
 Advanced Cardiac Life Support (ACLS) provides a well structured framework for those who resuscitate infrequently. There is room to move beyond the algorithm to potentially provide better care for our patients for those who resuscitate frequently. I will describe some tweaks to the way CPR, defibrillation, and medications are delivered in the arrests I manage.
Advanced Cardiac Life Support (ACLS) provides a well structured framework for those who resuscitate infrequently. There is room to move beyond the algorithm to potentially provide better care for our patients for those who resuscitate frequently. I will describe some tweaks to the way CPR, defibrillation, and medications are delivered in the arrests I manage.
Cardiopulmonary Resuscitation (CPR)
- Team: Performing a successful resuscitation is a team sport. Having a ‘pre-arrival code briefing’ will help to get everyone in the game, and can help to reinforce the goal of high quality, minimally interrupted CPR.
- Quality of CPR: Reinforcing to the ED technicians / students / nurses who will be delivering CPR that they are the most important member of the team helps. I try to have each new compressor match the best end-tidal CO2 that was achieved by the person they are replacing. If the end-tidal starts to fall, I will trade them out early.
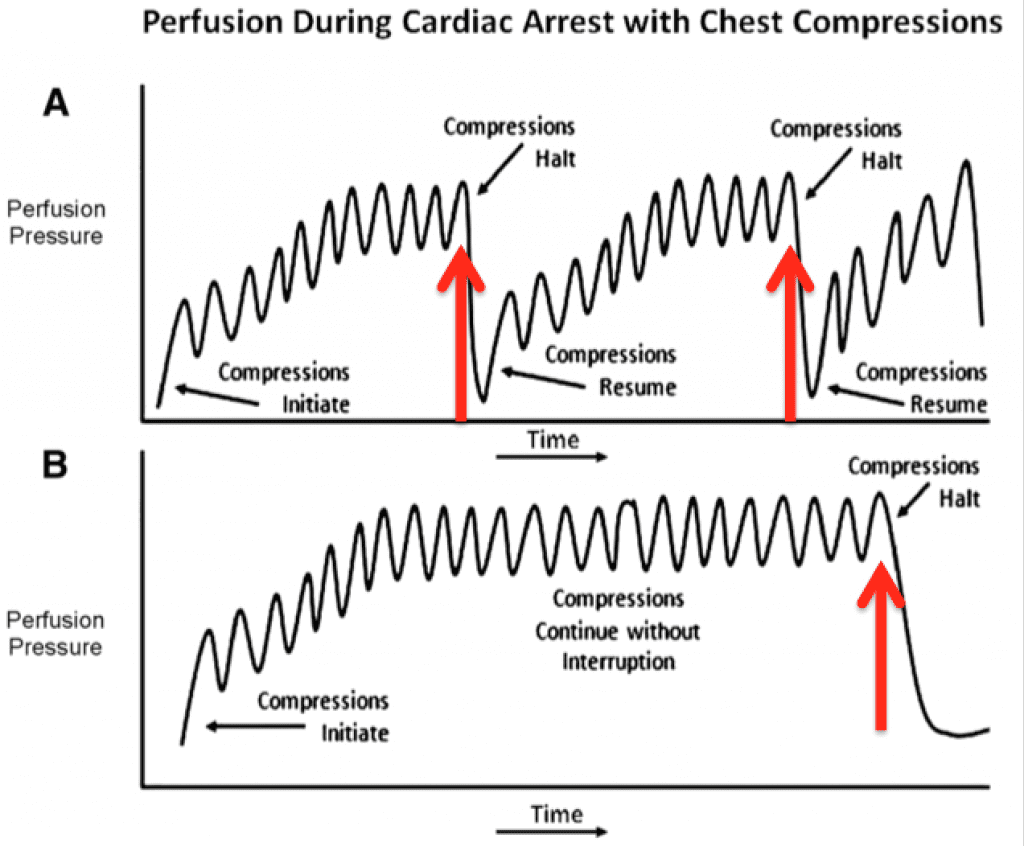
- Interruptions: The ‘pre-arrival code briefing’ also reinforces the need for minimally interrupted CPR. This involves counting out loud during cardiac ultrasound assessments, skipping pulse checks in favor of watching for a bump in the endtidal CO2, and reminding participants that compressions DO NOT need to be stopped during attempts at airway management.
Defibrillation
To minimize the interruption in compressions during defibrillation I will have the provider delivering compressions be the one in charge of calling the shock. Once a shockable rhythm has been identified, compressions will continue while the defibrillator is charging. The compressor will then ‘call the shock’ and say shock in 3, 2, 1, and will lift their hands off the chest for <2 seconds, and then immediately resume compressions and follow the ETCO2 data for evidence of ROSC. This technique requires a pre-resuscitation team briefing. The benefit of this technique is that it involves the ED technicians / nurses / students in the resuscitation and allows them to take an active role in the arrest (rather than being just a human CPR machine), it also allows for a very brief perishock pause.
Drug Dosing
ACLS recommendations: ‘consider epi, 1mg every 3-5 minutes’ allow for some wiggle room in the way we choose to deliver intra-arrest vasopressors.
It can cause undue unrest in your team if you skip the epi entirely without a very lengthy explanation. Epinephrine in cardiac arrest was already covered on REBEL EM (Is It Time to Abandon Epinephrine in Out-Of-Hospital Cardiac Arrest?). I will often hang an epi drip at 0.5 mcg/kg/min instead of having team members distracted by giving epi every 3-5 minutes. For a 100kg patient this will deliver 50 mcg per minute, or 250 mcg every 5 minutes. This dosing level equates to about 25% of ‘code dose’ epi, and should help to support intra-arrest diastolic coronary perfusion without hammering the heart and brain as hard as code dose epi does. This dosing approach treads the middle ground between the group who feel there is no benefit to epi during cardiac arrest, and those that are dosing their epi based on diastolic pressures to enhance coronary artery perfusion.
In the CHEER trial [1], once the decision to initiate E-CPR was made an epi drip was started at 50 mcg/min.(this is the same as 0.5 mcg/kg/min for a 100kg patient) For a full description of their protocol see the link from the ED-ECMO website: ED ECMO from the Alfred
The benefits to the drip are two-fold:
- Cognitive offloading: With the epi drip running, the team member who was having to remember epi every 3-5 minutes can now focus on other aspects of the code (ie, good, minimally interrupted compressions).
- Avoidance of post ROSC drop in BP: With conventional code dose epi administration a big drop in post Return of Spontaneous Circulation Blood Pressure (ROSC BP) can be seen once the epi wears off in patients who will have post ROSC pressor dependent hypotension. With an epi drip already running this post ROSC drop in BP can be averted, or can be identified, and treated more easily. Having an epi drip running also makes managing post ROSC MAP goals easier to achieve.
Running the epi drip is especially useful in those situations where compressions are anticipated to be needed for >15 minutes, i.e. intra arrest lytics for suspected or confirmed massive PE where 2 doses of lytics are given 15 min apart, or during the cannulation phase for E-CPR.
Spend an extra 10 minutes in the room post ROSC

A great piece of advice that was given by Sara Gray (@EmICUcanada) in her talk at SMACC Chicago is to spend an extra ten minutes at the bedside sweating the small stuff after an intubation, or after achieving ROSC.
Optimize Post Arrest Care
- Turn down the FiO2 to avoid hyperoxia (Pa02 >300mmHg) There is a mortality association between elevated post arrest PaO2 and death [2]. Kilgannon et. al. found that every 100mmHg elevation in peak post ROSC Pa02 was associated with a 24% increase in mortality [3].
- Tweak the vent (6cc/kg tidal volume)
- Check cuff pressure on ETT tube [4]
- Optimize temperature: 36 degrees by 4h post ROSC, or sooner if possible
- Optimize Mean Arterial Pressure (MAP)
- Optimize position (head of bed elevation to 30 degrees) [5]
- Confirm cause of arrest (if possible) Make sure that STEMI isn’t a PE, make sure that PE isn’t a STEMI, and ALWAYS consider dissection.
- TEACH: Check with your team if any of the interventions need clarification or explanation. If you are convincing, they will do this for other patients also.
Take Home Points
- Brief your team before patient arrival: CPR quality (ETCO2), limit all pauses, and smarter Defibrillation
- Consider an epi drip instead of code dose epi pushes: 0.5 mcg/kg/min IV/IO
- Sweat the small stuff after you get ROSC. 10 min is a small investment for improved patient outcomes
- TEACH
I am far from an expert resuscitationist, but these simple interventions have allowed for a calmer, quieter room during cardiac arrest resuscitations, and a realization that I am providing the best care possible for my patients.
References:
- Stub D et al. Refractory Cardiac Arrest Treated with Mechanical CPR, Hypothermia, ECMO and Early Reperfusion (The CHEER Trial). Resuscitation 2015. PMID: 25281189
- Wang CH et al. The Effect of Hyperoxia on Survival Following Adult Cardiac Arrest: A Systematic Review and Meta-Analysis of Observational Studies. Resuscitation 2014. PMID: 24892265
- Kilgannon JH et al. Relationship Between Supranormal Oxygen Tension and Outcome After Resuscitation from Cardiac Arrest. Circulation 2011. PMID: 21606393
- Hoffman RJ et al. Experienced Emergency Medicine Physicians Cannot Safely Inflate or Estimate Endotracheal Tube Cuff Pressure Using Standard Techniques. Am J Emerg Med 2006. PMID: 16490640
- Grap MJ et al. Ventilator-Associated Pneumonia: The Potential Critical Role of Emergency Medicine in Prevention. J Emerg Med 2012. PMID: 20692786
Also Checkout:
- Bryan Hayes at ALiEM: The Dirty Epi Drip – IV Epinephrine When You Need It
Post Peer Reviewed By: Salim Rezaie (Twitter: @srrezaie)
The post Beyond ACLS: CPR, Defibrillation, and Epinephrine appeared first on REBEL EM - Emergency Medicine Blog.
