
 Welcome to the October 2015 REBELCast, where Swami, Matt, and I are going to tackle a couple of topics in the world of Trauma, specifically ED Thoracotomy. Now we all know that ED thoracotomy is a last ditch salvage effort, performed under specific clinical circumstances, during a traumatic arrest. The purpose of the ED thoracotomy is to evacuate pericardial tamponade, control hemorrhage, improve coronary/cerebral blood flow, and if needed internal cardiac massage. The purpose of this podcast is to discuss specific indications where this already low yield procedure may have some benefit.
Welcome to the October 2015 REBELCast, where Swami, Matt, and I are going to tackle a couple of topics in the world of Trauma, specifically ED Thoracotomy. Now we all know that ED thoracotomy is a last ditch salvage effort, performed under specific clinical circumstances, during a traumatic arrest. The purpose of the ED thoracotomy is to evacuate pericardial tamponade, control hemorrhage, improve coronary/cerebral blood flow, and if needed internal cardiac massage. The purpose of this podcast is to discuss specific indications where this already low yield procedure may have some benefit.
- Topic #1: FAST US Examination as a Predictor of Outcomes After Resuscitative Thoracotomy
- Topic #2: Blunt Trauma Thoracotomy
REBEL Cast Episode 17: The All Thoracotomy Episode
Click here for Direct Download of Podcast
Topic #1: FAST US Examination as a Predictor of Outcomes After Resuscitative Thoracotomy
Background: In patients who suffer a traumatic cardiac arrest, a final salvage maneuver that is performed in the emergency department is a resuscitative thoracotomy (RT). There are two lines of thought about RT that are on opposite sides of the spectrum. The first line of thought is that if RT is not performed the patient is going to die anyways, so why not try it as a last ditch effort. The second line of thought is that due to the low yield in survival with RT, why expend resources and create a potential risk of harm to providers. The Focused Assessment Using Sonography for Trauma (FAST) has a high sensitivity and specificity for identifying hemopericardium and cardiac activity in a matter of seconds. Since there is really no good way to discriminate between which patients with traumatic cardiac arrest would benefit from RT, maybe adding a bedside FAST could help make this distinction.
What They Did:
- Prospective, Observational Trial in 1 Trauma center in California
- Patients undergoing RT in the Emergency Department
- All penetrating trauma patients with absent vital signs
- All blunt trauma patients with loss of vital signs en route or in the resuscitation bay
- FAST performed just before or concurrently with RT
Outcomes:
- Primary: Survival to discharge or organ donation
- Secondary Outcomes: ROSC
Results:
- 187 patients with traumatic arrest and underwent FAST
- 2% Survived
- 6% Organ Donors
- 2% Expired
- Demographics:
- Median Age 31 years
- 5% Male
- 3% Penetrating Trauma
- If no cardiac motion seen on US à0/126 survived
- If cardiac motion seen on US à9/45 survived or became organ donors
- Only 6 patients (3.2%) survived
- Only 3 patients (1.6%) became organ donors
- Cardiac motion on FAST was 100% sensitive and 73.7% specific for the identification of survivors and organ donors
- Addition of pericardial effusion did not improve sensitivity for the identification of survivors or organ donors
Discussion:
- Providers performing FAST exams completed a 2 day, 16 hour ultrasound course consisting of lectures, hands on training, in addition to at least 2 weeks of proctored training in point of care ultrasound
- Rhee et al did a review of 24 studies with 4620 cases finding an overall survival of 7.4% with normal neurologic outcomes in 92.4% of survivors. This review also looked at survival with:
- Location of injury (Survival 19.4% cardiac vs 10.7% thoracic vs 4.5% abdominal vs 0.7% multiple)
- Mechanism of injury (Survival 8.8% penetrating vs 1.4% blunt)
- Signs of life (Survival 11.5% if present on arrival vs 8.9% if present on transport vs 1.2% if absent in field)
- Author conclusion: No clear single independent pre0perative factor can uniformly predict death
- RT is already a rare procedure and using FAST as this study recommends may further decrease the number of RTs which may make it difficult to maintain the skills necessary for this procedure which could negatively impact the outcomes
Author Conclusion: With a high degree of sensitivity for the detection of potential survivors after traumatic arrest, FAST represents an effective method of separating those that do not warrant the risk and resource burden of RT from those who may survive. The likelihood of survival if pericardial fluid and cardiac motion were both absent was zero.
Clinical Take Home Point: ALL survivors and organ donors had visible cardiac motion on FAST. If no cardiac motion or pericardial effusion was seen on FAST, then survival was zero.
References:
- Inaba K et al. FAST Ultrasound Examination as a Predictor of outcomes After Resuscitative Thoracotomy: A Resuscitative Thoracotomy. Ann Surg 2015; 262 (3): 512 – 8. PMID: 26258320
For More Checkout:
- Thomas D at ScanCrit: FAST Thoracotomy
Topic #2: Blunt Trauma Thoracotomy
Background: Emergency department (ED) thoracotomy after blunt trauma is a very controversial procedure with opinions on both sides of the spectrum. Just to show you how confusing it is you have to look no further than guidelines from different societies. The Western Trauma Association recommends ED thoracotomy after blunt trauma if there are any signs of life or no signs of life with less than 10 minutes of CPR. The Advanced Trauma Life Support (ATLS) course states any patient who is pulseless upon arrival after blunt trauma does not benefit from ED thoracotomy.
What They Did:
- Systematic Review and Meta-Analysis of ED thoracotomy after blunt trauma
- Primary Objective: Do adult patients in cardiac arrest or periarrest after blunt trauma, treated with ED thoracotomy survive and have a good neurologic outcome
Outcomes:
- Mortality
- Neurologic Outcomes
Results:
- 27 articles with 1,369 patients were included in the review (All were case series)
- 13 articles analyzed for meta-analysis
- 21/1,369 (1.5%) patients survived with good neurologic outcome
- All patients had vital signs present on scene or in the ED
- All patients received no more than 11 – 15 minutes of CPR
- 2/500 (0.4%) patients survived with no vital signs at any time
- 100% had bad neurologic outcomes
- Meta-Analysis
- Poor outcome = death or poor neurologic status
- All patients had poor outcome if there were no signs of life or vital signs on scene or signs of life on scene but not in the ED
- If there were vital signs or signs of life present in the ED a poor outcome was still 99.2% (95% CI 96.4% – 99.7%)
Limitations:
- All pertinent studies were case series that were low quality studies due to biases (i.e. randomization, blinding, and control groups)
- The accuracy of the timing of CPR in traumatic arrest may not have been recorded accurately meaning times could have actually been less or a bit longer than what is stated.
- With no comparison group we do not know if a simple pericardiocentesis or transfer to the OR may have resulted in similar or even improved outcomes
- There is a significant amount of heterogeneity between studies in this review in definitions of signs of life or vital signs and when to decide when to perform an ED thoracotomy.
- The majority of the studies included were in large trauma centers where experience in performing ED thoracotomies is more likely than small community centers. Only one study included ED physicians performing thoracotomy in which there were zero survivors.
- Only a single reviewer performed study selection, data extraction, and quality appraisal.
Discussion:
- The heterogeneity in these studies really drives home the point of needing to have a protocol to perform ED thoracotomy with strict inclusion and exclusion criteria. For example excluding patients with non-survivable brain injuries, duration of CPR, and patients with no vital signs on scene.
- A very nice and reasonable algorithm is suggested in this paper for ED thoracotomy in blunt trauma to help eliminate situations in which thoracotomy will clearly not serve any noble benefit while considering patients where benefit may be obtained.
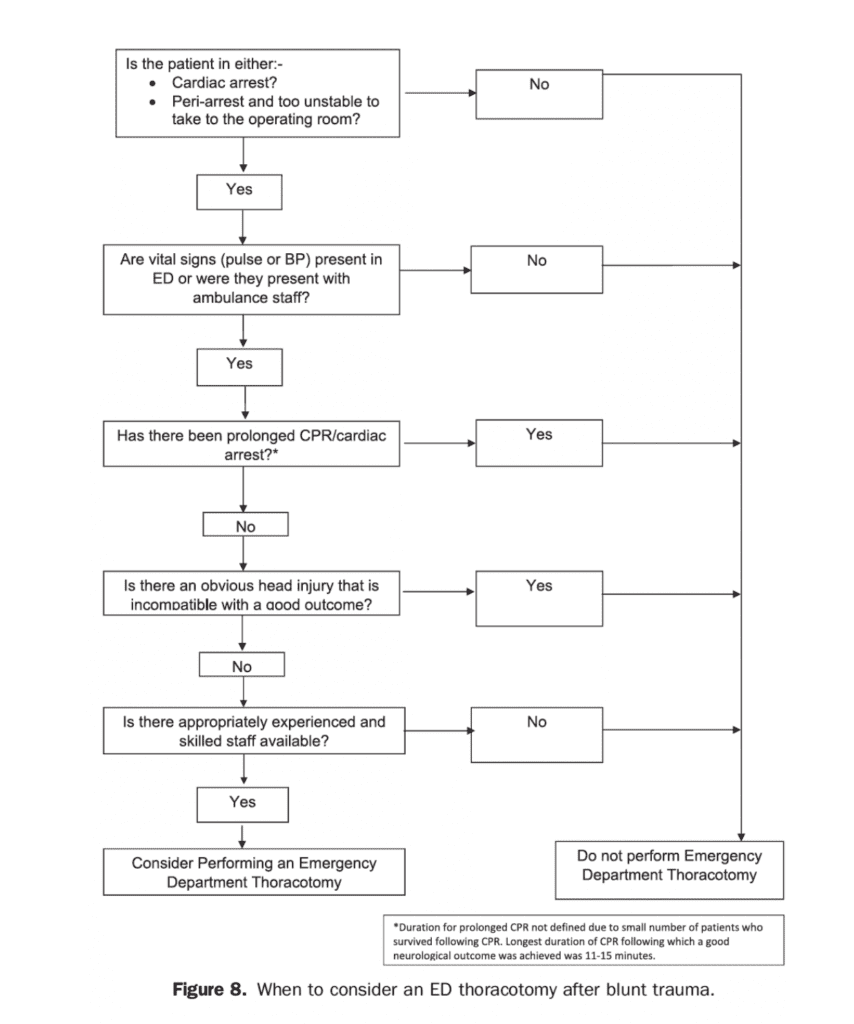
Author Conclusion: There may be a role for ED thoracotomy after blunt trauma, but only in a limited group of patients. Good outcomes have been achieved for patients who had vital signs on admission and for patients who received an ED thoracotomy within 15 minutes of cardiac arrest. The proposed guideline should be used to determine which patients should be considered for an ED thoracotomy, according to level 4 evidence.
Clinical Take Home Point: Although survival rates with good neurologic outcome are low in patients with blunt trauma having undergone ED thoracotomy, there may be some yield to the procedure in patients with vital signs on admission, or ≤15 minutes of CPR. What is clear however, is that in patients with no vital signs at any time or non-survivable head trauma, ED thoracotomy should not be performed.
References:
- Slessor D and Hunter S. To Be Blunt: Are We Wasting Our Time? Emergency Department Thoracotomy Follwing Blunt Trauma: A systematic Review and Meta-Analysis. Ann Emerg Med 2015; 65(3): 287 – 307. PMID: 25443990
For more on what others thought on these topics checkout:
- Thomas D at ScanCrit: FAST Thoracotomy
- Matthew DeLaney at EMLit of Note: Blunt Trauma Thoracotomy – Probably Still Not Time for Heroics
- John Hinds: Crack the Chest. Get Crucified
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami)
The post REBEL Cast Episode 17: The All Thoracotomy Episode appeared first on REBEL EM - Emergency Medicine Blog.
