
 Background: A resuscitative thoracotomy is a time-critical high acuity, low occurrence (HALO) procedure – as an emergency physician you need to know how to do it, but depending on your practice environment, it may be a once-in-a-career maneuver. All the more reason that, if you have to do it, you want to make sure your effort counts.
Background: A resuscitative thoracotomy is a time-critical high acuity, low occurrence (HALO) procedure – as an emergency physician you need to know how to do it, but depending on your practice environment, it may be a once-in-a-career maneuver. All the more reason that, if you have to do it, you want to make sure your effort counts.
In a prior post, I advised that if you’re going to be doing a thoracotomy as an EM doc, you should do a clamshell approach. This was based both on some evidence from the surgical literature as well as personal experience – I feel the clamshell gives you the exposure you really need if you are doing this rarely and the time difference compared to an anterolateral approach is negligible.
A recent paper from Newberry et al. (published ahead of print in Annals of Emergency Medicine) addresses this very issue – from an EM perspective.
Paper: Newberry R et al. Prospective randomized trial of standard left anterolateral thoracotomy versus modified bilateral clamshell thoracotomy performed by emergency physicians. Annals of Emergency Medicine 2020. PMID: 32807537
Clinical Question: What is the optimal technique for the nonsurgical specialist to perform a resuscitative thoracotomy?
What They Did:
- Prospective randomized cross-over trial
- EM senior residents (PGY 2 or 3) and attendings at a single level 1 trauma center were initially provided specific standardized training on both traditional left anterolateral thoracotomy (LAT) and modified clamshell thoracotomy (MCT).
- Study participants were randomized using electronic randomization software to perform both LAT and MCT on separate fresh, nonfrozen human cadavers with a 30-minute “washout” period in between attempts
- Bilateral thoracostomies were performed by the investigators prior to commencement of intervention
- Cadavers were reviewed by a board-certified surgeon to determine success, which was defined as (a) complete delivery of the heart and (b) 100% occlusion of the descending thoracic aorta
- Study participants then were asked to identify key anatomical structures (phrenic nerve, atria and ventricles of the heart, pulmonary hilum, descending thoracic aorta, and the esophagus)
- A survey was completed by participants afterwards to evaluate perceived difficulty, quality of view obtained, physician comfort with each technique, and procedural preference
- No feedback was given to the participants until completion of the entire study protocol
Outcomes:
- Primary: Time to successful completion of the resuscitative thoracotomy
-
Secondary Included:
- Successful exposure of the heart
- Successful cross-clamping of the descending thoracic aorta
- Successful procedural completion
- Time to exposure of the heart
- Time to cross-clamp placement
- Number and type of iatrogenic injuries
- Correct identification of anatomic structures
Inclusion:
- Emergency medicine physician, either:
- Senior resident (PGY2 or PGY3)
- Attending
Exclusion:
- Unwillingness to participate
Results:
- A power analysis was conducted a priori indicating a sample size of 28 (14 pairs) would be sufficient to identify a 60-second time difference using a paired t test with 80% power
- Initial assumption was that all participants would be successful. However, this would have only included 4 participants. Therefore, the model was changed to allow inclusion of failures.
- 15 total participants
- Mean age 34.5 years
- Male 80%
- Seniority:
- 3rd year resident – 47%
- Attending physician – 53%
- Median years post-residency – 2.5 years (IQR 1.5-5.5 years)
- Prior experience
- LAT
- 3-15 simulated
- 60% had done a therapeutic procedure
- MCT
- No simulated or therapeutic experience
- LAT
- Median time from training to data collection – 25 days (IQR 8-67 days)
-
Success of procedure
- Overall success
- LAT 40%
- MCT 67%
- Difference –27%; 95% CI –61% to 8% – no statistically significant difference
- Success of procedure by attending physicians
- LAT 25%
- MCT 88%
- Difference 63%; 95% CI 9 to 92% – statistically significant difference favoring MCT
- Mean time to successful procedure completion
- LAT 6 minutes 6 seconds (SD 2 minutes 34 seconds)
- MCT 6 minutes 18 seconds (SD 2 minutes 15 seconds
- Hazard ratio 0.5, 95% CI 0.2-1.4 – no statistically significant difference
- Overall success
-
Exposure of the heart
- Overall success
- LAT 73%
- MCT 87%
- Difference -14%; 95% CI -45% to 18%
- Mean time to exposure of the heart
- LAT 4 minutes 9 seconds (SD 1 minute 31 seconds)
- MCT 4 minutes 35 seconds (SD 1 minute 57 seconds)
- Hazard ratio 1.0; 95% CI 0.5 to 2.3
- Overall success
-
Cross-clamping of the aorta
- Overall success
- LAT 60%
- MCT 80%
- Difference -20%; 95% CI -47% to 7%
- Mean time to cross-clamping of the aorta
- LAT 6 minutes 37 seconds (SD 2 minute 13 seconds)
- MCT 6 minutes 15 seconds (SD 2 minute 2 seconds)
- Hazard ratio 0.7; 95% CI 0.4 to 1.1
- Overall success
- All structures correctly identified
- Overall
- LAT 40%
- MCT 67%
- Difference -27%; 95% CI -56 to 2
- Median percentage of structures identified
- LAT 87.5% (IQR 87.5-100%)
- MCT 100% (IQR 87.5-100%)
- Difference 0%; 95% CI -9.5% to 2.8%
- Overall
- Absence of iatrogenic injury (rib fractures, lacerations to diaphragm, esophagus, lung or heart)
- Overall
- LAT 0%
- MCT 33%
- Difference -33% 95% CI -57% to -9%
- Median number of injuries per procedure
- LAT 1 (1-4)
- MCT 1 (0 to 3)
- Difference 1; 95% CI 0 to 1 – significantly higher in LAT
- Overall
- Preference of technique based on post-trial questionnaire
- LAT 13%
- MCT 87%
- Difference 74%; 95 CI 23% to 97% – significant in favor of MCT
Strengths:
- Few papers have looked at the outcomes of non-surgeon physicians performing thoracotomies
- Significant effort was made to train participants in the procedure prior to data collection
- Study outcomes were determined by the same board-certified general surgeon who was present during all data collection to avoid any issue of interrater reliability
- No feedback was given between procedures until the completion of data collection
- Study participants were well balanced at baseline
- The study authors looked at iatrogenic injury, of which there has been little to no mention or review in prior work on this topic
Limitations
- The trial was conducted at a single center which trained military physicians. These physicians may have had more exposure in general to trauma than their other civilian counterparts which could have affected their proficiency in this particular procedure. Hence it may not be generalizable to other physician groups
- All participants had prior training and experience with the LAT technique, but none had prior training or experience with the MCT approach. This could bias results in favor of the LAT technique.
- Despite performing a power calculation, their sample size was not large enough to meet true statistical power
- Cadavers were utilized which were of varying quality and may have suffered from varying pathophysiologic changes that could have affected anatomy
- A key step in the procedure (thoracostomy) was already performed for the participants prior to the study.
- Identification of the correct interspace to proceed is a crucial step in the procedure and can add time, which was not accounted for
- Not proceeding in the right anatomical space can contribute to iatrogenic injury
- The criteria for success included 100% occlusion of the aorta. This was not met in many cases and hence the original model was altered to account for this. This can skew the results
- The outcome of physician level and procedural success was an unplanned subgroup analysis
- Potential for risk to the proceduralist was not accounted for in this study
Discussion:
- This study is one of the few to look at non-surgeon perform resuscitative thoracotomy utilizing the traditional LAT as well as the MCT, which has been used with success in other systems by non-surgeons.
- The authors report the time required to perform either a LAT or MCT is similar.
- This is similar to prior published literature on this topic
- Attending physicians may actually have better success in this procedure, and could theoretically perform it faster than senior resident physicians
- This may be particularly relevant at non-academic centers where attending physicians do more procedures themselves as opposed to supervising residents
- The perception of ease of MCT over LAT is important
- A new approach to a procedure may be met with challenges of having to learn a technique people are not familiar with
- This study shows that with simple training, the procedure can be completed largely appropriately and is perceived to be easier than the traditional LAT
- The anatomical exposure is improved with MCT versus LAT (something I alluded to in my previous post)
- This is critical in a situation where the person performing this HALO procedure has to rapidly be able to identify where the problem lies
- The improved identification of anatomy may have predisposed to the lower iatrogenic injury rate with MCT over LAT
- Iatrogenic injury is an important aspect to factor in.
- Little to no studies prior to this one have focused on the incidence of iatrogenic injuries
- Anecdotal evidence is that the incidence is overall low
- Some injuries e.g. a rib fracture may not carry much clinical significance down the line – we see this with effective closed chest compressions and those who survive can have this issue addressed
- Esophageal injuries, though relevant, will be difficult to assess unless the patient survives
- Ultimately, the patient needs to survive to have a complication. This does not mean one can be complacent about causing injury – this is where training is important. However, ultimately you are doing this procedure because the person in front of you has died. Your goal is to restore life. As one of my mentors once said, “There is little that you can do with this procedure that we (the surgeons) cannot fix.”
- This advantage of exposure must be weighed with the potential downrange risk of physiologic disturbance (should the patient survive) of not only having their thoracic cavity opened, but opened through a much large incision than with LAT
- I would liken this to telling my residents not to make a cosmetic incision for a finger thoracostomy when they are trying to save someone’s life. A larger incision to allow the necessary intervention (in this instance highly dependent on the operator being able to actually accurately identify the anatomical injury) is critical to saving this patient’s life
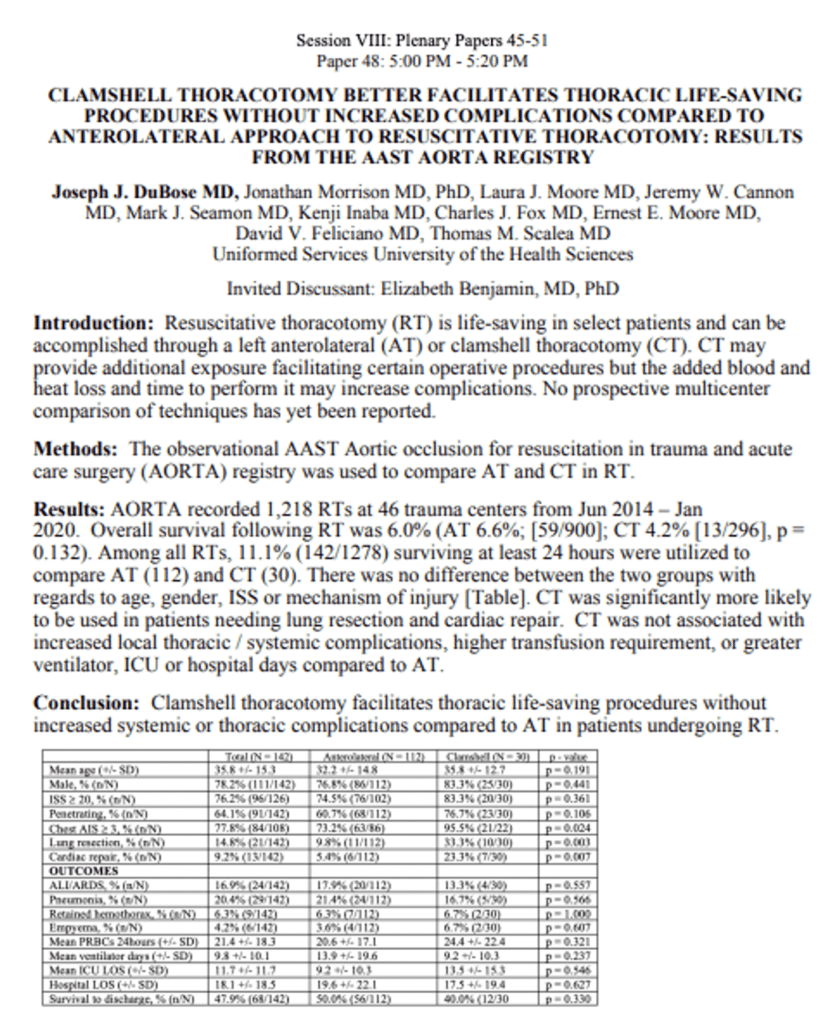
- An abstract being presented at this year’s American Association for the Surgery of Trauma’s Annual Meeting reports there are no increased systemic or thoracic complications when compared to LAT
Author Conclusion: “Resuscitative thoracotomy success rates were lower than expected in this capable subject population. Success rates and procedural time for the MCT and LAT were similar. However, the MCT had a higher success rate when performed by staff emergency physicians, resulted in less periprocedural iatrogenic injuries, and was the preferred technique by most subjects. The MCT is a potentially feasible alternative resuscitative thoracotomy technique that requires further investigation.”
Clinical Take Home Point: When faced with a time-critical injury amenable to resuscitative thoracotomy, the emergency physician has precious little opportunity to make a difference in outcome. Therefore, they should adopt the technique that will most likely allow success. This paper shows that for this HALO procedure, the MCT allows timely access to the chest, provides the best exposure to attempt to fix the problem, and decreases the risk of iatrogenic injury. It should be strongly considered by the emergency physician having to perform this while working within the right system to support this procedure.
References:
- Flaris AN, et al. Clamshell incision versus left anterolateral thoracotomy. Which one is faster when performing a resuscitative thoracotomy? The tortoise and the hare revisited. World J Surgery 2015. PMID: 25561192
- Newberry R et al. Prospective randomized trial of standard left anterolateral thoracotomy versus modified bilateral clamshell thoracotomy performed by emergency physicians. Annals of Emergency Medicine 2020. PMID: 32807537
- Puchwein P et al. Clamshell thoracotomy and open heart massage – a potential life-saving procedure can be taught to emergency physicians: an educational cadaveric pilot study. Injury 2015. PMID: 26068645
- Qasim Z. If you’re going to do the thoracotomy…do a clamshell. REBELEM 2019.
- Wise D et al. Emergency thoracotomy: “how to do it.” Emerg Med J 2005. PMID: 15611536
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post Resuscitative Thoracotomy: What Really is the Quickest Way to a Person’s Heart? appeared first on REBEL EM - Emergency Medicine Blog.
