
 Background:There are two trains of thought in using transthoracic direct current cardioversion (DCCV) when it comes to converting atrial fibrillation. The first is an escalating energy approach which allows cardioversion to occur at the lowest energy for each individual patient and potentially decrease post-shock arrhythmias. The second train of thought is to start at the highest energy approach in order to minimize total number of shocks delivered and duration of the procedural sedation. There is a considerable variation in practice that exists as I recently discovered based on conversations on social media. The authors of this study aimed to compare an escalating energy protocol starting at 100J with a non-escalating energy protocol of 200J to establish the efficacy and safety of both practices of cardioversion using biphasic DCCV of atrial fibrillation.
Background:There are two trains of thought in using transthoracic direct current cardioversion (DCCV) when it comes to converting atrial fibrillation. The first is an escalating energy approach which allows cardioversion to occur at the lowest energy for each individual patient and potentially decrease post-shock arrhythmias. The second train of thought is to start at the highest energy approach in order to minimize total number of shocks delivered and duration of the procedural sedation. There is a considerable variation in practice that exists as I recently discovered based on conversations on social media. The authors of this study aimed to compare an escalating energy protocol starting at 100J with a non-escalating energy protocol of 200J to establish the efficacy and safety of both practices of cardioversion using biphasic DCCV of atrial fibrillation.
What They Did:
- This was a prospective multicenter randomized trial enrolling 380 patients with persistent atrial fibrillation. Patients were randomized to either an escalating energy protocol (100J, 150J, 200J, 200J) or a non-escalating energy protocol (200J, 200J, 200J). Patients would be given a minimum of 1 minute between each successive shock and a successful cardioversion was defined as sustained normal sinus rhythm for at least 30 seconds. Cardioversion was performed using a biphasic waveform, all patients fasted overnight, and were on at least 4 weeks of warfarin before having DCCV. Sedation was with either IV midazolam or IV propofol.
Outcomes:
- The primary outcome of this study was not clearly stated, but the main outcomes reported on were: shock success, number of shocks, cumulative energy, amount of sedation, duration of the procedure, and post-shock arrhythmias.
Inclusion:
- History of persistent atrial fibrillation
- Referred for outpatient DC cardioversion of atrial fibrillation
Exclusion:
- Inadequate anticoagulation (at least 4 weeks prior to procedure)
- Known intracardiac thrombus
- Significant electrolyte imbalance
- Digoxin toxicity
- Cardiogenic shock
- Refractory pulmonary edema
- Uncontrolled thyrotoxicosis
- Pregnancy
- Permanent pacemaker
- Mental condition not allowing informed consent
Results:
- 380 patients were recruited, 193 patients were randomized to an escalating energy protocol and 187 were randomized to a non-escalating protocol. The mean BMI in this study was 28 kg/m2. There were no baseline differences between groups.
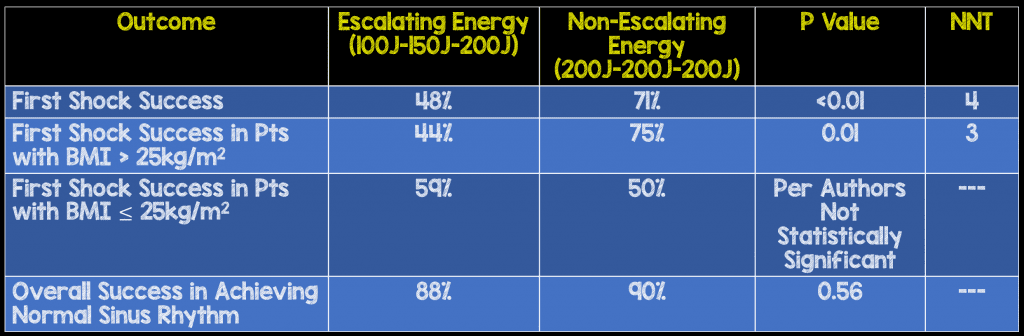
- Use of a non-escalating protocol resulted in fewer shocks (1.46 shocks vs 1.88 shocks) but with a higher cumulative energy (251 J vs 201 J). It is unclear to me whether either of these outcomes is truly clinically significant.
- There was no difference in duration of procedure (Mean of 4 minutes), amount of sedation administered, or post-shock arrhythmia between groups
Strengths:
- The obvious strength of this study is that it was a prospective multicenter randomized trial that asks a clinically important question for both providers and patients. Of note this is the first randomized trial that I am aware of comparing escalating vs non-escalating doses of electricity in successful cardioversion of atrial fibrillation.
Limitations:
- The biggest limitation of this study was in regards to the duration of atrial fibrillation and the follow up for these patients. Although the duration of atrial fibrillation did not have any influence on efficacy of shocks, these are not the patients we are attempting cardioversion for in the ED. The patient population we are treating generally need to have <48hrs of symptoms and good follow up (which is not always possible for uninsured patients) for this to be a feasible practice.
Discussion:
- Biphasic cardioversion is superior to monophasic cardioversion in terms of efficacy at lower energies, post-shock arrhythmias, fewer skin burns, and myocardial stunning.So if you have your choice, go biphasic over monophasic all the way.
- In patients with BMI > 25 kg/m2 starting at 200 J is more efficacious, but in patients with “normal” BMI of ≤25kg/m2 there was no difference whether you started at 100J or 200J. This makes anatomic sense as there is more distance to traverse and less energy getting to the atria for the cardioversion. So in these patients consider starting at 100J, but no one would fault you if you just wanted to do 200J across the board, and it’s just easier to remember.
- In regards to pad placement, a systematic review of 5 trials using biphasic machines published in Academic Emergency Medicine in 2014 [2], showed that pad placement was not a critically important factor in successful cardioversion. There were some important limitations to this review including a small number of trials, small patient populations, no studies investigating recent onset atrial fibrillation, and large variations in study protocols. Personally, I prefer anterior-posterior pad placement as opposed to anterior-lateral (apical) pad placement as this gives the maximum conduction and the shortest distance for the electricity to travel
Author Conclusion: “First-shock success was significantly higher, particularly in patients with a BMI > 25kg/m2, when non-escalating initial 200J energy was selected. The overall success, duration of procedure, and amount of sedation administered, however, did not differ significantly between the two protocols.”
Clinical Take Home Point: In patients with persistent atrial fibrillation being evaluated for electrical cardioversion, using a non-escalating 200J first shock strategy, with biphasic machines has a higher success at conversion to normal sinus rhythm with no difference in duration of procedure, amount of sedation administered, or post-shock arrhythmias compared to an escalating (100J – 150J – 200J) shock strategy. Persistent atrial fibrillation is much more likely to not respond to electricity at lower doses where as in patients with new onset atrial fibrillation (<48hrs), lower doses may be feasible as these patients are more likely to be electro-sensitive.
References:
- Glover BM et al. Biphasic Energy Selection for Transthoracic Cardioversion of Atrial Fibrillation. The BEST AF Trial. HEART 2008. PMID: 17591649
- Kirkland S et al. The Efficacy of Pad Placement for Electrical Cardioversion of Atrial Fibrillation/Flutter: A Systematic Review. Acad Emerg Med 2014. PMID: 25117151
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami)
The post The BEST AF Trial: What is the Optimal Energy Selection for Cardioversion in Patients with Afib? appeared first on REBEL EM - Emergency Medicine Blog.
