
 Background: High quality CPR and early defibrillation are the cornerstones of improving outcomes in cardiac arrest. We know that prolonged duration of pauses during chest compressions affect hemodynamics, shock conversion rates and ultimately survival [2]. Therefore, it is paramount to reduce hands-off time during chest compressions. A potential next step to reduce hands-off time might be pre-charging the defibrillator before pausing chest compressions for rhythm analysis.
Background: High quality CPR and early defibrillation are the cornerstones of improving outcomes in cardiac arrest. We know that prolonged duration of pauses during chest compressions affect hemodynamics, shock conversion rates and ultimately survival [2]. Therefore, it is paramount to reduce hands-off time during chest compressions. A potential next step to reduce hands-off time might be pre-charging the defibrillator before pausing chest compressions for rhythm analysis.
Paper: Iversen BN et al. Pre-Charging the Defibrillator Before Rhythm Analysis Reduces Hands-Off Time in Patients with Out-Of-Hospital Cardiac Arrest with Shockable Rhythm. Resuscitation 2021. PMID: 34627866
Clinical Question: Does pre-charging the defibrillator prior to rhythm checks reduce the hands-off time during chest compressions in cardiac arrest?
What They Did:
- Retrospective, observational study comparing defibrillation methods in Denmark
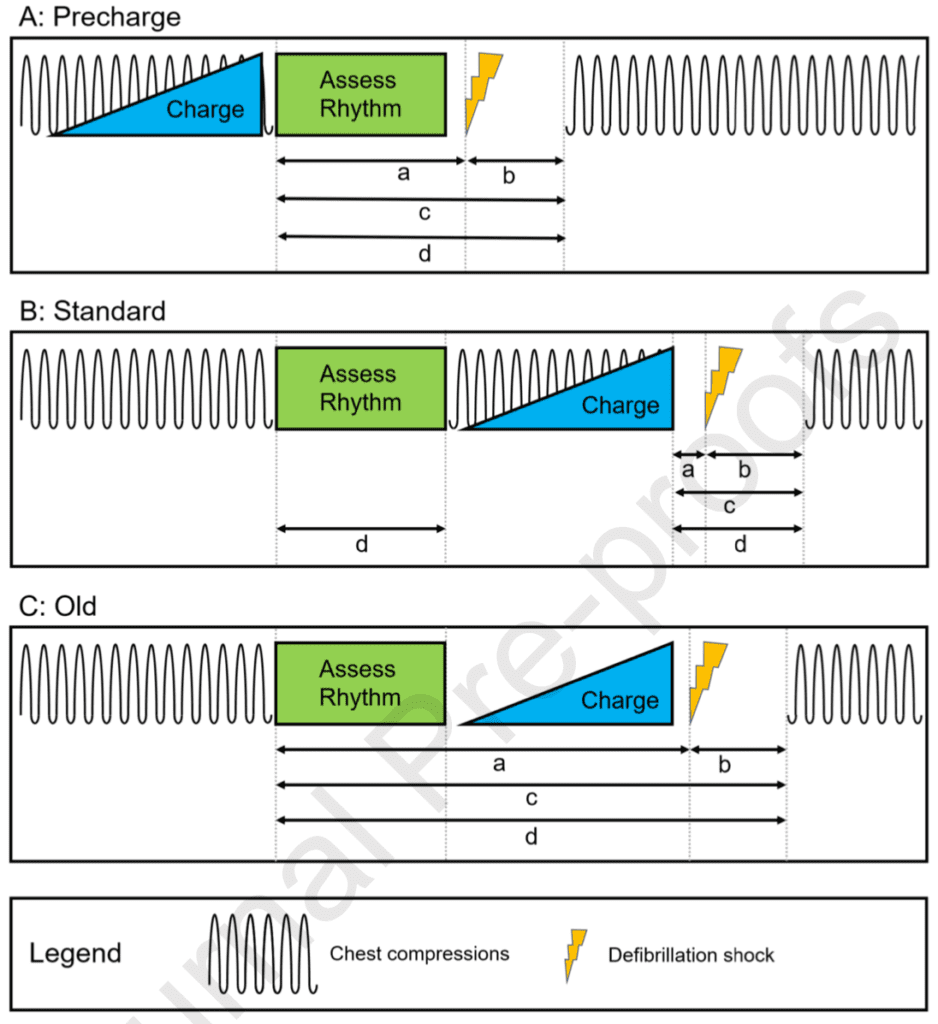
- Defibrillation methods:
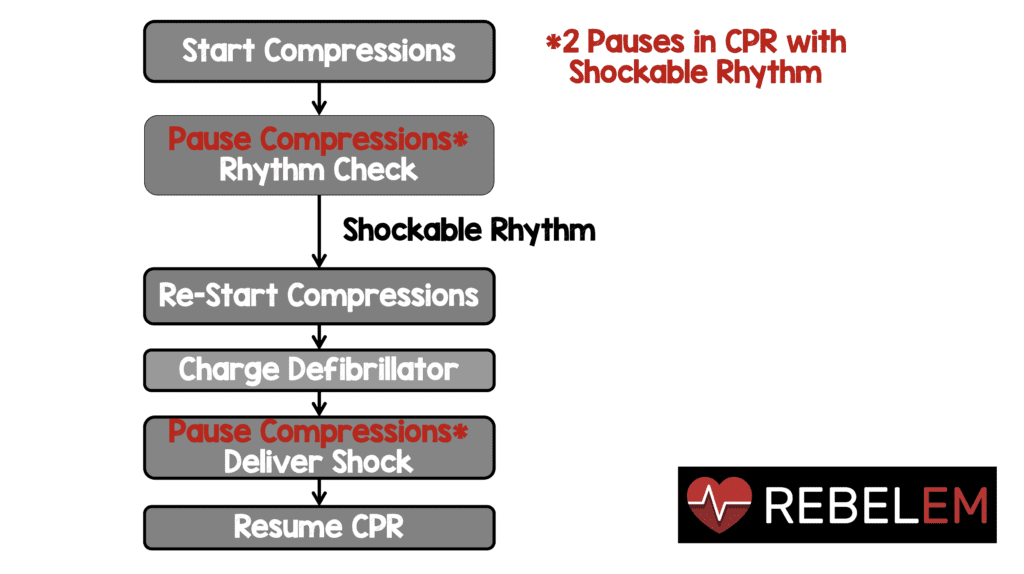
- Standard: Pausing compressions for rhythm analysis, resuming compressions during defibrillator charging and pausing compressions during shock delivery
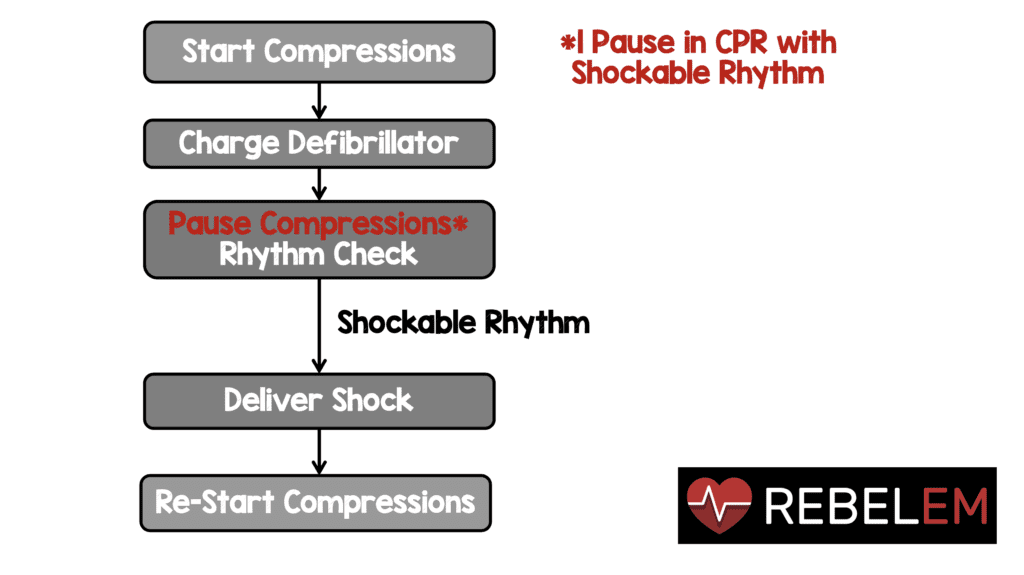
- Precharge: Charging the defibrillator prior to rhythm analysis pause and shocking immediately if indicated
- Old: Pausing compressions for rhythm analysis, charging the defibrillator, then delivering the shock before resuming compressions
Outcomes:
- Primary: Change in hands-off time
-
Secondary:
- Duration of pre-, post-, and peri-shock pauses
- Change in total hands-off fraction
Inclusion:
- Adult patients (≥18 years)
- Defibrillated at least once during resuscitation
Exclusion:
- Patients without transthoracic impedance (TTI) data
Results:
- 287 OHCA patients received at least one defibrillation
- 109 excluded due to none or insufficient data
- The final cohort compromised 178 patients with 523 defibrillations
- Mean age = 68.4 years
- Male = 78.7%
- Initial shockable rhythm = 69.7%
- Bystander CPR = 86%
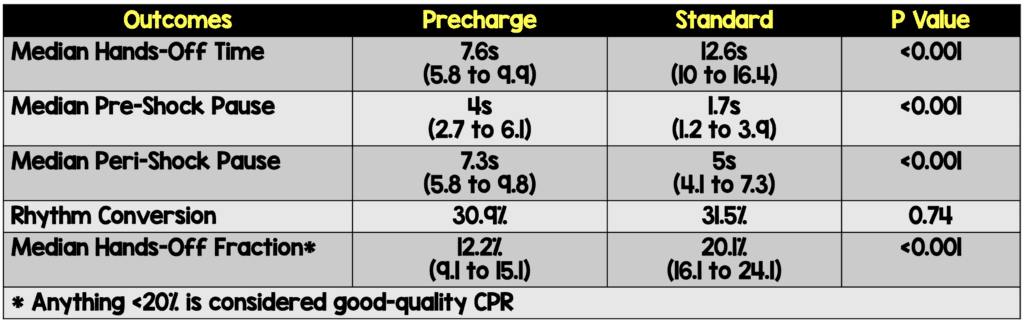
- No difference in post-shock pauses
- Inappropriate shocks delivered to non-shockable rhythms:
- Precharge: 7%
- Standard: 12%
- Old: 5%
Strengths:
- 1st study to demonstrate the impacts of precharging the defibrillator in a prehospital setting
Limitations:
- The impact of pre-charging on patient-oriented outcomes is unclear based on this study (i.e. survival with good neurological outcomes)
- 1/3rd of patients excluded due to either absence of or uninterpretable data
- No data on why one method was performed over another (may reflect some other feature of competency of resuscitation)
- No data on management other than defibrillator
- Potential Hawthorne effect
Discussion:
- Use of the precharge method reduced hands-off time (by 5 seconds) and reduced the total hands-off fraction during resuscitation
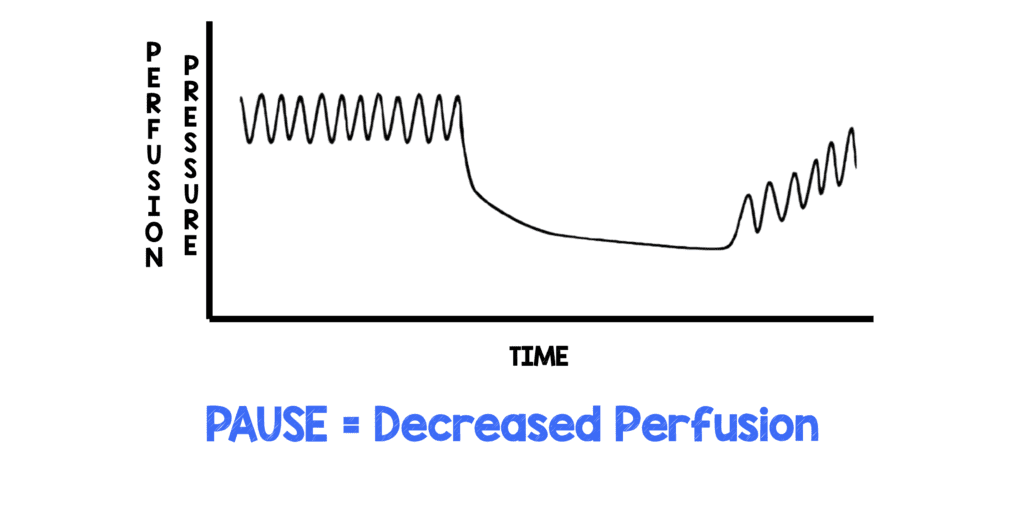
- In the precharge method, as rhythm analysis is done immediately prior to defibrillation the pre-shock pause may increase. Any prolongation of pre- and peri-shock pauses, could be detrimental if resuming chest compressions is delayed. However, in this study, neither the defibrillation method nor the pre-shock pause affected the conversion ratio. Reducing hands-off time and increasing the duration of uninterrupted compression periods between defibrillations may be more important than a 2 second difference in the pre-shock period.
- Interruptions in CPR cause a decrease in cardiac output and ultimately cerebral/coronary perfusion pressure. More importantly the decrease in perfusion pressure is not just during the pause, but is also the time to build the pressure back up (i.e. Decreased coronary perfusion pressure lasts longer than the pause itself). This is important because ischemic cardiomyocytes are less likely to be successfully defibrillated
- Below are two graphics showing the standard way we do rhythm checks vs how pre-charging the defibrillator would look:
Author Conclusion: “The Precharge method reduces hands-off time during defibrillation procedures, reduces the total hands-off fraction and may consequently be associated with increased ROSC rate in OHCA patients with shockable rhythms. The rate of shocks to non-shockable rhythms or accidental shocks were not increased. We propose increased emphasis on pre-charging in future cardiac arrest guidelines. Controlled studies examining patient-level outcomes are warranted.”
Clinical Take Home Point: Precharging the defibrillator reduced hands-off time during defibrillation procedures, as well as the total hands-off fraction which could result in increased ROSC rates in patients with shockable rhythms. Although physiologically sound, a larger trial with patient-oriented outcomes would be needed before changing practice.
References:
- Iversen BN et al. Pre-Charging the Defibrillator Before Rhythm Analysis Reduces Hands-Off Time in Patients with Out-Of-Hospital Cardiac Arrest with Shockable Rhythm. Resuscitation 2021. PMID: 34627866
- Christenson J et al. Chest Compression Fraction Determines Survival im Patients with Out-of-Hospital Ventricular Fibrillation. Circulation 2009. PMID: 19752324
- Cunningham LM et al. Cardiopulmonary Resuscitation for Cardiac Arrest: The Importance of Uninterrupted Chest Compressions in Cardiac Arrest Resuscitation. AJEM 2012. PMID: 22633716
For More on This Topic Checkout:
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post Pre-Charging the Defibrillator Before Rhythm Checks in Cardiac Arrest appeared first on REBEL EM - Emergency Medicine Blog.
