
 Background: CCTA has become a popular modality in the ED setting to assess anatomic atherosclerotic disease in patients presenting with chest pain. Advocates of CCTA feel that CCTA has a greater accuracy in identifying obstructive coronary artery disease and identification of high-risk disease compared to standard physiologic testing. However, many published trials on CCTA were not adequately powered to evaluate patient oriented end points. The aim of the current published study was to perform a systematic review and meta-analysis comparing CCTA with other standard of care (SOC) approaches in evaluation of patients with acute chest pain.
Background: CCTA has become a popular modality in the ED setting to assess anatomic atherosclerotic disease in patients presenting with chest pain. Advocates of CCTA feel that CCTA has a greater accuracy in identifying obstructive coronary artery disease and identification of high-risk disease compared to standard physiologic testing. However, many published trials on CCTA were not adequately powered to evaluate patient oriented end points. The aim of the current published study was to perform a systematic review and meta-analysis comparing CCTA with other standard of care (SOC) approaches in evaluation of patients with acute chest pain.
What They Did: This was a systematic review and meta-analysis of randomized trials published in peer-reviewed journals comparing CCTA to physiologic testing in patients with acute chest pain
Outcomes:
-
Primary Outcomes:
- All-cause mortality
- Major Adverse Cardiac Events (MACE)
- Myocardial infarction (MI)
- Invasive coronary angiography (ICA)
- Revascularization
-
Efficiency Outcomes:
- Length of stay
- Cost of acute care
Inclusion:
- Randomized trials published in peer-reviewed journals
- No language restrictions
- Reported clinical outcomes
- Studies included patients presenting with acute chest pain (ED and/or inpatient)
- Studies required non-ischemic ECG and/or negative cardiac biomarkers
Exclusion:
- Observational studies
- Abstracts
- Case series and case reports
- Individual study exclusions:
- Pregnancy
- Renal failure
- Allergy to iodine contrast
- Inability to obtain informed consent
- 8 out of 10 studies excluded patients with known coronary artery disease
Results:
- 10 trials with 6,285 patients were included
- Studies published between 2007 – 2016
- Follow up period for included studies ranged from 1 -12 months for ED studies and 7 – 19 months for inpatient studies
- All-cause mortality: RR 0.48; 95% CI 0.17 – 1.36; p = 0.17
- MI: RR 0.82; 95% CI 0.49 – 1.39; p = 0.47
- MACE: RR 0.98; 95% CI 0.67 – 1.43; p = 0.92
- ICA: RR 1.32; 95% CI 1.07 – 1.63; p = 0.01
- Revascularization: RR 1.77; 95% CI 1.35 – 2.31; p<0.0001
- No difference in MI, MACE, or all-cause mortality, but an increase in invasive coronary angiography and revascularization
- 7 studies reported repeat ED visits and 9 reported repeat hospitalizations after index evaluation for chest pain. There was no statistical difference in either of these endpoints
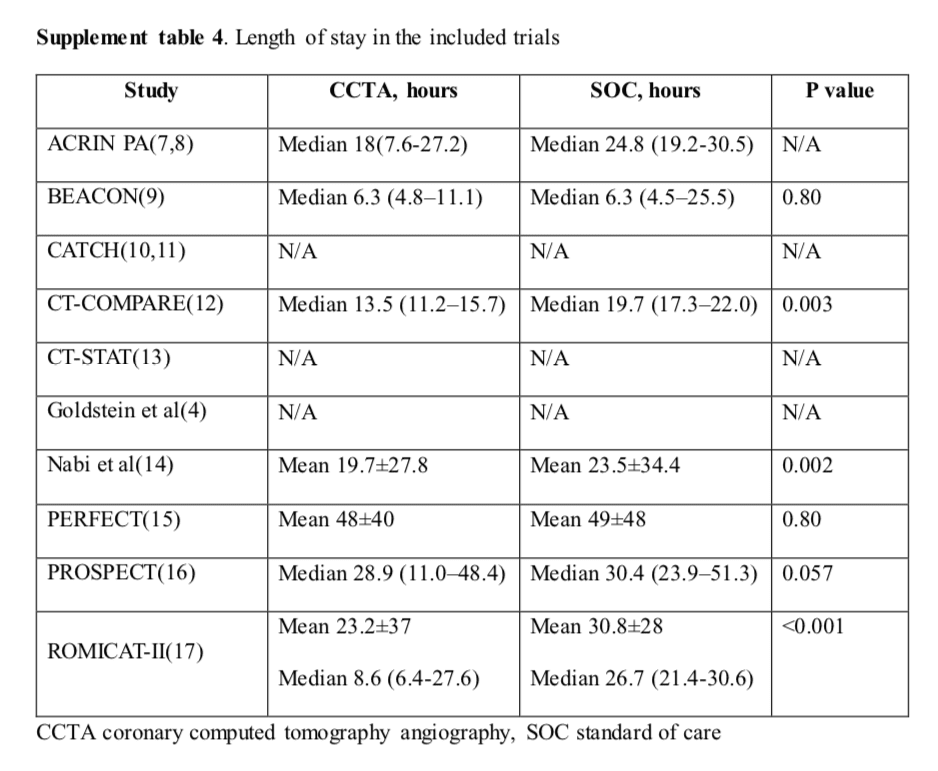
- 10 studies reported length of stay in the included trials and overall the length of stay was shorter with CCTA
- 10 studies reported cost of acute care in the included trials and overall the cost of care was significantly less with CCTA

Strengths:
- Meta-analysis was performed based on PRISMA meta-analyses statement
- Only randomized trials published in peer-reviewed journals were considered for meta-analysis
- Cochrane collaboration tool for assessing bias in randomized tool was used and there was no evidence of high-risk bias found in the included studies
Limitations:
- The included trials used different definitions and implementation for SOC, but all used physiologic testing such as stress electrocardiography, stress echocardiography, and myocardial perfusion imaging as the comparator
- The results of this study are only applicable to short-term clinical outcomes
- The number of mortality events were very low and the mortality comparison should be interpreted with caution
- The use of stress electrocardiography as a comparator arm in some studies performed may exaggerate the benefits of CCTA-based strategy due to a relatively inferior performance in ischemia detection compared with stress imaging
- Only a small number of included studies prespecified the criteria for downstream testing such as invasive angiography based on the findings on CCTA and/or functional testing leaving the decision to the management up to the treating physician
- The issue of radiation exposure pertinent to different testing strategies was not addressed by this review
- This study also did not study the long-term effect of diagnostic strategy on subsequent testing and treatment as well as quality of life
Discussion:
- TIMI scores used in the included studies were low, therefore, these studies assessed low-risk and low-to-intermediate risk patients with a low expected adverse cardiac event rate
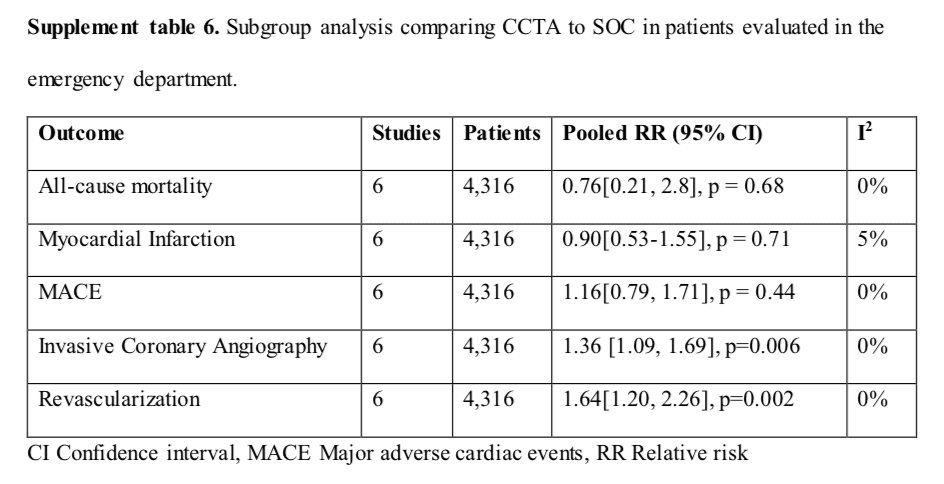
- Subgroup analysis of ED studies showed no differences in all-cause mortality, MI, and MACE between CCTA vs SOC approaches, but the ICA and revascularization rates were significantly higher in the CCTA group
- It is unclear if detection of anatomic coronary artery disease may benefit from prompt adjustment of medical management (i.e. lipid-lower therapy, lifestyle modification, etc…) to decrease long-term risk of acute coronary events and requires further study in prospective trials (i.e. invasive strategy vs medical management modification)
Author Conclusion: “Compared with other SOC approaches use of CCTA is associated with similar major adverse cardiac events but higher rates of revascularization in patients with acute chest pain.”
Clinical Take Home Point: In patients that are deemed “low risk” for atherosclerotic disease, with no previous diagnosis of coronary artery disease the use of CCTA compared to standard of care physiologic testing decreases length of stay, increases downstream testing (invasive coronary angiography and revascularization), without any patient oriented benefit all-cause mortality, MI, MACE) and should not be used in this patient population.
References:
- Gongora CA et al. Acute Chest Pain Evaluation using Coronary computed tomography Angiography Compared with Standard of Care: A Meta-Analysis of Randomised Clinical Trials. HEART 2018. PMID: 28855273
Post Peer Reviewed By: Rick Pescatore, DO (Twitter: @Rick_Pescatore)
The post Coronary Computed Tomography Angiography (CCTA): The Holy Grail of “Low Risk” Chest Pain Evaluation? appeared first on REBEL EM - Emergency Medicine Blog.
