from this study
- The vast majority of patients were from a single study that left out critical information.This likely biases the conclusions of this meta-analysis
- Confidence intervals are relatively wide on neuro deterioration and death
Discussion:
- An important point to note is that despite 0 – 26% (Cumulative incidence of 5.7%) of patients having progression of lesions on interval imaging, only 0.75% experienced neurological deterioration and 0.0017% eventually required neurosurgical intervention. Extremely low numbers!!! As we are trying to cut down on health costs and ionizing radiation to patients, this seems to be an optimal group to forgo repeat imaging unless there are changes in neuro status or other unique factors.
Author Conclusion:“These patients experience very low rates of radiographic progression and neurologic deterioration and rarely require neurosurgical intervention or die due to neurological injury.”
Clinical Take Home Point: Based on the methodologically limited data available, it does not appear that patients with itSAH are at a significant risk of requiring neurosurgical intervention, decompensation, or death. However the poor quality of the included studies prevents us from making a strong recommendation. It is instead, advisable to discuss this literature with your neurosurgeons and create a protocol based on regional best practices. No conclusions can be drawn about patients on anticoagulation/antiplatelet agents, the elderly, children, or patients with alcohol and drugs in their system based on this meta-analysis.
References:
- Nassiri F et al. The Clinical Significance of Isolated Traumatic Subarachnoid Hemorrhage in Mild Traumatic Brain Injury: A Meta-Analysis. J Trauma Acute Care Surg 2017. PMID: 289697013
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post Is it Safe to Discharge Patients Home with Isolated Traumatic Subarachnoid Hemorrhage (itSAH)? appeared first on REBEL EM - Emergency Medicine Blog.
