
 Background: Welcome back to the September 2016 REBEL Cast. We are back with another episode and I am super excited about this episode because we are going to talk about two papers just published in the Resuscitation Journal on management of refractory ventricular fibrillation. It is a well known fact that the cornerstones for survival from Out-Of-Hospital Cardiac Arrest (OHCA) have always been early, high quality CPR and early defibrillation in patients with shockable rhythms (i.e. Ventricular Fibrillation/Ventricular Tachycardia). Some patients with shockable rhythms may be refractory to standard defibrillation therapy (i.e. refractory VF). Even more frustrating, there is truly a dearth of data on what to do with these patients. One strategy that has been reported more and more in the literature is double sequential defibrillation (DSD).
Background: Welcome back to the September 2016 REBEL Cast. We are back with another episode and I am super excited about this episode because we are going to talk about two papers just published in the Resuscitation Journal on management of refractory ventricular fibrillation. It is a well known fact that the cornerstones for survival from Out-Of-Hospital Cardiac Arrest (OHCA) have always been early, high quality CPR and early defibrillation in patients with shockable rhythms (i.e. Ventricular Fibrillation/Ventricular Tachycardia). Some patients with shockable rhythms may be refractory to standard defibrillation therapy (i.e. refractory VF). Even more frustrating, there is truly a dearth of data on what to do with these patients. One strategy that has been reported more and more in the literature is double sequential defibrillation (DSD).
Another issue in cardiac arrest patients is we frequently give boluses of 1mg epinephrine every 3 – 5 minutes as is outlined in the ACLS guidelines. When patients have minimal cardiac output, the buildup of catecholamines may potentially cause refractory ventricular fibrillation (RVF). This could be due to an increase myocardial oxygen consumption causing an increase in myocardial ischemia, and ultimately more difficulty in successful defibrillation. But maybe by blocking the beta-adrenergic receptors in the myocardium, we can block the beta effects of the catecholamines and potentially increase the chances of successful sustained ROSC.
REBEL Cast Episode 28: Refractory Ventricular Fibrillation
Click here for Direct Download of Podcast
Article #1:
- Cortez E et al. Use of Double Sequential External Defibrillation for Refractory Ventricular Fibrillation During Out-of-Hospital Cardiac Arrest. Resuscitation 2016. S0300-9572(16): 30398 – 7. [Epub ahead of print] PMID: 27521470
What They Did:
- Retrospective Chart Review of Ventricular Fibrillation (VF) Patients Treated with DSD
Definitions:
- Refractory VF = VF refractory to 5 single defibrillations
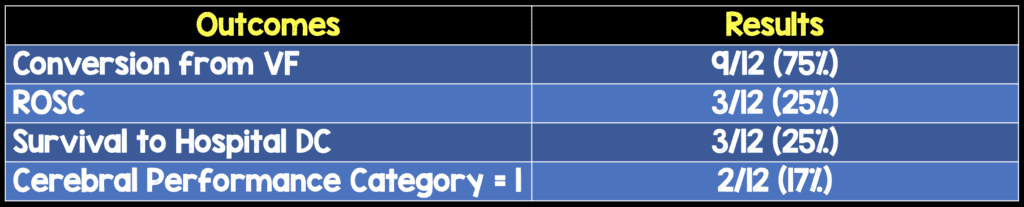
Outcomes:
- Return of Spontaneous Circulation (ROSC)
- Conversion from VF
- Survival to Hospital Discharge
- Cerebral Performance Category Score
Results:
- 2428 OHCA Events Reviewed
- 499 (21%) of patients with shockable rhythm
- 12 (0.5%) patients treated with DSD
- 50% Witnessed Arrests
- 85% Received Bystander CPR
- Median DSD Time = 27 min
- Median Resuscitation Time = 32 min
Limitations:
- Retrospective Case Series with a very small sample size. Would need a much larger sample size for more accurate insights about DSD
- Lack of blinded, randomized-control methodology does not allow for definitive conclusions about DSD
- The cases of refractory VF that did not receive DSD were not included in this study.
- CPR quality parameters were not documented for the patients in this case series. For example, if CPR was done poorly, then it could be less likely patients would survive with good neurologic outcomes despite DSD in refractory VF
Discussion:
- Another case series of 10 patients [2] with refractory VF treated with DSD had zero survivors but there were some key differences between that study and the current study being discussed:
- Median time to DSD: 27min vs 39min
- Median Resuscitation Time: 32min vs 51min
- Another retrospective cohort analysis of 50 patients with refractory VF and DSD [3], there was no statistically significant difference in neurologically intact survival between DSD and standard defibrillation (6% vs 11.4%; p = 0.317)
- It should be clarified that in the literature the method of shock delivery varies due to the fact that without more sophisticated electronic monitoring, it is difficult to confirm whether two shocks were delivered at the same time or just slightly one after the other. It is not clear if one method is superior to the other:
- Simultaneous Shock = At the same time
- Sequential Shock = One after the other
Author Conclusion: “Double Sequential Defibrillation may be another tool to improve neurologically intact survival from OHCA. Further studies are needed to demonstrate direct benefits to patient outcomes.”
Clinical Take Home Point: In patients with refractory ventricular fibrillation, when standard ACLS measures have failed in termination of VF, consideration of other tools such as DSD may be an option, but based on the current evidence it is not clear if DSD improves neurologically intact survival from OHCA.
Article #2:
- Lee YH et al. Refractory Ventricular Fibrillation Treated with Esmolol. Resuscitation 2016. [Epub Ahead of Print]. PMID: 27523955
What They Did:
- Single center retrospective pre-post study of patients with refractory ventricular fibrillation (RVF) receiving esmolol (Loading dose 500ug/kg, infusion 0 – 100ug/kg/min)
Inclusion:
- Age ≥ 18 years
- OHCA with initial VF or VT
- RVF (VF resistant to ≥3 defibrillation, 3mg epinephrine, 300mg of amiodarone, and no ROSC after >10min of CPR)
Exclusion:
- Severe head trauma or acute active bleeding
- Severe sepsis
- VF that developed during resuscitation for initial asystole or PEA
- Terminal stage malignancy
- History of severe neurological deficits (i.e. Dementia, ICH, ischemic stroke with bedridden status)
- Patients who had received beta-blocker therapy before the cardiac arrest
Outcomes:
- Primary: Sustained ROSC (>20 minutes of spontaneous circulation without recurrence of cardiac arrest)
- Secondary:
- Survival to ICU admission and hospital discharge
- Survival with favorable neurological outcomes at 30d, 3 months, and 6 months (used the Glasgow-Pittsburgh Cerebral Performance Category with good outcomes defined as CPC Score of 1 – 2)
Results:
- 41 patients were included in the analysis
- No Esmolol (Control Group) n = 25
- Esmolol Group (Intervention Group) n = 16
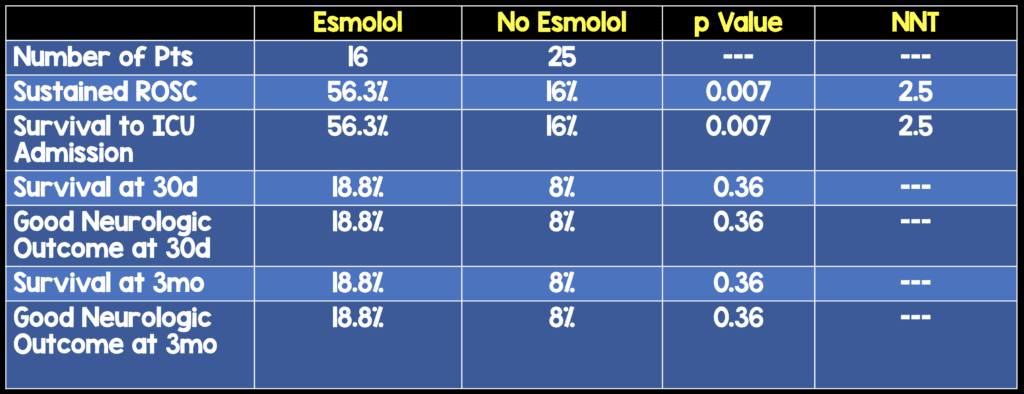
Strengths:
- No significant differences in baseline characteristics and ACLS treatments
Limitations:
- Retrospective nature of this study could cause a selection bias
- Single hospital and very small sample size
Discussion:
- There is not a lot of prospective human evidence on the use of beta blockers in refractory VF:
- Nademanee K et al [4]: 49 patients with electrical storm with the 1 week mortality being higher in patients not receiving beta blockade (82% vs 22% respectively)
- Miwa Y et al [5]: 42 patients with electrical storm in which landiolol, an ultra-short acting beta 1-selective blocker, was used and inhibited electrical storm in 79% of patient’s refractory to class III antiarrhythmic drugs
- The authors of this paper chose esmolol over cavedilol and atenolol for several reasons:
- Cardio-selective beta blocker with short elimination half-life (9 minutes)
- Most animal studies used esmolol and showed better results in terms of longer survival after ROSC, and no VF recurrence
- Although the rate of sustained ROSC was high in this study, only 1/3 of patients survived and had good neurologic outcomes. The authors also mention that this may be due to the long duration of CPR in this study with a median time of 51.5min in the ROSC group
Author Conclusion: “The findings of our study suggest that administration of esmolol may increase the rate of sustained ROSC and ICU survival among patients with RVF in OHCA. Further larger-scale, prospective studies are necessary to determine the effect of esmolol for RVF in OHCA.”
Clinical Take Home Point: In patients with refractory ventricular fibrillation, this study indicates that the use of esmolol resulted in a higher rate of sustained ROSC, but a much larger prospective study will still need to be performed to determine if the surrogate marker of sustained ROSC will translate to longer term survival with good neurologic outcomes.
References:
- Cortez E et al. Use of Double Sequential External Defibrillation for Refractory Ventricular Fibrillation During Out-of-Hospital Cardiac Arrest. Resuscitation 2016. S0300-9572(16): 30398 – 7. [Epub ahead of print] PMID: 27521470
- Cabanas JG et al. Double Sequential External Defibrillation in Out-of-Hospital Refractory Ventricular Fibrillation: A Report of Ten Cases. Prehosp Emerg Care 2015; 19: 126 – 30. PMID: 25243771
- Ross EM et al. Dual Defibrillation in Out-of-Hospital Cardiac Arrest: A Retrospective Cohort Analysis. Resuscitation 2016; 106: 14 – 17. PMID 27344928
- Lee YH et al. Refractory Ventricular Fibrillation Treated with Esmolol. Resuscitation 2016. [Epub Ahead of Print]. PMID: 27523955
- Nademanee K, Taylor R, Bailey WE, Rieders DE, Kosar EM. Treating electrical storm :sympathetic blockade versus advanced cardiac life support-guided therapy. Circulation 2000; 102: 742-7. PMID: 10942741
- Miwa Y et al. Effects of landiolol, an ultra-short-acting beta 1-selective blocker, on electrical storm refractory to class III antiarrhythmic drugs. Circ J 2010; 74: 856 – 63. PMID: 20339194
For More Thoughts on These Topic Checkout:
- Salim Rezaie at REBEL EM: Beyond ACLS – Dual Simultaneous External Defibrillation
- Jess Mason at EM:RAP: Double Sequential Defibrillation
- CORE EM: Proper Defibillator Pad Placement + Dual Sequential Defibrillation
- Cliff Reid at Resus.ME: Esmolol for Refractory VF
- The Resus Room: Double Sequential Defibrillation
- Sameer Sharif at CanadiEM: My Heart Goes Boom…Beta Blockers in Cardiac Arrest
Post Peer Reviewed By: Matt Astin (Twitter: @mastinmd)
The post REBEL Cast Episode 28: Refractory Ventricular Fibrillation appeared first on REBEL EM - Emergency Medicine Blog.
