
 Take Home Points
Take Home Points
- Patients with severe hypercalcemia (> 14 mg/dL) are at risk for severe cardiac dysrhythmias and cardiac collapse
- Treatment centers on volume repletion with normal saline with consideration for the addition of loop diuretics AFTER volume reexpansion is complete
- As the patient begins to diurese, continually monitor electrolytes
REBEL Core Cast 87.0 – Hypercalcemia
Definition: A serum calcium level > 10.5 mg/dL.
Background
Causes
- Malignancy (multiple myeloma, metastases to bone)
- Granulomatous disease (TB, sarcoidosis)
- Endocrine (hyperthyroidism, hyperparathyroidism, adrenal insufficiency, pheochromocytoma)
- Pharmacologic agents (thiazide diuretics, milk-alkali syndrome, PTH therapy for osteoporosis, lithium, Vitamin A)
- Miscellaneous (Dehydration, rhabdomyolysis, prolonged immobilization, dietary, iatrogenic)
Clinical Manifestations
- “Stones (renal), Bones (bone pain), Groans (abdominal pain) + Moans (Psychiatric overtones)”
- Cardiac Effects
- Bradydysrhythmias
- AV block
- Sinus Arrest
- Atrial Fibrillation
- Ventricular Tachycardia
- QTc shortening
- Neuropsychiatric Disorders
- Major: AMS, seizures, weakness, lethargy, coma
- Minor: Anxiety, depression, confusion, hallucinations
- Hyporeflexia
Diagnosis
- Serum calcium > 10.5 mg/dL
- 10.5 – 12.0 mg/dL considered moderate
- > 14 mg/dL considered severe + potentially life-threatening
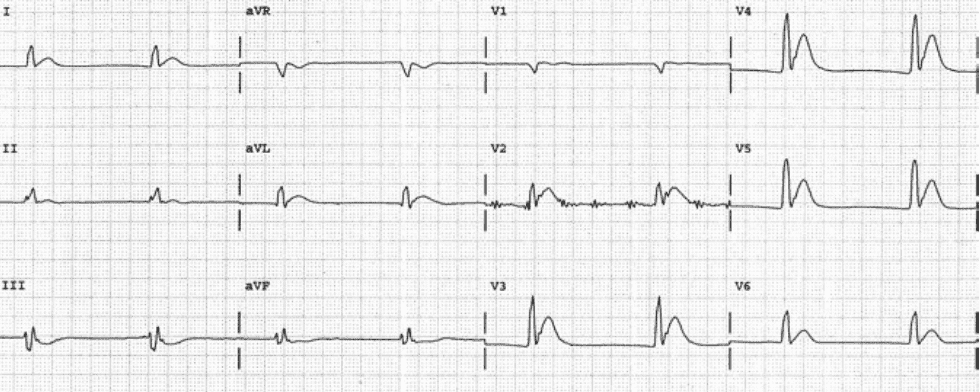
- EKG
- Short QTc interval (also caused by congenital short QT syndrome and digoxin)
- Prolonged PR
- Widened QRS complex
- AV block
Management
- Supportive Care – ABCs, IV, O2, Monitor
- Volume Expansion
- The majority of patients with hypercalcemia have significant dehydration
- Normal saline administration
- Mechanism of action: Corrects volume depleted state and inhibits proximal tubule calcium resorption
- Monitor other electrolytes (potassium, sodium)
- Dose
- Bolus to correct hypotension
- Careful administration while monitoring overall fluid status (patients often have cardiac and/or renal dysfunction making them susceptible to volume overload)
- Loop diuretics (i.e. furosemide)
- Mechanism of action: Inhibits reabsorption of Na,K, Cl via the Na+-K+-2Cl– cotransporter in the thick ascending loop of henle, thereby also inhibiting Ca2+ and Mg2+ reabsorption
- Theoretical benefit of “forced diuresis” not proven in the literature
- Should NOT be given until volume repletion completed as it can exacerbate hypercalcemia in this situation
- Bisphosphonates
- Mechanism of action: inhibit osteoclast-mediated bone resorption
- Zoledronic acid
- Preferred in hypercalcemia in the setting of malignancy
- Dose: 4 mg IV over 15 minutes
- Other Agents: Pamidronate, Etidronate
- Calcitonin
- Mechanism of action: inhibits Ca2+ absorption in the intestines, inhibits osteoclast activity, stimulates osteoblastic activity, inhibits renal tubular cell reabsorption
- Dose: 4 IU/kg IM Q12
- Cinacalcet
- Mechanism of action: increases the sensitivity of Ca2+ receptors on parathyroid cells to reduce PTH levels and, thus Ca2+ levels
- Indications: Hypercalcemia in patients with secondary hyperparathyroidism (i.e. CKD on dialysis, parathyroid carcinoma)
- Other
- Hemodialysis
- Parathyroidectomy may be considered in patients with hypercalcemia caused by hyperparathyroidism
Take Home Points
- Patients with severe hypercalcemia (> 14 mg/dL) are at risk for severe cardiac dysrhythmias and cardiac collapse
- Treatment centers on volume repletion with normal saline with consideration for the addition of loop diuretics AFTER volume reexpansion is complete
- As the patient begins to diurese, continually monitor electrolytes
References
Pfenning CL, Slovis CM: Electrolyte Disorders; in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 8. St. Louis, Mosby, Inc., 2014, (Ch) 125: p 1636-53.
Read More
- LITFL: QT Interval
- LITFL: Hypercalcemia
- LITFL: Hypercalcemia
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post REBEL Core Cast 87.0 – Hypercalcemia appeared first on REBEL EM - Emergency Medicine Blog.
