
 Background: Sports-related concussions are among the most common injuries in children and adolescents, affecting millions of youth athletes annually.1 Given their prevalence in this population, providers must be up to date on diagnosis and management. Historical practice recommends rest to prevent adverse outcomes; however, evidence suggests strict rest is harmful. Relative rest (activities of daily living and reduced screen time) is indicated for the first 12-48 hours, followed by light-intensity physical activity (walking or stationary cycling while avoiding the risk of contact, collision, or fall) as tolerated.2 The authors of this paper sought to “better understand the effects of activity after a concussion in youth.”3
Background: Sports-related concussions are among the most common injuries in children and adolescents, affecting millions of youth athletes annually.1 Given their prevalence in this population, providers must be up to date on diagnosis and management. Historical practice recommends rest to prevent adverse outcomes; however, evidence suggests strict rest is harmful. Relative rest (activities of daily living and reduced screen time) is indicated for the first 12-48 hours, followed by light-intensity physical activity (walking or stationary cycling while avoiding the risk of contact, collision, or fall) as tolerated.2 The authors of this paper sought to “better understand the effects of activity after a concussion in youth.”3
Article: Chauhan R, Cheng A, Tsow R, Sakakibara BM, Babul S, Schmidt J. Activity and Recovery Among Youth With Concussion: A Meta-analysis. Pediatrics. 2023 May 1;151(5):e2022059592. PMID: 37073681.4
Clinical Question: In children and youth under 18, how effective is early return to physical and social activity compared to usual care on recovery following concussion?
What They Did:
- The authors performed a systematic review up to October of 2022, meta-analyses were conducted where appropriate for RCTs included in the review.
- They searched the following databases: Medline Ovid, Embase Ovid, CINAHL EBSCO, and PsychINFO.
- The main search terms included concussion, exercise, social participation, child, and adolescents.
- The Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines were followed.
- Two authors independently screened each article for inclusion and completed a full-text review of articles that met eligibility criteria.
- Reviewer discrepancies were resolved through discussion and adding a third author if needed.
- Investigators contacted the original study’s authors to obtain data not reported in the article.
- The Cochrane Risk of Bias Tool was used for Randomized Control Trials.
- The Risk of Bias in Nonrandomized Studies of Intervention (ROBINS-I) assessment tool was used for non-randomized studies.
- The trial was registered with PROSPERO (#CRD42020176278).
Population:
Inclusion:
- Children and adolescents aged 0-18 years from the community who sustained at least one concussion.
- Studies with a mixed population of children and adults were included if greater than 50% of the sample size was within the age range.
Exclusion:
- Studies that used a review methodology (literature, scoping, systematic) or were “gray” literature (i.e., thesis, conference abstracts).
- Papers not published in English.
Intervention:
- Activity-based interventions following a concussion
- Physical (aerobic and anaerobic)
-
And/or social activities
- Activities that engage a person based on the role, social setting, or interests include club involvement or peer interactions.
Control:
- “Usual care intervention” or following regular care guidelines
- No comparison group (ie, pre-post studies)
- Comparisons between 2 activity-based interventions
Outcomes:
Primary Outcome:
-
Recovery after a concussion is defined by:
- Symptoms, including duration, severity, and number of symptoms
- Quality of life/QoL (mental and physical health, school functioning, and activity participation)
- Days until return to preinjury activity
Results:
- 5642 studies selected for screening
- 5519 articles excluded
- 123 full-text studies screened for eligibility
-
24 Studies were included following screening:
- 10 RCTs, 4 case series/ studies, 4 retrospective study designs, 3 quasi-experimental designs, 2 pre-post studies, and 1 feasibility study
- All studies included physical activity in their intervention protocol.
- None of the studies included interventions composed of social activities.
- 4 studies included adults but met a prespecified condition of >50% within the age range 0-18 years.
- Symptom reporting was the most common outcome in the included studies.
Primary Outcome:
-
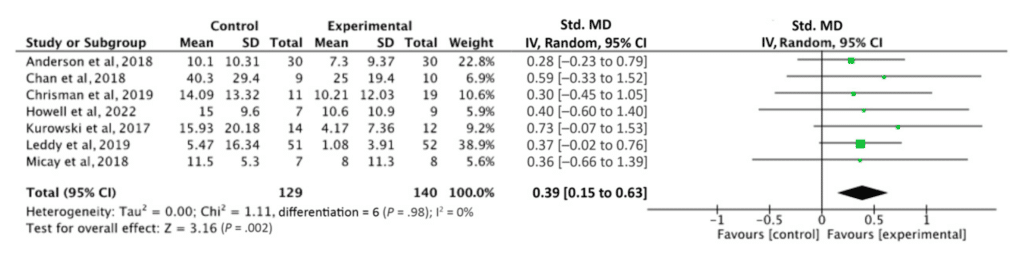
Effect of Physical Activity on Symptom Resolution:
- Seven studies informed the meta-analysis on symptom resolution.
- Activity engagement had a significant effect on symptom resolution (standardized MD, 0.39 [95% CI, 0.15 to 0.63]; I2, 0%; P 5 .002)
Forest Plot for the effectiveness of ABI on symptoms
-
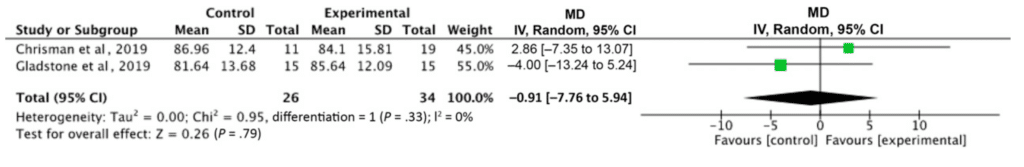
Effect of Physical Activity on Quality of Life:
- Engagement in a physical activity-related intervention did not significantly improve QoL.
- Activity-based interventions had no significant effect on QoL (mean difference, 0.91 [95% confidence interval, –7.76 to 5.94]; I2, 0%; P 5 .79).
Forest Plot of ABI on QOL Outcomes
-
Effect of Physical Activity on Days to Preinjury Activity Levels:
- No meta-analysis was performed on return to preinjury activity levels because of the insufficient number of RCTs conducted.
- 1 RCT did not demonstrate significant results (P = .82) between usual care and exercise on time until approval of return to full activity.
Strengths:
- Asks a clinically relevant question.
- Investigators performed a comprehensive search of multiple databases.
- They followed PRISMA guidelines and registered the study with PROSPERO, increasing the results’ transparency and reproducibility.
-
Researchers utilized two bias tools in an attempt to assess bias:
- The Cochrane Risk of Bias Tool was used for RCTs.
- The Risk of Bias in Nonrandomized Studies of Intervention (ROBINS-I) tool was used for non-RCTs.
- Overall, Heterogeneity was low, meaning that patients and data in the meta-analysis were similar enough to feel confident in the pooled estimate.
Limitations:
- The search excluded non-English papers and unpublished trials.
- The included studies included had small sample sizes ranging from 6 to 677 patients.
- Some included studies contained an adult population, albeit no more than 50%, which could affect generalizability.
- The investigators included both acute and chronic symptoms.
-
There was massive variability in the included studies in terms of intervention initiation (i.e. days vs years).
- It would have been better to just include studies that initiated intervention within days of concussion as this was the main question at hand.
- There was a lack of true comparison or control groups in some studies.
- The “usual care intervention” was not well-defined.
- The paper Included examples of physical and social activities but did not address return to play or sport-specific activities in intervention groups which is an important clinical question for youth athletes.
- Unable to blind participants in RCT due to the nature of the intervention.
- There were 24 studies in total, with 13 studies rated as having high or serious risk of bias, with only 1 study meeting low risk of bias.
- One aim was to evaluate social activity, but no studies included social interventions.
- Only 1 RCT measured days until return to activity. Therefore, no meta-analysis was completed.
- Of the 7 RCTs which could be pooled together for symptom resolution, 2 studies provided more than 60% of the weight.
- There was variation in intervention initiation from time of injury (days versus years), which may impact the precision of findings and validity.
Discussion:
- According to the most recent consensus statement on concussion in sport, early return to activities, including activities of daily living which does not exacerbate symptoms, should be encouraged and may facilitate recovery, although more evidence is needed. 5
- Although this systematic review and meta-analysis address an essential clinical question shrouded in uncertainty, the quality of evidence of the included papers is poor. Most included studies had small sample sizes, no true control groups, and a high or serious risk of bias.
- The studies were understandably unblinded. It would be difficult to blind these studies, as participants would know if they are performing physical activity. Likewise, the measures of outcomes were based on subjective self-assessed questionnaires. In an open-label trial, subjective assessments are particularly prone to bias. Quantitative measures should be used to limit the introduction of bias when possible.
- Graduated return-to-play protocols typically include sport-specific activities. This study did not address or include these activities nor a return to play protocol but instead focused on light aerobic activities. It is essential to outline a rehabilitation plan which includes clear, well-defined, and sport-specific steps to keep this population motivated throughout their recovery.
- Concussion symptoms are often delineated into four categories: physical, emotional, cognitive, and sleep. One of the main aims was to evaluate social activities. However, the definition of “social” activities was not well defined. Furthermore, no studies with social interventions were included. Despite their importance in this population, there is limited information on “return to learn” and other cognitive activities.
Author Conclusions: “Findings indicate that activity-based interventions may significantly improve concussion symptoms. There is insufficient data to understand the effect of activity-based intervention on QoL and return to preinjury activity levels.”
Our Conclusion:
Concussions are common and have the potential to cause long-term neurologic sequelae. Youth may experience slower recovery and prolonged side effects compared to adults.6 Given these considerations, we must have high-quality research to inform prevention, recognition, and early evaluation and management of concussions. The data from this systematic review and meta-analysis are far from high quality and informed by small, unblinded, subjective, low-quality studies with a high risk of bias. Furthermore, the results do not add new information beyond what we already know about concussion recovery—garbage in, garbage out.
References
- McKeithan L, Hibshman N, Yengo-Kahn A, Solomon GS, Zuckerman S. Sport-Related Concussion: Evaluation, Treatment, and Future Directions. Medical Sciences. 2019;7(3):44. PMID: 30884753.
- Leddy JJ , Burma JS , Toomey CM , et al . Rest and exercise early after sport-related concussion: a systematic review and meta-analysis. Br J Sports Med 2023:bjsports-2022-106676. PMID: 37316185.
- Chauhan R, Cheng A, Tsow R, Sakakibara BM, Babul S, Schmidt J. Activity and Recovery Among Youth With Concussion: A Meta-analysis. Pediatrics. 2023 May 1;151(5):e2022059592. PMID: 37073681.
- Chauhan R, Cheng A, Tsow R, Sakakibara BM, Babul S, Schmidt J. Activity and Recovery Among Youth With Concussion: A Meta-analysis. Pediatrics. 2023 May 1;151(5):e2022059592. PMID: 37073681
- Patricios JS, Schneider KJ, Dvorak J, et al. Consensus statement on concussion in sport: the 6th International Conference on Concussion in Sport–Amsterdam, October 2022. British Journal of Sports Medicine. 2023;57(11):695-711. PMID: 37316210.
- Lax ID, Paniccia M, Agnihotri S, et al. Developmental and gender influences on executive function following concussion in youth hockey players. Brain Inj. 2015;29(12):1409–1419. PMID: 26362811
Guest Post By:

Laura Schenkel, MD
Sports Medicine Fellow
Vassar Brothers Hospital, Poughkeepsie, New York
Email: laura.schenkel@nuvance.org

Alex Chasin, MD
Sports Medicine Fellowship Program Director
Vassar Brothers Hospital, Poughkeepsie, New York
Email: alexander.chasin@nuvancehealth.org

Marco Propersi, DO FAAEM
Vice-Chair of Emergency Medicine
Assistant Emergency Medicine Residency Program Director
Vassar Brothers Hospital, Poughkeepsie, New York
Twitter: @marco_propersi
Post-Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post Back in the Game: The Effects of Activity on Youth Concussion Recovery appeared first on REBEL EM - Emergency Medicine Blog.
