
 Background: Emergency Medicine clinicians must be adept in the management of the agitated patient. While verbal de-escalation techniques should be attempted, they are often inadequate. The next option after attempts at verbal de-escalation is chemical restraint with medications to help with a more rapid decline in agitation. Although it is agreed that IM antipsychotics or benzodiazepines are first line medications to treat agitation, there is no consensus on any one single agent. The big question therefore, still remains however of what medications should we use and at what dose? There are numerous papers investigating the utility of various medications. Today, we look at a comparison of droperidol, ziprasidone and lorazepam.
Background: Emergency Medicine clinicians must be adept in the management of the agitated patient. While verbal de-escalation techniques should be attempted, they are often inadequate. The next option after attempts at verbal de-escalation is chemical restraint with medications to help with a more rapid decline in agitation. Although it is agreed that IM antipsychotics or benzodiazepines are first line medications to treat agitation, there is no consensus on any one single agent. The big question therefore, still remains however of what medications should we use and at what dose? There are numerous papers investigating the utility of various medications. Today, we look at a comparison of droperidol, ziprasidone and lorazepam.
Article: Martel ML et al. Randomized Double-blind Trial of Intramuscular Droperidol, Ziprasidone, and Lorazepam for Acute Undifferentiated Agitation in the Emergency Department. Acad Emerg Med 2020. PMID: 32888340 [Open in Read by QxMD]
Clinical Question: Which intramuscular medication, droperidol, ziprasidone or lorazepam, is most effective in achieving sedation of undifferentiated agitated patients in the ED at 15 minutes?
Population: Emergency department patients >18 years old with acute agitation if treating physician determined there was a need for parenteral medications for agitation.
Outcomes:
- Primary: Proportion of patients adequately sedated at 15 minutes using the Altered Mental Status Scale (AMSS) and Behavioral Activity Rating Scale (BARS) scores
-
Secondary:
- Rate of rescue medication
- Respiratory depression (Sp02 <90%, requiring supplemental O2 or decrease in ETCO2 >10mmHg or increase in ETCO2 >15mmHg)
- Adverse medication effects (Akathisia, dystonia, or allergic reaction)
- ED length of stay
Intervention: Droperidol 5mg, Ziprasidone 10mg, Ziprasidone 20mg, Lorazepam 2mg
Design: Prospective randomized double-blind trial with pairwise comparison of treatment arms
Excluded:
- Prisoners
- Previously enrolled in trial
- Known to be pregnant or breast feeding
- Allergy to any of the study medications
Primary Results:
- Study performed in a single, large urban ED
- 149 patients screened for study eligibility, 34 deemed ineligible. 115 patients enrolled
- Median age 40 years
- 87 were male (76%)
- Alcohol Intoxication was very common (Range 79 to 94% of cohorts)
Critical Findings:
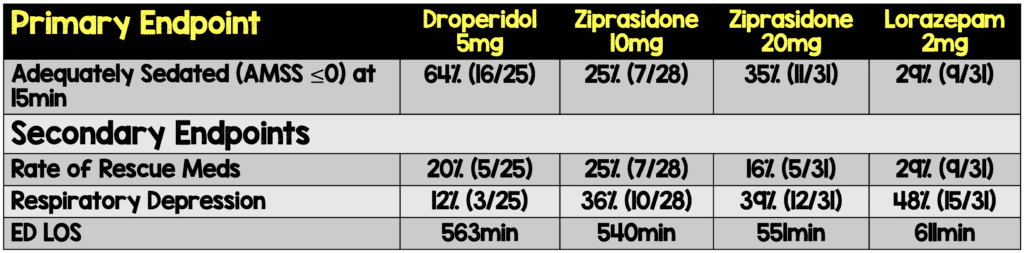

- Median Corrected QT
- Droperidol: 413ms
- Ziprasidone 10: 410ms
- Ziprasidone 20: 428ms
- Lorazepam: 414ms
- P = 0.52
Strengths:
- Double-blind randomized control trial
- Randomization and blinding appropriately performed
- Addresses a clinically important question
- Focuses on ED specific patients and outcomes
- Baseline AMSS scores similar between groups
- Doses of medications used in this trial were derived from information from preceding RCTs
- Since no dose-finding study of ziprasidone, authors included 10mg and 20mg to determine if a smaller dose would be as effective, with fewere side effects, and shorter duration of sedation
- Recorded multiple outcomes including AMSS, BARS, etCO2, and SpO2 at time of medication administration, 15, 30, 45, 60, 90, and 12 minutes after medication administration.
Limitations:
- Study was conducted at a single center with a dedicated agitation, intoxication unit
- Convenience sample of patients – vulnerable to selection bias which makes this less generalizable
- Small study with small individual treatment groups
- 34 patients excluded from randomization but, the researchers are not aware of why they were excluded
- Majority of patients agitated secondary to alcohol. Results may not apply to other reasons for agitation
- Age of the data: Initially collected in 2005 and published in 2020, prevalence of amphetamines and other drugs has increased
- There was significantly more head injury in the Ziprasidone and Lorazepam groups compared to Droperidol (29% vs 23% vs 16% vs 4% respectively)
- Due to small size of study, and rarity of adverse events it is difficult to draw meaningful assessments of safety (i.e. QTc prolongation, dyskinesia, etc…)
Discussion:
- IM droperidol is an ideal agent for agitated patients:
- Quick On: Rapid absorption via IM route (≈5min)
- Quick Off: Half-life of 2.3hrs
- Although there was more respiratory depression with ziprasidone and lorazepam compared to droperidol, this was driven almost entirely by changes in etCO2 as hypoxia did not differ between groups
- Don’t forget majority of patients in this study were alcohol intoxication patients who have higher risk for respiratory depression at baseline
- IM Droperidol was found to be superior to IM Lorazepam or IM Ziprazidone at two doses for the treatment of acute undifferentiated agitation in the ED. Fewer patients receiving droperidol had respiratory complications and more desirable sedation levels.
- Lorazepam resulted in slower time to adequate sedation, increased need for rescue sedation and increase in adverse events compared to droperidol.
- Ziprasidone had no difference in sedation at 15 minutes, adverse effects, rescue medications or total time in ED at either dose. 10mg dose of Ziprasidone did have a 40-minute shorter time of “ready for ED discharge” than that of the 20mg dose
- This was a well-done double-blind study with appropriate randomization done looking at a clinically important question focused on the ED.
- The study is limited by the fact it was done by convenience sampling which could lead to sampling bias, was a small study with small groups.
- With the study being so small the confidence intervals are rather large meaning that it is difficult to draw conclusions as to just how effective the medication really is.
Authors Conclusions: “Droperidol was more effective than lorazepam or either dose of ziprasidone for the treatment of acute agitation in the ED and caused fewer episodes of respiratory depression.”
Our Conclusions: We believe this is a well-done pilot study that gives us clear indication that droperidol is safe and very effective at getting adequate sedation for the agitated patient. However, with its potential sampling bias and overall small numbers a larger study should be undertaken to confirm the data found.
Potential to Impact Current Practice: With Droperidol being placed again on hospital formularies this medication is again finding many uses. This study shows just how effective it is in treating the agitated patient. Along with ketamine, Droperidol is becoming an EM darling medication.
Bottom Line: Droperidol appears to be the superior medication for rapid sedation of the agitated patient in comparison to lorazepam or ziprasidone.
References:
- Martel ML et al. Randomized Double-blind Trial of Intramuscular Droperidol, Ziprasidone, and Lorazepam for Acute Undifferentiated Agitation in the Emergency Department. Acad Emerg Med 2020. PMID: 32888340 [Open in Read by QxMD]
For More on This Topic Checkout:
- REBEL EM: Comparison of IM Midazolam, Olanzapine, Ziprasidone, and Haloperidol for Behavioral Control
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami) and Salim R. Rezaie, MD (Twitter: @srrezaie)
The post Droperidol Reigns Supreme appeared first on REBEL EM - Emergency Medicine Blog.
