
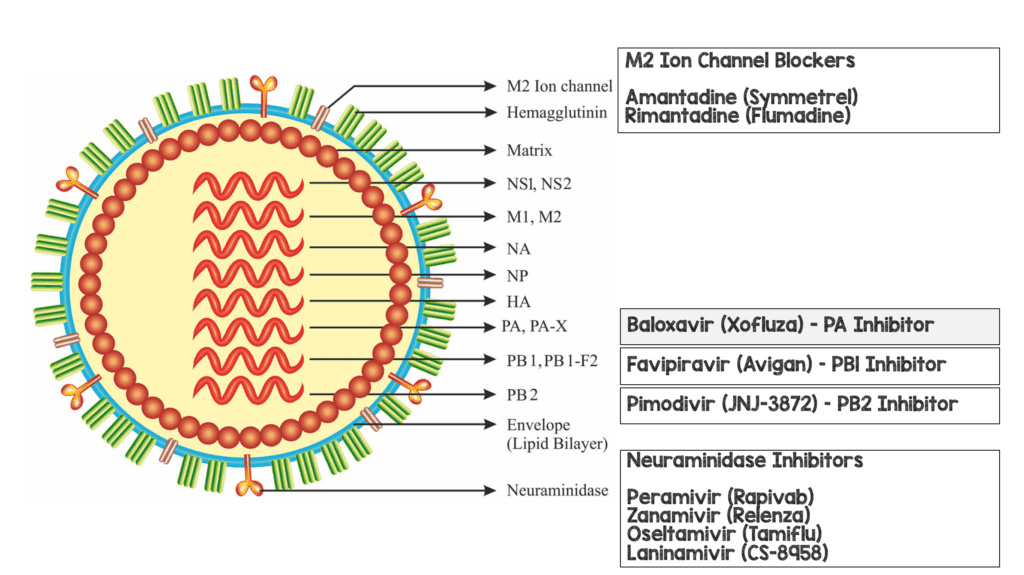
 Background: On October 24th, 2018, Roche, the maker of oseltamivir, announced that the US Food and Drug Administration (FDA) approved Xofluza (baloxavir marboxil) for the treatment of acute, uncomplicated influenza in people 12 years of age and older. Historically, there have been two classes of influenza treatment, the M2 ion-channel inhibitors, and the neuraminidase inhibitors, however circulating influenza viruses have become largely resistant to M2 ion-channel inhibitors and the emergence of newer strains of influenza (H1N1) could threaten the utility of neuraminidase inhibitors as well. I have written previously about the Tamiflu Debacle and why this is a medication we should not prescribe to immunocompetent patients. In this post, we attempt to answer a different question: Is baloxavir approval another debacle or does it actually improve patient oriented outcomes?
Background: On October 24th, 2018, Roche, the maker of oseltamivir, announced that the US Food and Drug Administration (FDA) approved Xofluza (baloxavir marboxil) for the treatment of acute, uncomplicated influenza in people 12 years of age and older. Historically, there have been two classes of influenza treatment, the M2 ion-channel inhibitors, and the neuraminidase inhibitors, however circulating influenza viruses have become largely resistant to M2 ion-channel inhibitors and the emergence of newer strains of influenza (H1N1) could threaten the utility of neuraminidase inhibitors as well. I have written previously about the Tamiflu Debacle and why this is a medication we should not prescribe to immunocompetent patients. In this post, we attempt to answer a different question: Is baloxavir approval another debacle or does it actually improve patient oriented outcomes?
How Does Baloxavir Work (Warning: This is Super Nerdy Viral Replication Stuff)?
Influenza has a polymerase complex composed of three protein subunits: polymerase basic protein 1 (PB1), polymerase basic protein 2 (PB2), and polymerase acidic protein (PA). All three components are essential for viral replication. The way influenza replicates is that the PB2 subunit binds to host cellular pre-messenger RNA and is cleaved by the endonuclease in the PA subunit. This process allows for transcription of viral messenger RNA by the RNA polymerase function of PB1. Baloxivir is a prodrug of the selective PA component and inhibits endonuclease activity.
What They Did:
- This publication was actually two, double-blind, placebo-controlled, randomized trials involving healthy outpatients with acute uncomplicated influenza.
- The first trial, was a phase 2, dose-ranging study of 10, 20, and 40mg of baloxavir vs placebo in Japanese adults, aged 20 – 64 years, with acute influenza from December 2015 – March 2016. The randomization of this trial was done in a 1:1:1:1 ratio.
- The second trial, was a phase 3 trial called CAPSTONE-1. This was a placebo-controlled, randomized trial of patients with influenza-like illness, in the United States and Japan, during the December 2016 – March 2017 influenza season. Patients aged 20 – 64 years were randomized in a 2:2:1 ratio to receive single oral dose of baloxavir (40mg for patients weighing <80kg or 80mg for patients ≥80kg), oseltamivir at a dose of 75mg BID for 5 days, or matching placebos.
- Adult patients in the three groups of the CAPSTONE-1 trial received a 5-day regimen of baloxavir and a placebo matching oseltamivir, oseltamivir and a placebo matching baloxavir, or placebo only
- Adolescent patients aged 12 – 19 years of age were randomized in a 2:1 ratio to receive either baloxavir or placebo on day 1 only (No oseltamivir)
Outcomes:
- Primary: Time to alleviation of influenza symptoms in the intention-to-treat infected population (Defined as: time from the start of the trial regimen to the time when all seven influenza-related symptoms were rated by the patients as absent or mild for at least 21.5 hours)
-
Secondary:
- Time to resolution of fever
- Time to return to usual health
- Newly occurring complications leading to antibiotic use
-
Virologic:
- Changes from baseline in infectious virus and viral RNA titers
- Duration of virus detection
- Frequency of the emergence of amino acid changes associated with reduced susceptibility to baloxavir
-
Safety:
- Frequency and severity of adverse events
Inclusion:
- Patients able to give informed written consent and comply with all study procedures
- In the phase 2 study, patients had to have a virology confirmation of influenza to get treatment; In the phase 3 study, patients did not have to have virology confirmation of influenza (i.e. flu-like illness)
- 1,044 patients with confirmed flu (≈75%)
- 356 patients negative for flu (≈25%)
- Age ≥12 years to ≤64 years
- Patients with a diagnosis of influenza confirmed by all of the following:
- Fever ≥38 degrees Celsius (axillary)
- At least one of the following general systemic symptoms
- Headache
- Feverishness or chills
- Muscle or joint pain
- Fatigue
- At least one of the following respiratory symptoms
- Cough
- Sore Throat
- Nasal Congestion
- Time interval between onset of symptoms and predose examination ≤48 hours. Onset of symptoms defined as either:
- Time of the first increase in body temperature (an increase of at least 1 degree Celsius from normal body temperature)
- Time when the patient experiences at least one general or respiratory symptom
- Women of childbearing potential who agreed to use a highly effective method of contraception for 3 months after the 1st dose of the study drug
Exclusion (And no, we are not kidding…this list is extensive):
- Severe influenza infection requiring inpatient treatment
- Patients aged ≥20 years with known allergy to oseltamivir
- Patients with any of the following risk factors:
- Women who are pregnant or within 2 weeks post-partum
- Residents of long-term care facilities
- Chronic respiratory diseases including bronchial asthma
- Neurological and neurodevelopmental disorders including disorders of the brain, spinal cord, peripheral nerve, and muscle
- Heart disease such as congenital heart disease, congestive heart failure, or coronary artery disease, excluding hypertension
- American Indians and Alaskan natives
- Blood disorders such as sickle cell disease
- Endocrine disorders including diabetes mellitus
- Kidney disorders
- Liver disorders
- Metabolic disorders
- Compromised immune system (i.e. immunosuppressant therapy, cancer on chemotherapy, human immunodeficiency virus)
- Morbid obesity (BMI ≥40)
- Patients unable to swallow tablets or capsules
- Previously received baloxavir
- <40kg weight
- Patients exposed to an investigational drug within 30 days prior to predose examinations
- Breast feeding or positive pregnancy test
- Concurrent infections requiring systemic antimicrobial and/0r antiviral therapy
- Received peramivir, Laninamivir, oseltamivir, zanamivir, rimantadine, umifenovir, or amantadine within 30 days prior
- Received an investigational monoclonal antibody for a viral disease in the last year
- Severe chronic underlying diseases
- Known creatinine clearance ≤60mL/min
- Patients unlikely to comply with required study visits and interventions
Results (This is 2 trials in 1):
Phase 2 Trial (Dose-Finding Study)
- 400 patients underwent randomization, but only 389 completed the trial
- Only 61 – 71% of patients were infected with confirmed influenza virus
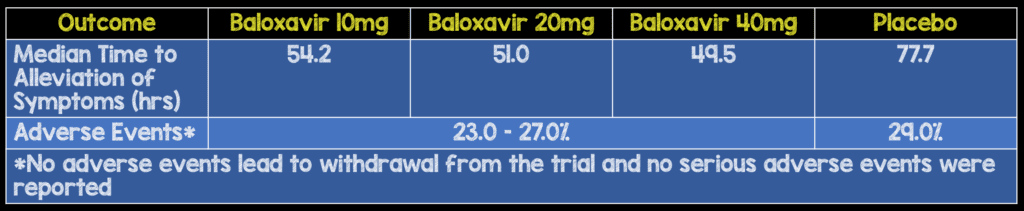
- All 3 Baloxavir groups had lower viral titers on days 2 & 3 compared to placebo group
- 4/182 (2.2%) of Baloxavir patients had post-treatment development of PA amino acid substitutions that confer increased resistance to baloxavir
Phase 3 Trial (CAPSTONE-1)
- 1436 patients underwent randomization, but only 1366 patients completed the trial and 1064 were included in the intention-to-treat infected population
- Only 52.9% of patients initiated the trial regimen within 24 hours after symptom onset
- Influenza A (H3N2) accounted for 84.8 – 88.1% of infections in all three trial groups
- 77.2% of patients were enrolled in Japan
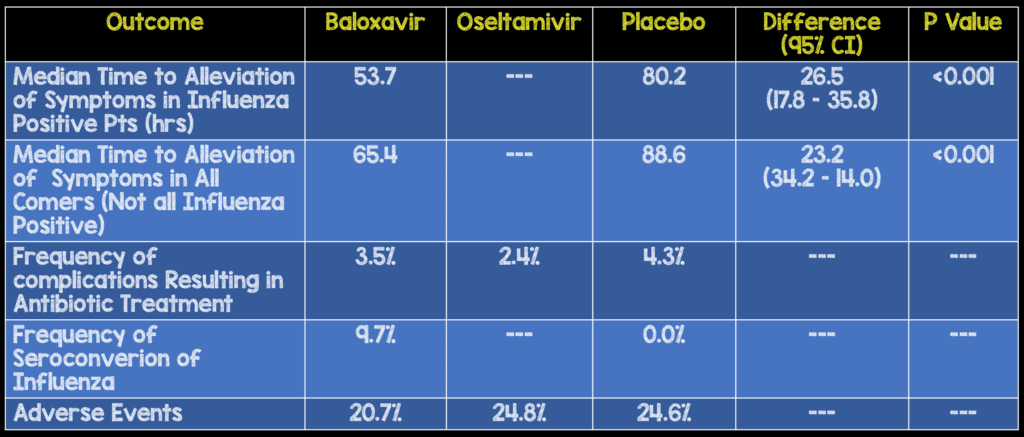
- Median Time to Alleviation of Symptoms in Adolescents was also reduced 38.6hrs (p = 0.006)
- Alleviation of symptoms greater in patients who initiated trial regimen within 24 hours after symptoms onset vs those who initiated later:
- Treatment ≤24hrs median difference, 32.8hrs; p<0.001
- Treatment >24hrs median difference, 13.2hrs; p = 0.008
- There was no difference in the time to alleviation of symptoms between baloxavir vs oseltamivir groups.
- There was also a median shorter time to resolution of fever with baloxavir vs placebo (24.5hrs vs 42.0hrs)
- Baloxavir was associated with significantly more rapid declines in infectious viral load than placebo vs oseltamivir by day 1 after initiation of medications and shorter median duration of virus detection
Strengths:
- Important question to investigate as pandemic influenza remains an important issue
- Patients of all ages received their first dose of the trial medication under direct observation to ensure the medication was taken
- Patients equally matched at baseline between groups in terms of demographic and clinical characteristics
- Investigators unaware of trial group assignments
Limitations:
- Authors’ access to the data was not restricted by confidentiality agreements
- Study design performed by the study sponsor
- Data were compiled by the sponsor and analyzed by a statistician employed by the sponsor
- A positive rapid antigen test for influenza was an entry criterion for the phase 2 trial but not for the phase 3 trial
- An extensive exclusion list, limits the generalizability of using this medication in the majority of patient populations (i.e. these were young healthy patients, with essentially, no medical problems)
- In the ClinicalTrials.gov [2] listing there is 1 primary outcome and 19 secondary outcomes, with several time points for each evaluated, however in the main manuscript we get cherry picked time points that show benefit without information on all the secondary endpoints listed or time frames evaluated (i.e. We do not have full release of data)
- Study needed 1494 patients to provide at least a 90% power to detect a 28-hour difference in the median time to alleviation of symptoms and fell short of this number. Also of the 1400 randomized, 400 were excluded creating a selection bias
- It is unclear if the increased virus seroconversion associated with baloxavir will affect susceptibility, but there was a longer median time to alleviation of symptoms in patients with seroconversion.
- It is unclear if reduced viral load is associated with a reduced risk of virus transmission
- 88% of patients had H3N2 influenza. This means the results of this trial have no applicability to other strains based on this data
- Placebo group did not have real symptom guided therapy (i.e. NSADs, APAP, decongestants)
- Unclear how randomization was done
Discussion:
- Cost of baloxavir = $150.00 US for a single dose (Company states it plans to offer a coupon that will bring price down to $30.00 US for people with commercial insurance)
- Cost of oseltamivir (Tamiflu) = $100.00 US for a five day course
- Approval of baloxavir is based on a single, relatively small, narrow population, pharmaceutical sponsored trial, with ¾ of the patients, not in the US is irresponsible at best and criminal at worst
- Authors state that there is no safety concern, however a study of this size cannot give true safety data
- Based on the phase-2 dose finding study, would it make more sense to go with the lowest possible dose which gives peple almost the same time to relief?
- Variable dosing based on weight wasn’t studied prior to the phase 3 trial
Author Conclusion: “Single-dose baloxavir was without evident safety concerns, was superior to placebo in alleviating influenza symptoms, and was superior to both oseltamivir and placebo in reducing the viral load 1 day after initiation of the trial regimen in patients with uncomplicated influenza. Evidence for the development of decreased susceptibility to baloxavir after treatment was also observed.”
Clinical Take Home Point: Consistent with every other study on anti-viral medications for influenza, baloxavir appears to decrease duration of symptoms, especially in patients treated within 24 hours of symptoms, BUT a massive exclusion list, cost of the medication, increased resistance after initiation, results only applicable to H3N2 (88% of patients with flu), no comparison to standard care (i.e. symptom based therapy), pharma sponsored study, and no patient oriented outcomes, it is hard to make an argument for the use of baloxivir in patients with confirmed influenza. This trial should be a reminder as to why an industry funded trial, without full release of data, and cherry picked endpoints should not be used to change practice.
References:
- Hayden FG et al. Baloxavir Marboxil for Uncomplicated Influenza in Adults and Adolescents. NEJM Sept 2018. PMID: 30184455
- ClinicalTrials.gov [Link is HERE]
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post Baloxavir (Xofluza), a New Influenza Anti-Viral Medication is FDA Approved, But Does it Work? appeared first on REBEL EM - Emergency Medicine Blog.
