
 Babesiosis
Babesiosis
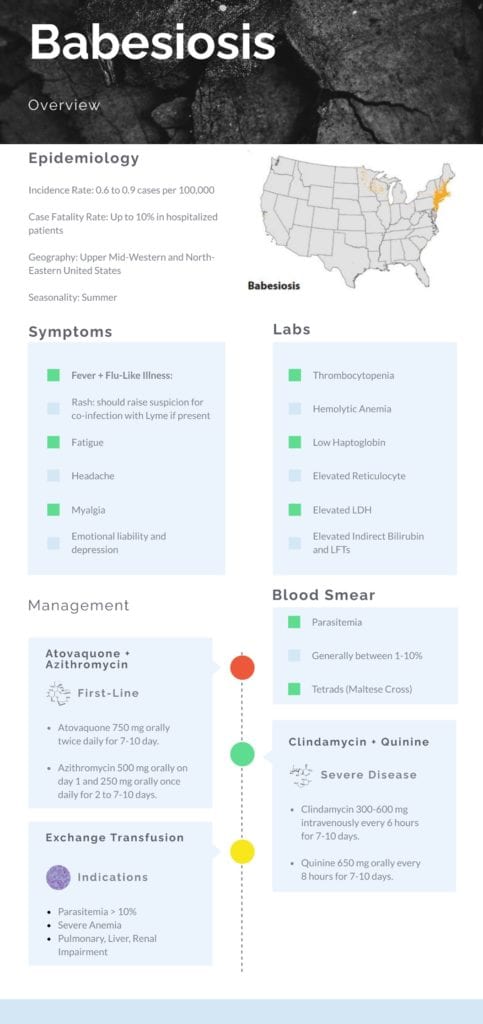
Epidemiology
Incidence:
- Overall annual incidence rose from 0.6 to 0.9 cases per 100,000 in the United States between 2012 and 2015 (Gray 2019)
- Annual incidence is highest in those between 60-69 years of age (Gray 2019)
Age:
- Median age is 63 years of age with greater than 89% of cases reported in Caucasian patients (Gray 2019 2010)
Gender:
- Male to female predominance (Gray 2019)
Morbidity/Mortality:
- Overall hospitalization rates for confirmed cases are noted to range from 16% to 72.6% depending on the patient’s age (Gray 2019)
- Mortality rates up to 10% have been noted in hospitalized patients (Vannier 2015)
- Mortality rates are much higher among immunocompromised patients and those who acquired the illness through blood transfusion
Geography and Seasonality (Gray 2019): Cases predominately in the Northeastern and Upper Midwestern United States
- Seven States account for over 94% of all reported cases:
- New York
- Massachusetts
- Connecticut
- New Jersey
- Rhode Island
- Wisconsin
- Minnesota
- Seasonal distribution is concentrated in June, July, and August
Poor Prognostic Factors (Vannier 2015):
- Neonates and > 50 years of age
- Coinfection with Lyme Disease
- Immunocompromised states
- Delays in diagnosis and treatment
- Asplenia
Pathogenesis (Krause 2019):
- After tick transmissibility, Babesia species, an intraerythrocytic protozoa, will mature, replicate, and release into the bloodstream to invade nearby red blood cells
- This infection leads to erythrocyte lysis, metabolic alterations, proinflammatory cytokine production, and obstruction of blood vessels
History and Physical:
Symptoms (Vannier 2015):
- Symptoms typically appear 1-4 weeks after bite of an infected tick
- Rash is not a common occurrence unlike other tick-borne illnesses
- If present, it should raise the suspicion for co-infection with Lyme disease
- Fever occurs in 89% of recognized cases of babesiosis along with other non-specific flu-like symptoms:
- Fatigue
- Chills
- Headache
- Anorexia
- Myalgia
- Emotional liability and depression
- Gastrointestinal symptoms are often seen
- Physical Examination:
- Mild splenomegaly and hepatomegaly are sometimes found on examination
- Jaundice and dark urine are sometimes found on examination due to intravascular hemolysis
- Severe Manifestations: Most cases are self-limiting, but Babesiosis has been associated with the following severe disease manifestations:
- ARDS
- Renal Failure and Hepatic Failure
- Rhabdomyolysis
- DIC
- Heart Failure
- Coma
- Splenic Rupture
- Hemophagocytic Syndromes
Diagnosis:
Labs: Characteristic laboratory findings are seen in Babesiosis along fever and non-specific flu-like illness:
- Thrombocytopenia
- Hemolytic Anemia
- Low Haptoglobin Level
- Elevated Reticulocyte Count
- Elevated LDH Level
- Elevated Indirect Bilirubin and Mildly Elevated Hepatic Transaminase
Blood Smear (Vannier 2015):
- Diagnosis can be made with visualization of Babesia parasites on Giemsa or Wright stained thin blood smears.
- The level of parasitemia is typically between 1 and 10% but can be as high as 80% in severe disease.
- Babesia species sometimes exhibit the presence of tetrads (Maltese cross) and have the absence of hemozin deposit in the ring form as well as lack banana-shaped shaped gametocytes, thus distinguishing them from plasmodia species.
Confirmatory Testing:
- Serological testing of IgM and IgG antibodies specific to Babesia species using indirect immunofluorescence assay (IFA) is available for confirmation.
- RT-PCR assays are also available for diagnosis of Babesiosis with have high sensitivity and specificity.
Guest Post By:

Akash Ray, DO
PGY-2 Emergency Medicine Resident Inspira Medical Center
Vineland, NJ
Twitter: @_kashray
References:
- Biggs H et al. Diagnosis and Management of Tickborne Rickettsial Diseases: Rocky Mountain Spotted Fever and Other Spotted Fever Group Rickettsioses, Ehrlichioses, and Anaplasmosis – United States. MMWR Recomm Rep. 2016. PMID: 27172113
- Gray E et al. Babesiosis Surveillance – United States, 2011-2015. MMWR Surveill Summ. 2019. PMID: 31145719
- Vannier E et al. Babesiosis. Infect Dis Clin North Am. 2015. PMID: 25999229
- Krause P. Human babesiosis. Int J Parasitol. 2019. PMID: 30690090
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post Emerging Tick-Borne Illnesses: Not Just Lyme Disease Part 5 Babesiosis appeared first on REBEL EM - Emergency Medicine Blog.
