Thu, Dec 12, 2013 By Felipe Serrano, MD , Lawrence B. Stack, MD, FACEP , R. Jason Thurman, MD , Lara Phillips, MD , Wesley H. Self, MD, MPH
Figure 3: Attempts to remove intraocular foreign bodies should not be made in the prehospital setting. Photo courtesy Lawrence B. Stack
There are over 2.4 million ocular injuries in the United States every year, with about 1 million of these patients presenting to EDs.1,2 The estimated incidence of eye injuries requiring medical attention is approximately 3.2 to 9.7 per 1,000 population in the U.S.2–4 Traumatic eye injuries are the most common cause of monocular blindness in the U.S., with more than 40,000 new cases every year.1,4 Therefore, these injuries have an important socioeconomic impact both in healthcare costs and lost productivity in the workplace—eye injuries account for more than 140,000 disabling work injuries every year, with the direct and indirect cost estimated at over $4 billion.5
Eye injuries are often accompanied by other traumatic injuries and can be easily overlooked, especially in the prehospital setting where rapid stabilization and transport take priority. An estimated 2% of patients with major trauma have associated eye injuries, including 65% of patients with facial fractures.6,7 With the high morbidity associated with eye injuries, it’s critically important for prehospital providers to recognize them swiftly and initiate appropriate management.
In the prehospital setting, the most important management principle is to protect the eye from further trauma during transport.
In this article, we describe the diagnosis and initial management of six common eye injuries recognizable in the prehospital setting and associated with significant morbidity when not managed appropriately.
As is typical with open globe injuries, the teardrop points toward the corneal injury.
Figure 1a: As is typical with open globe injuries, the teardrop points toward the corneal injury. Photos courtesy Lawrence B. Stack and R. Jason Thurman
Case 1: Open Globe Injuries
You are called to a construction site by the foreman of the crew stating that one of his team members was hammering a nail and then immediately felt pain in his right eye. The man states he has blurry vision in his right eye. You look at the man’s eye and see the findings shown in Figure 1a.
Question: Why does the pupil look irregular and what should you do during transport to the hospital?
Answer: The pupil has an irregular, teardrop shape because a piece of nail penetrated the patient’s cornea and the iris prolapsed through this corneal defect. In this case, the foreign body can be seen at the 8-o’clock position. The iris is drawn to the corneal defect, causing the iris to stretch and the pupil to appear like a teardrop. As is typical with these injuries, the teardrop points toward the corneal injury. A teardrop pupil is a sign of an open globe injury and the eye should be shielded without any pressure on the eye itself to prevent further injury during transport.
Discussion: This patient has an open globe injury, defined as a traumatic violation of the external layer of the eye (sclera and/or cornea). An open globe can be caused by either blunt trauma, in which blunt force causes extreme intraocular pressure to rupture the sclera/cornea (ruptured globe), or penetrating trauma, in which a foreign object enters the eye and creates a hole in the cornea/sclera (“globe laceration”).
A patient shows a prolapse of the iris through an open globe defect in the cornea
Figure 1b: Here, a patient shows a prolapse of the iris through an open globe defect in the cornea at the 10-o'clock position. This represents "extrusion of globe contents," and signifies an open globe injury. Photo courtesy Ted Brenkert
Common history and physical exam signs of an open globe include severe eye pain, decreased vision, hyphema (blood in the anterior chamber), a “peaked” or
teardrop-shaped pupil, and extrusion of globe contents.8 (See Figure 1b.) However, many patients don’t display these classic findings and it’s critical to remain highly suspicious of an open globe injury whenever a patient has the possibility of a penetrating eye injury or has sustained major blunt force to the face.
The goal of management for open globe injuries in the prehospital setting is to avoid secondary injury by preventing any increase in intraocular pressure (IOP). It’s crucial to avoid applying any external pressure to the eye. A protective shield should be placed over the eye for transport, being especially careful not to place any pressure points of the shield onto the eye itself, but instead onto the bones surrounding the eye. If a commercial metal or plastic eye shield is not available, a Styrofoam or plastic cup can be taped over the eye for protection. The head of the bed should be elevated to 30° if possible to prevent increased IOP. Because pain, agitation, uncontrolled hypertension and Valsalva maneuvers can elevate IOP, appropriate analgesic, antiemetic and sedative therapy should be provided. Narcotics are preferred to non-steroidal anti-inflammatory drugs (NSAIDs) due to the latter’s platelet-inhibiting properties. Treatment in the hospital typically includes continued protection of the globe to prevent worsening injury, intravenous antibiotics to prevent post-traumatic endophthalmitis, tetanus prophylaxis and emergent ophthalmology consultation for surgical repair of the injury.
A chemical burn can cause irreversible damage to the eye in minutes.
Figure 2a: A chemical burn can cause irreversible damage to the eye in minutes. Photo courtesy R. Jason Thurman
Case 2: Chemical Burns
You’re called to a construction site where a plumber has splashed a chemical in his eye. He’d been using this chemical to clean some of his plumbing pipes, and is now complaining of severe pain and loss of vision in his left eye, which looks like Figure 2a.
Question: After ensuring scene safety, what are your management priorities for this eye injury?
Answer: Initiate thorough irrigation of the affected eye.
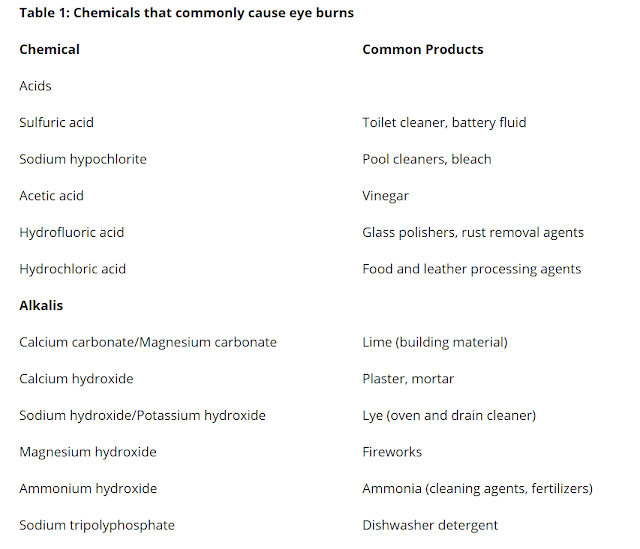
Table 1: Chemicals that commonly cause eye burns
Discussion: This patient has an alkali chemical burn of the cornea from exposure to a pipe-cleaning agent. Both acids and alkalis can cause severe chemical burns to the eye. Table 1 contains a list of chemicals that commonly cause these burns. Alkali substances lead to very rapid and deep eye injury by a process called liquefactive necrosis, in which cells are completely digested by the chemical and turn into liquid. Irreversible damage to the eye can occur within a few minutes of alkali exposure. Acid burns tend to be less severe, but still can result in significant eye damage, especially if the chemical is not rapidly removed. Hydrofluoric acid—commonly found in etchant, rust-removing compounds and wheel-cleaning agents—is an exception to this rule, behaving like an alkali with rapid penetration and damage to the eye.9
Severe chemical eye burns can cause a large corneal defect.
Figure 2b: Severe chemical eye burns can cause a large corneal defect. Photo courtesy Lawrence B. Stack
Most patients with chemical eye burns complain of severe pain, decreased vision, blepharospasm (inability to open the eyelids) and watery eyes.9 However, exposure to some alkali substances may not be painful at first due to the local inhibition of sensation. In severe cases of alkali injury, the eye may appear white due to conjuctival ischemia or a large cornea defect may be visible. (See Figure 2b.)
The essential aspect of managing chemical eye burns is immediate and copious irrigation of the eye to dilute and remove as much of the chemical as possible. Irrigation should begin in the prehospital setting. Delays in initiating irrigation by as little as 20 seconds have been associated with more severe injury in animal models of alkali eye burns.10
When positioning nasal cannula tubing for eye irrigation, the cannula prongs should be placed at the medial aspect of the affected eye.
Figure 2c: When positioning nasal cannula tubing for eye irrigation, the cannula prongs should be placed at the medial aspect of the affected eye. Then, irrigation solution can be injected through the tubing to wash out the eye. Photo courtesy Lawrence B. Stack
The eye should be quickly examined and particulate matter removed with a moist cotton swab. If possible, the patient should be placed on his/her side with the affected eye down, and irrigation should be directed from the nasal corner outward to wash away chemicals from the lacrimal punctum.11 Fluids can be injected through nasal cannula tubing into the eye for effective irrigation. (See Figure 2c.) The patient should be asked to look in all directions during irrigation to ensure complete removal of chemicals from the entire surface of the eye. Normal saline, lactated Ringer’s and water are all appropriate solutions for irrigation.10
Adequate pain control is also important, and may require parenteral doses of opioids. If possible, prehospital personnel should identify the chemical that caused the burn and relay this information to hospital providers. If safety permits, it’s useful to bring the container of the offending agent to the hospital for definitive identification of the chemical exposure. All patients with chemical eye burns should be transported to the ED. ED providers will measure the pH of tears coming from the burned eye and continue irrigation until the pH has returned to a normal range (7.5 to 8.0), indicating all of the chemical has been removed.
Case 3: Retained Foreign Body
You respond to a call from a fishing dock and find a 14-year-old boy with a fishing hook lodged in his eye. (See Figure 3, at top.) He’s extremely anxious and persistently reaching up to his eye attempting to remove the hook. He’s in severe pain and is actively vomiting.
Question: Should you remove the hook from this patient’s eye in the prehospital setting?
Answer: No.
Discussion: This patient has sustained an open globe penetrating injury with a retained intraocular foreign body. No attempts to remove intraocular foreign bodies should be made in the prehospital setting. The distal end of an intraocular foreign body may be lodged deep within the eye, in a paranasal sinus or even in the intracranial space.12 Manipulation of the object can increase the severity of injury by further damaging surrounding structures and inducing agitation and vomiting.
In the hospital setting, radiographic imaging, such as computed tomography, is often used to identify the precise location of the foreign body. The objects are usually removed by ophthalmologists in an operating room, where damage to surrounding structures can be minimized. As detailed above in Case 1, important aspects of prehospital management for these open globe injuries include eye protection with a shield, minimizing IOP by placing the head of the bed at 30°, and administering medications to minimize pain and vomiting.
Prognosis of penetrating eye injuries is very poor, with over one-third of patients requiring enucleation or having no light perception. Only about one-third of patients have visual acuity of greater than 20/200 at hospital discharge.13
More than 80% of patients with traumatic hyphemas have concomitant injuries.
Figure 4a: More than 80% of patients with traumatic hyphemas have concomitant injuries, such as facial fractures and open globe injuries. Photo courtesy Lawrence B. Stack
Case 4: Hyphema
A 16-year-old girl was struck in the left eye with a tennis ball two days ago. (See Figure 4a.) She states she initially had red-tinged blurry vision in the left eye, which has now improved. Bright lights hurt her eye. She frequently takes ibuprofen for knee pain.
Question: What is the sliver of red discoloration inferior to this patient’s pupil?
Answer: This patient has a traumatic hyphema. This red sliver is blood that has pooled in the anterior chamber, which is the space between the cornea and iris.
Discussion: Hyphema is the term used to describe bleeding into the anterior chamber of the eye. Most hyphemas are the result of trauma to the eye, but hyphemas can also occur spontaneously, especially in patients with sickle cell disease and other blood disorders.
Traumatic hyphemas are caused by tearing of the blood vessels in the iris and other structures in the anterior part of the eye due to transiently increased IOP.14 Patients with a hyphema typically complain of blurred, red-stained vision due to blood floating in the anterior chamber over the pupil.15 Patients frequently also experience photophobia, especially with direct illumination as the pupil constricts and stretches the injured iris.
This patient presents with a 100%, "8-ball" hyphema.
Figure 4b: This patient presents with a 100%, "8-ball" hyphema. Photo courtesy Lawrence B. Stack
Many hyphemas, such as the one pictured in Figure 4a, are visible with simple inspection of the eye while the patient is sitting up. However, trauma patients are regularly placed supine for spinal precaution during transport. In this position, a hyphema is difficult to diagnose as the blood layers over the iris. When safe to do so, the head of the bed should be raised to 30°. In this position, the blood layers at the bottom of the anterior chamber, which facilitates the diagnosis and improves the patient’s vision because blood moves out of the direct visual line with the pupil.14 Hyphemas are graded by the percentage of the anterior chamber filled with blood. The hyphema pictured in Figure 4a is an approximate 20% hyphema. A hyphema that completely fills the anterior chamber, such as that in Figure 4b, is sometimes referred to as an “8-ball hyphema.”
Although relatively minor direct blunt eye trauma can cause a hyphema, most are caused by major blunt force and over 80% of patients with traumatic hyphemas have concomitant injuries, such as facial fractures and open globe injuries. Therefore, prehospital providers should perform open globe precautions as outlined in Cases 1 and 3 when they see a patient with a traumatic hyphema.15
Long-term management principally involves preventing re-bleeding by avoiding NSAIDs and other antiplatelet agents and minimizing repeated constriction and dilation of the iris either with cycloplegic medications or by having the patient stay in a dark room.15 Overall, the prognosis is good, with smaller hyphemas associated with better prognosis. Only about 5% of patients require operative management for blood evacuation. Approximately 75% of patients achieve visual acuity of 20/50 or better.14
Prehospital management of retrobulbar hematomas includes rapid transport and minimizing IOP.
Figures 5a and 5b: Prehospital management of retrobulbar hematomas includes rapid transport and minimizing IOP. Photo courtesy Lawrence B. Stack
Case 5: Retrobulbar Hematoma
You respond to a high-speed motor vehicle crash and discover a 59-year-old man on the side of the road after hitting his left eye on the steering wheel. During transport he develops progressive swelling and proptosis of his left eye and his pupil becomes nonreactive to light. (See Figures 5a and 5b.)
Question: Why is this patient’s eye bulging anteriorly?
Answer: He has developed a retrobulbar hematoma, which is a bleeding posterior to the eye causing the eye to push forward.
Discussion: Retrobulbar hematoma occurs when veins draining the posterior of the eye are injured and bleed into the space between the eye and skull. Blunt trauma to the face is the typical mechanism of injury, but retrobulbar hematoma can also occur as a complication of orbital or sinus surgery. Displaced orbital wall fractures can protect against retrobulbar hematoma, because bleeding inside the orbit can drain through the fracture. Rarely, reduction of these fractures can lead to a retrobulbar hematoma if bleeding into the orbit isn’t controlled prior to reduction.16
Symptoms of a retrobulbar hematoma typically develop over a few hours as the expanding hemorrhage exerts increasing pressure on the eye, resulting in elevated IOP.17 This elevation in pressure results in ischemia to the retina and optic nerve by decreasing blood flow through the central retinal artery.17 Animal models have shown permanent eye damage within 90–120 minutes of sustaining a retrobulbar hematoma.17 Signs and symptoms include decreased visual acuity, painful proptosis (anterior displacement of the eye), a dilated pupil and restricted extraocular movements.
Principles of prehospital management include rapid transport and minimizing IOP. Vomiting and Valsalva maneuvers can lead to increased IOP, so prevention with antiemetics and pain control is especially important with retrobulbar hematomas. It’s prudent to avoid medications that can increase the risk of further bleeding, including NSAIDs and other antiplatelet agents.
Definitive treatment in the hospital involves surgical drainage of the hematoma. This procedure is typically performed by an ophthalmologist in an operating room. If an ophthalmologist is not immediately available, experienced emergency physicians or surgeons may perform an emergency lateral canthotomy and cantholysis in the ED in attempt to relieve the elevated IOP and prevent permanent blindness.17 In this procedure, the tendon positioned immediately laterally to the globe is incised, allowing blood to flow anteriorly and laterally out of the retro-orbital space.
Anisocoria occurs when one eye has a defect that prevents either normal pupillary constriction or normal pupillary dilation.
Figure 6: Anisocoria occurs when one eye has a defect that prevents either normal pupillary constriction or normal pupillary dilation. Photo courtesy Lawrence B. Stack
Case 6: Anisocoria & Mydriasis
You’re called to the scene of a domestic dispute and find a 33-year-old woman sitting on the curb next to a police car. Police called for an EMS response when they noticed her pupils were not equal. (See Figure 6.) She reports no trauma today but does say she was struck with a fist in the right eye two days ago. She complains of mild pain to the right eye and photophobia. Her left eye constricts normally to light, but the right eye doesn’t constrict at all. Her mental status is normal. Other than these pupillary findings, her neurologic exam is normal, including extraocular movements.
Question: Should you begin treatment to decrease intracranial pressure, such as intravenous mannitol?
Answer: No. Although increased intracranial pressure caused by a space-occupying lesion—such as intracranial bleeding—can cause a unilateral dilated and non-reactive (“blown”) pupil, many other conditions can also cause this pupillary abnormality. Because the patient is well-appearing and her neurologic exam is otherwise normal, a severe intracranial injury is less likely and a potentially harmful medication, such as mannitol, should not be administered. This patient has traumatic mydriasis, not an intracranial hemorrhage.
Discussion: This patient has anisocoria, defined as pupils of unequal size. Anisocoria occurs when one eye has a defect that prevents normal pupillary constriction (the affected pupil is dilated, called mydriasis), or prevents normal pupillary dilation (the affected pupil is constricted, called miosis). In this case the right pupil doesn’t constrict to light, indicating abnormal mydriasis of the right eye. Mydriasis is caused by either injury to the sphincter muscle in the iris or the parasympathetic nerves innervating the iris.18 Three important causes of mydriasis include an intracranial space-occupying lesion compressing cranial nerve III, pharmacologic mydriasis and traumatic mydriasis.
Space-occupying lesion: With severe increases in intracranial pressure due to intracranial bleeding or swelling, which can occur with traumatic brain injury, the brain is pushed inferiorly. With extremely high intracranial pressure, the uncus of the temporal lobe herniates through the tentorium, which is the dura mater separating the cerebrum from the brainstem. Uncal herniation causes compression and dysfunction of cranial nerve III, leading to loss of parasympathetic innervation and mydriasis to the eye on the same side as the herniation. Uncal herniation is associated with many other neurologic abnormalities, including hemiparesis to the limbs on the opposite side of the herniation, impaired extraocular movements, and altered mental status eventually leading to coma. In an unconscious trauma patient with anisocoria, uncal hernia should be assumed until proven otherwise with brain imaging at the hospital.
Pharmacologic mydriasis: Anticholingeric medications that block the parasympathetic nervous system can cause pharmacologic mydriasis when they contact one eye. The anticholinergic nebulizer medication ipratropium, which is used to treat asthma and chronic obstructive pulmonary disease, commonly causes mydriasis when an ill-fitting nebulizer mask results in the medication spraying into one eye.19
Traumatic mydriasis: Direct blunt trauma to the sphincter muscle of the iris can cause traumatic mydriasis. Symptoms include eye pain, blurry vision and photophobia. Contusion of the muscle results in a transient mydriasis, while tears to the muscle fibers can cause permanent injury. The mainstay of prehospital management involves protection of the eye from further injury during transport. ED evaluation involves ruling out other causes of mydriasis and facilitating ophthalmologic evaluation. Surgical repair is a potential option for patients with severe and persistent symptoms.20
Conclusion
Traumatic eye injuries are commonly encountered in the prehospital setting and associated with significant morbidity. The primary role of prehospital providers is to recognize that an eye injury is present and protect the eye from further harm. During transport, it’s prudent to assume all penetrating and blunt eye injuries have an open globe and to protect the eye with a firm shield. When treating patients with chemical eye burns, prehospital providers have an opportunity to greatly reduce the severity of the injury by initiating rapid, copious and continuous irrigation of the eye.
In patients with multisystem trauma, ensuring airway-breathing-circulation and rapid transport are priorities, but alerting hospital providers to possible eye injuries helps them continue appropriate shielding to protect the eye from further damage and to initiate definitive treatment. Through expert recognition and initiation of prehospital treatment, EMS providers can maximize a patient’s recovery from an eye injury.
References
1. National Society to Prevent Blindness. Vision problems in the U.S.: A statistical analysis. National Society to Prevent Blindness; New York, 1980.
2. McGwin G Jr, Owsley C. The incidence of emergency department-treated eye injury in the United States. Arch Ophthalmol. 2005;123(5):662–666.
3. May DR, Kuhn FP, Morris RE, et al. The epidemiology of serious eye injuries from the United States Eye Injury Registry. Graefes Arch Clin Exp Ophthalmol. 2000;238(2):153–157.
4. McGwin G, Xie A, Owsley C. The rate of eye injury in the United States. Arch Ophthalmol. 2005;123(9):970–976.
5. National Safety Council. (2013.) Injury facts 2013 edition. MHI. Retrieved Oct. 1, 2013, from www.mhi.org/downloads/industrygroups/ease/technicalpapers/2013-National-Safety-Council-Injury-Facts.pdf.
6. Poon A, McCluskey PJ, Hill DA. Eye injuries in patients with major trauma. J Traum.1999;46(3):494–499.
7. Holt GR, Holt JE. Incidence of eye injuries in facial fractures: An analysis of 727 cases. Otolaryngol Head Neck Surg. 1983;91(3):276–279.
8. Pokhrel PK, Loftus SA. Ocular emergencies. Am Fam Physician. 2007;76(6):829–836.
9. Fish R, Davidson RS. Management of ocular thermal and chemical injuries, including amniotic membrane therapy. Curr Opin Ophthalmol. 2010;21(4):317–321.
10. Spector J, Fernandez WG. Chemical, thermal, and biological ocular exposures. Emerg Med Clin North Am. 2008;26(1):125–136.
11. Duffy B. Managing chemical eye injuries. Emerg Nurse. 2008;16(1):25–29.
12. Morley MG, Nguyen JK, Heier JS, et al. Blast eye injuries: A review for first responders. Disaster Med Public Health Prep. 2010;4(2):154–160.
13. Smith D, Wrenn K, Stack LB. The epidemiology and diagnosis of penetrating eye injuries. Acad Emerg Med.2002;9(3):209–213.
14. Sankar PS, Chen TC, Grosskreutz CL, et al. Traumatic hyphema. Int Ophthalmol Clin. 2002;42(3):57–68.
15. Brandt MT, Haug R. Traumatic hyphema: A comprehensive review. J Oral Maxillofac Surg. 2001;59(12):1462–1470.
16. Colletti G, Valassina D, Rabbiosi D, et al. Traumatic and iatrogenic retrobulbar hemorrhage: An 8-patient series. J Oral Maxillofac Surg. 2012;70(8):e464–e468.
17. Chen YA, Singhal D, Chen YR, et al. Management of acute traumatic retrobulbar hematomas: A 10-year retrospective review. J Plast Reconstr Aesthet Surg. 2012;65(10):1325–1330.
18. Kawasaki A: Disorders of pupillary function, accommodation, and lacrimation. In Miller NR, Walsh FB, Hoyt WF (Eds.), Walsh and Hoyt's clinical neuro-ophthalmology. Lippincott Williams & Wilkins: Philadelphia, pp. 739–805, 2005.
19. Iosson N. Images in clinical medicine: Nebulizer-associated anisocoria. N Engl J Med. 2006;354(9):e8.
20. Angmo D, Agarwal T, Khokhar S. Single pass, single suture technique for repair of traumatic mydriasis. Eur J
By
Felipe Serrano, MD
Felipe Serrano, MD, is an emergency medicine physician practicing at a major Level I trauma center. He is also associated with Vanderbilt University School of Medicine’s Department of Emergency Medicine in Nashville (Tenn.).
Lawrence B. Stack, MD, FACEP
Lawrence B. Stack, MD, is an emergency physician with 23 years of experience in treating patients at Level I trauma centers, and author of The Atlas of Emergency Medicine, The Atlas of Emergency Radiology, and The Handbook of Medical Photography. He is also associated with Vanderbilt University School of Medicine’s Department of Emergency Medicine in Nashville (Tenn.).
R. Jason Thurman, MD, is an emergency physician with 15 years of experience at Level I trauma centers, and author of The Atlas of Emergency Medicine and The Atlas of Emergency Radiology. He is also associated with Vanderbilt University School of Medicine’s Department of Emergency Medicine in Nashville (Tenn.).
Lara Phillips, MD, is an emergency physician at a Level I trauma center and former emergency medicine technician. All authors are associated with Vanderbilt University School of Medicine’s Department of Emergency Medicine in Nashville (Tenn.).
Wesley H. Self, MD, MPH, is an emergency physician with 10 years of experience in treating patients at Level I trauma centers and a physician-scientist specializing in rapid management of critically ill and injured patients. He is also associated with Vanderbilt University School of Medicine’s Department of Emergency Medicine in Nashville (Tenn.).
Tactical Field Care: Penetrating Eye Trauma
by JTS / CoTCCC
Eye injuries can lead to significant vision loss and blindness if the damage is not mitigated on the battlefield. Eye injuries should be evaluated after active combat has ceased and other life-threatening injuries have been addressed. If a penetrating eye injury is noted or suspected, perform a rapid field test to evaluate visual acuity, document your findings and treat appropriately. This video provides more in-depth information on the following topics:
- Simplified visual acuity testing to be performed on the battlefield
- Indications for immediate evacuation based on presenting symptoms after eye injury
- Corneal laceration and other penetrating eye injuries
- Infection prevention and the role of antibiotics in penetrating eye trauma
- Rigid eye shields and field treatment options
Joint Trauma System (JTS) / Committee on Tactical Combat Casualty Care (CoTCCC). The CoTCCC is the branch of the JTS focused on the standard of care for prehospital battlefield medicine. The JTS is the Department of Defense Center of Excellence for Trauma providing clinical practice guidelines and performance improvement for all levels of military trauma care.
This work is licensed under a CreativeCommons Attribution-NonCommercial-NoDerivatives 4.0 International License. For more information, please visit https://creativecommons.org/.
Dr Ramon REYES, MD,
Por favor compartir nuestras REDES SOCIALES @DrRamonReyesMD, así podremos llegar a mas personas y estos se beneficiarán de la disponibilidad de estos documentos, pdf, e-book, gratuitos y legales..
Por favor compartir nuestras REDES SOCIALES @DrRamonReyesMD, así podremos llegar a mas personas y estos se beneficiarán de la disponibilidad de estos documentos, pdf, e-book, gratuitos y legales..
Grupo Biblioteca/PDFs gratis en Facebook
https://www.facebook.com/groups/PDFgratisMedicina #DrRamonReyesMD
https://www.facebook.com/DrRamonReyesMD
https://www.instagram.com/drramonreyesmd/
https://www.pinterest.es/DrRamonReyesMD/
https://twitter.com/eeiispain
Blog
http://emssolutionsint.blogspot.com/2016/12/dr-ramon-reyes-diaz-md-emt-t-dmo.html
TELEGRAM
Group https://t.me/joinchat/GRsTvEHYjNLP8yc6gPXQ9Q