
 Background: Prior to the discovery of thrombolytics, clinicians could only observe their patients completing their myocardial infarctions and then classify them according to whether their subsequent ECGs developed Q waves. When trials showed a clear survival benefit with thrombolytics (especially in STE) this shifted the paradigm from “Q-wave/ non Q-wave MI” to “STEMI / non-STEMI”. Eventually STEMI became synonymous with acute coronary occlusion (ACO) requiring reperfusion, except this connection was never studied in trials. Unfortunately, the STEMI criteria have limited diagnostic criteria for ACO, leading to false cath lab activation. And worse, missing ⅓ of ACO (NSTEMI), depriving them of emergent reperfusion therapy. This led many authors to shift from STEMI/ NSTEMI to ACO-MI/ non- ACO-MI.
Background: Prior to the discovery of thrombolytics, clinicians could only observe their patients completing their myocardial infarctions and then classify them according to whether their subsequent ECGs developed Q waves. When trials showed a clear survival benefit with thrombolytics (especially in STE) this shifted the paradigm from “Q-wave/ non Q-wave MI” to “STEMI / non-STEMI”. Eventually STEMI became synonymous with acute coronary occlusion (ACO) requiring reperfusion, except this connection was never studied in trials. Unfortunately, the STEMI criteria have limited diagnostic criteria for ACO, leading to false cath lab activation. And worse, missing ⅓ of ACO (NSTEMI), depriving them of emergent reperfusion therapy. This led many authors to shift from STEMI/ NSTEMI to ACO-MI/ non- ACO-MI.
Paper: Aslanger EK et al.Diagnostic Accuracy of Electrocardiogram for Acute Coronary Occlusion Resulting in Myocardial Infarction (DIFOCCULT Study). Int J Cardiol Heart Vasc 2020. PMID: 32775606
Clinical Question: Does shifting from a STEMI/NSTEMI paradigm to a new approach (ACO-MI/ non-ACO-MI) result in better identification of the patients who need acute reperfusion therapy?
What They Did:
- Data was collected between May 2017 and December 2018 at a tertiary care center for percutaneous coronary intervention in Turkey.
- Single center, retrospective case-control study in Turkey
- Adult patients who presented, to the ED, clinically like ACS syndrome were evaluated
-
According to admission ECG, based on the fourth universal definition of MI, patients were divided into 3 groups:
- STEMI
- NSTEMI
- Control (ACS excluded)
- The diagnosis of acute coronary occlusion was dependent upon angiographic occlusion and rising cardiac biomarker levels.
- A combined ACO endpoint was composed of peak troponin level, troponin rise within the first 24h and angiographic appearance
-
Because in some cases of ACO, the artery may have spontaneously opened by the time of the angiogram, the investigators needed to have surrogate endpoints:
- Culprit lesion
- Acute occlusion on the angiogram AND a sufficiently elevated peak troponin, (i.e., peak troponin I > 1.0 ng/mL with a 20% change within first 24 hours)
- Peak troponin T > 5.0 ng/mL, (which has been shown to be highly correlated with ACO)
- Cardiac arrest in a clinical scenario compatible with ACO before blood could be withdrawn for troponin essay.
- The sensitivity, specificity and diagnostic accuracy of all predefined ECG criteria were sought
Outcomes:
Primary:
-
ACO was defined using the following criteria:
- Total occlusion or presence of culprit lesion on angiography with peak troponins I level equal to or greater than 1.0ng/ml + an at least 20% rise within 24 hours
- A highly elevated peak troponin (greater than 5.0 ng/ml)
- Cardiac arrest before any troponin rise has been documented with supporting clinical evidence of possible ACO
- The sensitivity and specificity of different ECG findings for ACO (up to 48 hours)
- All cause in-hospital mortality (checked from hospital records)
- All cause long term mortality (from electronic national database)
Secondary:
- Time from ECG to coronary angioplasty or CABG
- The sensitivity and specificity of current criteria in diagnosing ACO
- The sensitivity and specificity of ECG without ST-segment elevation to diagnose ACO (accuracy of ECG interpretation of acute coronary occlusion without STEMI criteria)
- The specificity of ECG with STEMI criteria (correct ECG interpretation of false positive STEMI criteria)
- The sensitivity of ECG with STEMI criteria (correct ECG interpretation of false negative STEMI criteria)
- The outcome according to ECG subclassifications (outcomes of the patients who are labeled as STEMI and the patients who are labeled as having NSTEMI but have acute coronary occlusion)
Inclusion:
- Adult patients who presented to a tertiary care center’s emergency department with clinical picture suggestive of acute coronary syndrome and were diagnosed to have an MI with or without subsequent coronary intervention
Exclusion:
- Patients without admission ECG
- Patients younger than 18 years of age.
Results:
-
Patients Eligible for Evaluation:
- 1152 STEMI
- 2353 NSTEMI
- 15,510 patients with clinical picture suggestive of acute coronary syndrome ruled-out by serial troponin
- 1000 patients of each presentation group were included in the final analysis
- Control group was younger in age, had less comorbid disease, and lower GRACE risk score compared to the STEMI/NSTEMI groups
-
ACO Detection in NSTEMI Group:
-
28.2% of patient re-classified as having ACO
- 215 (76.2%) had minor STE with reciprocal ST-depression
- 35 (12.4%) had hyperacute T-waves or de Winter’s patterns
- 18 (6.3%) had subtle anterior STE
- 14 (4.9) had non consecutive STE
-
28.2% of patient re-classified as having ACO
-
Reclassified NSTEMI to ACO was more similar to STEMI group vs non-reclassified NSTEMI group:
-
Frequency of ACO:
- Reclassified NSTEMI: 60.9%
- STEMI: 85.3%
- Non-reclassified NSTEMI: 25.3%
-
Measured Myocardial Damage by 24 to 48-hour Troponin I:
- Reclassified NSTEMI: 5.703ng/mL
- STEMI: 32.990ng/mL
- Non-reclassified NSTEMI: 0.622ng/mL
-
In-Hospital Mortality:
- Reclassified NSTEMI: 5.0%
- STEMI: 8.3%
- Non-reclassified NSTEMI: 1.8%
-
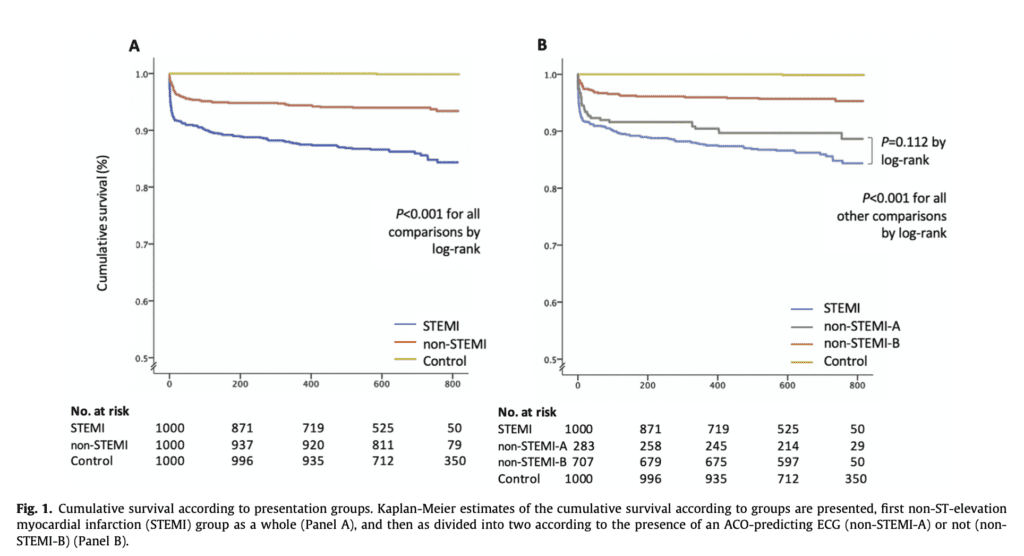
Long-Term Mortality:
- Reclassified NSTEMI: 10.6%
- STEMI: 13.7%
- Non-reclassified NSTEMI: 4.4%
-
Frequency of ACO:
-
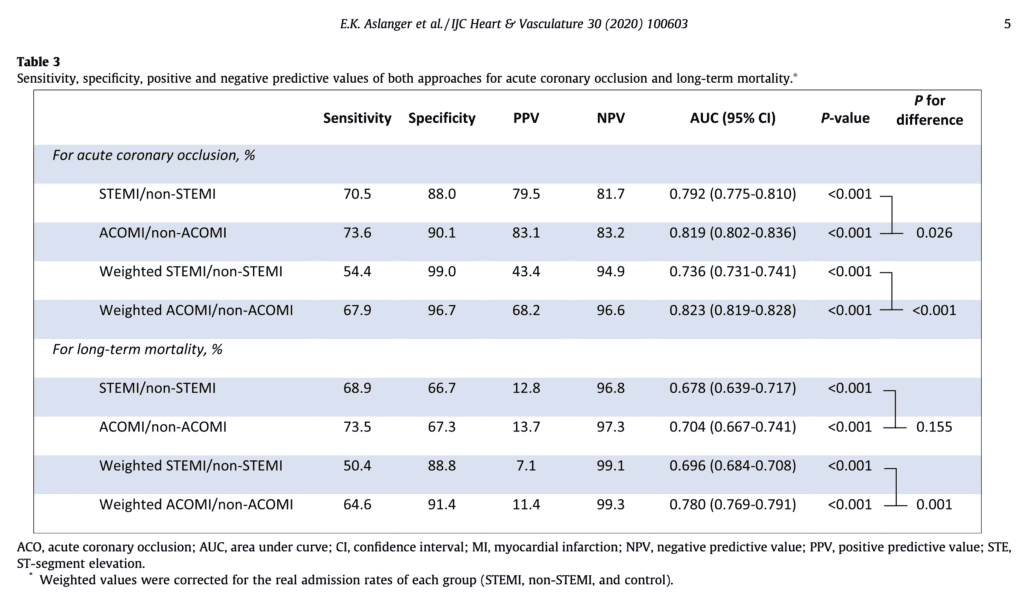
STEMI/NSTEMI vs OMI/NOMI Approach to ECG and Long-Term Mortality:
- The diagnostic accuracy of OMI/NOMI approach was superior to STEMI/NSTEMI approach
-
Effect of Intervention Timing According to ECG (ECG to PCI <120min vs ECG to PCI ≥120min)
- ECG clearly diagnostic of MI due to ACO: Early intervention associated with significantly lower long-term mortality compared to late intervention (HR 0.47; 95% CI 0.23 to 0.97; p = 0.042)
- ECG clearly diagnostic of MI due to STE and reciprocal depression, hyperacute T-waves, DeWinter’s pattern, etc: Early intervention not-associated with significantly lower long-term mortality compared to late intervention (HR 0.85; 95% CI 0.26 to 2.75; p = 0.796)
- Combining the above two types of MI compared to other types of MI: Early intervention associated with significantly higher long-term mortality compared to late intervention (HR 2.81; 95% CI 1.10 to 7.12; p = 0.030
-
Coronary Revascularization (PCI or CABG):
- ECG clearly diagnostic of MI due to ACO: Reduced mortality: 47.1% to 12.0% (HR 0.21; 95% CI 0.12 to 0.35; p < 0.001)
- ECG clearly diagnostic of MI due to STE and reciprocal depression, hyperacute T-waves, De-Winter’s pattern, etc: Non-statistically significant trend toward improved mortality: 14.7% vs 7.7% (HR 1.07; 95% CI 0.40 to 2.84; p = 0.887)
Strengths:
- Consecutive patients with an initial diagnosis of MI (i.e. not a convenience sample)
- All patients received guideline-recommended contemporary medical treatment
- Good intraobserver and interobserver agreement. They accounted for inter observer variability by having one of the ECG reviewers review the ECGs twice 3 months apart
- Large study (3000 patients were included, 1000 in each arm)
- Clear criteria of ECG findings to classify the ECGs
- ECGs were randomly sorted and reviewed by two cardiologists who were blinded to the angiogram and clinical outcomes. If there was a disagreement a third cardiologist resolved it
- Coronary angiograms were reviewed for ACO by independent investigators who were blinded to the ECG parameters and any disagreement was resolved by a third cardiologist’s opinion
Limitations:
- Retrospective study and susceptible to bias. Intra- and inter-observer agreement on ECG can change according to the experience of ECG interpreters. Although they accounted for that inthe study, extrapolating this to the real clinical world will lead to variation in diagnosis.
- This new paradigm still misses 17.9% of ACO in the non-STEMI group
- The calculated PPV and NPV may change depending on the STEMI/ non-STEMI control ratio since it is variable amongst hospitals
- Although all patents were intended to take guideline-recommended contemporary treatment, this was not controlled. Timing, duration, and percentage of used drugs could have influenced outcomes
- Intervention timing was not a randomized process, and the decision to undergo catheterization early or late might be influenced by multiple factors
- Admission Troponin measured were the first troponins obtained in the emergency department or in the cath lab whether it’s before during or after cardiac catheterization. However cardiac catheterization procedure in itself might elevate troponin levels making their initial GRACE score not completely accurate
Discussion:
- Various ECG patterns (including but not limited to STE) were tested to diagnose ACO
-
Using the ACOMI/ non- ACOMI approach
- Consistently recognizes a high risk subgroup in the non-STEMI population that have a higher frequency of ACO, larger infarct size and higher mortality
- Has significantly superior diagnostic accuracy in the prediction of ACO and long term mortality compared to the STEMI/ NSTEMI approach
-
The reasons for less pronounced ECG changes in Type 1b might be explained by
- A more limited infarct size (as indicated by lower troponin peaks and higher LVEF in this group)
- Involvement of an electrocardiographically silent area (circumflex artery)
-
Early intervention (ECG to PCI <120min) in patients with obvious MI due to ACO showed lower long-term mortality compared to late intervention, but was unchanged in patients with obvious MI due to STE with reciprocal depression, hyperacute T-waves, DeWinter’s pattern, etc.
- Interpret this with caution because some patients with subtle ECG changes may have had large MIs and others more limited area-at risk which could negate the benefits of early intervention. Additionally, this was a post hoc analysis and the study was not adequately powered to detect a modest benefit from early intervention over late intervention
- Non-ACO predicting ECG types showed significant harm with early intervention. This may be a reflection of limited area at risk and less benefit from emergent revascularization
- Universally recommended STEMI criteria come from studies designed to discriminate biomarker-positive-MI from benign-variant- STE, however neither of them had PCI intervention utilized.
-
This study validates the old STEMI concept with STE as surrogate for the physiologic ACO. However, STEMI implies that only the ST segment matters when it comes to reperfusion with no consideration for other ECG variables such as:
- Preceding QRS complex
- T wave
- ST segment morphology
- ACOMI/ non-ACOMI classification does not only depend on the ECG and therefore encompasses a broader category of patients that might need intervention.
Author Conclusion: “We believe that it is time for a new paradigm shift from the STEMI/non-STEMI to the ACOMI/non-ACOMI in the acute management of MI.”
Clinical Take Home Points:
- The title of this study was appropriate (The DIFOCCULT Trial) as the there were lots of stats that were difficult to read through
- We agree with the author’s conclusion that a new paradigm shift should be used when considering taking patients with ischemic myocardium to the cath lab, or when considering reperfusion therapy
- The current STEMI / non-STEMI approach is highly insensitive and has a weak evidence base. It implies that only certain ECG criteria (ST elevations) should be intervened on immediately, missing ⅓ of ACOs that would benefit from such therapy.
- The ACOMI/ non-ACOMI approach was found to improve long term mortality and has higher sensitivity, PPV and NPV when compared to the standard STEMI/ non-STEMI approach
- Various ECG findings (not just STE) showed correlation with ACO and should be used clinically to change the course of management for our patients from observation and troponin trending to the deserved intervention and emergent reperfusion
References:
- Aslanger EK et al.Diagnostic Accuracy of Electrocardiogram for Acute Coronary Occlusion Resulting in Myocardial Infarction (DIFOCCULT Study). Int J Cardiol Heart Vasc 2020. PMID: 32775606
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post The DIFOCCULT Trial: Time to Change from STEMI/NSTEMI to OMI/NOMI? appeared first on REBEL EM - Emergency Medicine Blog.
