
 Mechanical Ventilation is a modality commonly used in the critically ill, but many providers, may not have a strong understanding of the basics. Emergency Medicine and Critical Care Physicians need to have a firm grasp of the basic concepts of mechanical ventilation because without it, we can do serious harm to our patients. Airway management is not complete once the endotracheal tube is placed through the cords, and the proper selection of both the ventilator mode and initial settings is essential to ensure your patient has the best possible outcomes. You should not simply rely on the respiratory therapist to know your patients physiology. Clear communication with your therapist about the patient’s physiology and initial ventilator setting is crucial.
Mechanical Ventilation is a modality commonly used in the critically ill, but many providers, may not have a strong understanding of the basics. Emergency Medicine and Critical Care Physicians need to have a firm grasp of the basic concepts of mechanical ventilation because without it, we can do serious harm to our patients. Airway management is not complete once the endotracheal tube is placed through the cords, and the proper selection of both the ventilator mode and initial settings is essential to ensure your patient has the best possible outcomes. You should not simply rely on the respiratory therapist to know your patients physiology. Clear communication with your therapist about the patient’s physiology and initial ventilator setting is crucial.
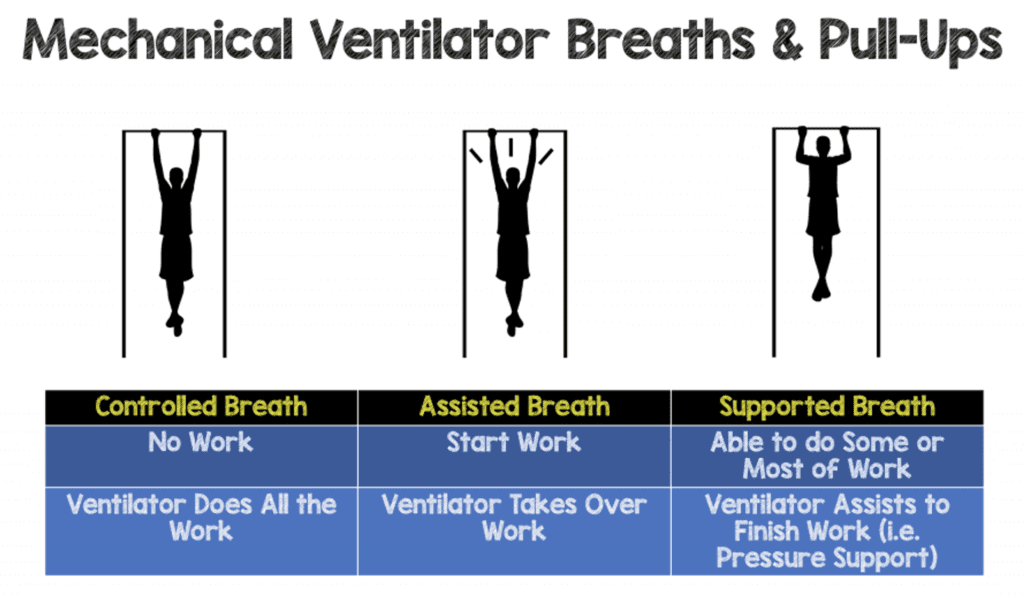
Instead of going through all the various modes and learning them individually as most ventilator talks do, let’s try something different. Let’s first learn the 3 possible types of breaths your patient can receive on a ventilator and the 2 ways these breaths can be delivered. If you understand these concepts, then you can deconstruct almost any mode of mechanical ventilation and have a clearer understanding of how to use them. There are many modes that exist, but I suggest you learn a few, get to know them well, and when to apply each to your patient.
REBEL Crit Cast Ep6.0 – Mastering Mechanical Ventilation Part 1
Three Types of Breaths
Controlled Breaths:
These types of breaths are completely controlled by the ventilator. We never set up a ventilator to give only controlled breaths, but patients will receive these types of breaths. Controlled breaths are not triggered or initiated by a patient’s effort but are delivered by the ventilator at a set time interval.
Controlled breaths are delivered to patients if they are heavily sedated, paralyzed or the ventilator rate is set higher than a patient is wanting to breath.
Patients can receive either a pressure controlled or volume controlled breath depending on the breath type or mode selected.
Assisted Breaths:
If you understand an assist in sports, you will understand an assisted breath. When you pass the ball to your teammate, you initiate the process but it’s up to your teammate to score the basket or goal. During an assisted breath the patient trigger’s or initiated the breath. Once the breath is triggered or initiated, a breath is then delivered by the ventilator like a control breath. The only difference between a controlled and an assisted breath is that assisted breaths are initiated by the ventilator and controlled breaths are initiated by time. After these breaths are initiated, they are essential identical.
Patients can receive either a pressure assist or volume assist breath depending on the breath type or mode selected.
Spontaneous (Supported) Breaths:
Spontaneous breaths are like assisted breaths where they are initiated or triggered by the patient however, once triggered, the patient performs some work/effort during the breath but does get support from the ventilator.
Patients can receive a pressure support of volume support breath depending on the mode selected. A pressure supported breath would give a set pressure to support a patient’s spontaneous breaths in order to achieve a desired tidal volume. If the tidal volume is too high, then the support can be decreased or too low then the pressure support can be increased. A volume support breath is a newer type of spontaneous breath where a desired tidal volume is preset and the pressure is automatically adjusted up or down by the ventilator to help the patient achieve the preset tidal volume.
Breath Delivery
Volume Breath:
Volume breaths deliver a set tidal volume (set by the clinician) however the pressure needed to deliver this tidal volume can vary. The pressure needed to deliver these volume breaths depends on compliance or the “stiffness” of the lungs. Compliance is simply the change in volume/change in pressure. Low compliance or “stiff” lungs (ex. ARDS) may mean that higher pressures are required to deliver the volume of gas (tidal volume) to the patient. High compliance or “stretchy” (ex. emphysema) may mean that less pressure is required to deliver the volume of gas (tidal volume).
Pressure Breath:
Pressure breaths deliver a set pressure (set by the clinician) however now the tidal volume can vary depending on compliance. The tidal volume delivered for a set pressure will vary depending on the compliance of the lungs. As mentioned above, low compliance or “stiff” lungs may mean that that more pressure may be required to deliver an adequate tidal volume. High compliance or “stretchy may mean that less pressure is required to deliver an adequate tidal volume.
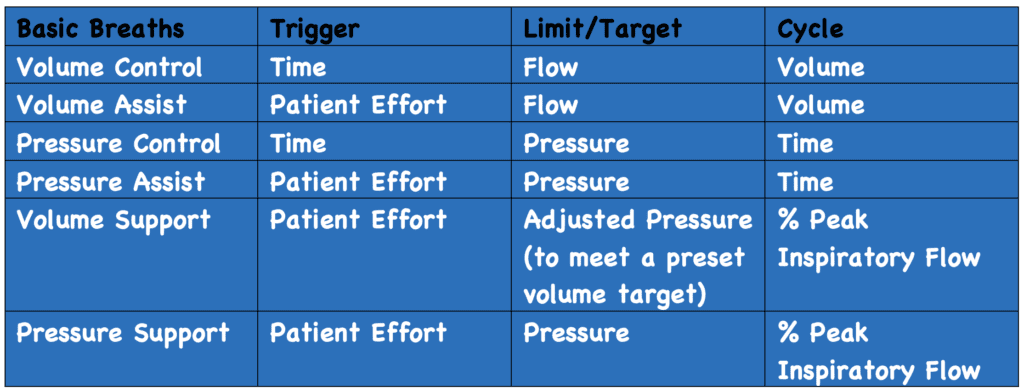
Trigger, Limit (Target), & Cycle
Trigger:
Trigger is how a breath is initiated. There are 3 main ways a breath can be initiated: time, flow, or pressure. Controlled breaths are time triggered and are initiated at a set time interval.
Assisted breaths and spontaneous breaths are triggered by either a pressure or flow trigger. Once the ventilator detects a change in pressure or flow in the circuit (initiated by the patient) the breath will be delivered. A flow trigger is more commonly used and is generally easier and more comfortable for the patient. Flow triggers can occasionally lead to a phenomenon known as autotriggering (discussed below). A pressure trigger can also used but can be more difficult for a patient to trigger and therefore less comfortable.
Autotriggering
Autotriggering is a type of ventilator dyssynchrony that occurs when the ventilator is triggered by something else rather than the patient. It occurs using flow triggering and may be caused by water or air leaks in the circuit or cardiac oscillations. If you suspect autotriggereing you may have to suction out the water in the tubing, correct any leaks or switch to a pressure trigger to make it more difficult for a breath to be initiated.
Limit (Target):
This is the variable that you want to achieve or sustain during the breath and not exceed.
The target in a volume breath is flow (Volume/Time) and the target in a pressure breath is pressure.
If the patient is receiving a volume control or volume assist beath, the limit is flow. The flow rate will determine how long that breath will last. You can make the breath go faster with higher flow rate or slower by decreasing the flow rate. Regardless the flow rate is maintained until the set tidal volume is achieved.
In pressure modes, the breath will maintain a set pressure. In a pressure control, pressure assist, or a spontaneous pressure supported breath a set pressure will be maintained.
Cycle:
Cycle is what terminates the breath or what ends the inspiratory cycle and what begins expiration. In volume breaths it’s going to be a set tidal volume. So once that tidal volume is delivered to the patient, then the ventilator is going to cycle into an exhalation.
In pressure control or pressure assist breath that’s going to be time. The breath will maintain or target a set pressure for a set time period and once the set time is reached, the inspiratory breath will terminate, and exhalation will begin. A spontaneous pressure supported breathe will terminate once a certain % of peak inspiratory flow rate is achieved (usually 25% of peak inspiratory flow). The only difference between a pressure assist and controlled breath and a spontaneous pressure supported breath is that in a pressure supported breath, inspiratory flow is the cycle.
Guest Post By
John Paul Papadopoulos, MD
Fellow, Critical Care Medicine
Geisinger Medical Center
Danville, PA
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post REBEL Crit Cast Ep6.0 – Mastering Mechanical Ventilation Part 1 appeared first on REBEL EM - Emergency Medicine Blog.
