
 Background: Rapid sequence intubation (RSI) involves the use of an induction agent followed by a neuromuscular blocking (NMB) agent to obtain optimal intubating conditions. Administration of a NMB results in apnea which, in turn, can lead to oxygen desaturation. Oxygen desaturation during rapid sequence intubation may lead to serious adverse events including dysrhythmias, hypotension, and cardiac arrest. Preoxygenation helps extend the duration of safe apnea and has 2 major goals:
Background: Rapid sequence intubation (RSI) involves the use of an induction agent followed by a neuromuscular blocking (NMB) agent to obtain optimal intubating conditions. Administration of a NMB results in apnea which, in turn, can lead to oxygen desaturation. Oxygen desaturation during rapid sequence intubation may lead to serious adverse events including dysrhythmias, hypotension, and cardiac arrest. Preoxygenation helps extend the duration of safe apnea and has 2 major goals:
- Attempt to achieve an O2 saturation of 100%
- Maximize oxygen storage in the lungs by denitrogenation of the residual capacity of the lungs (Approximately 95% of oxygen reservoir)
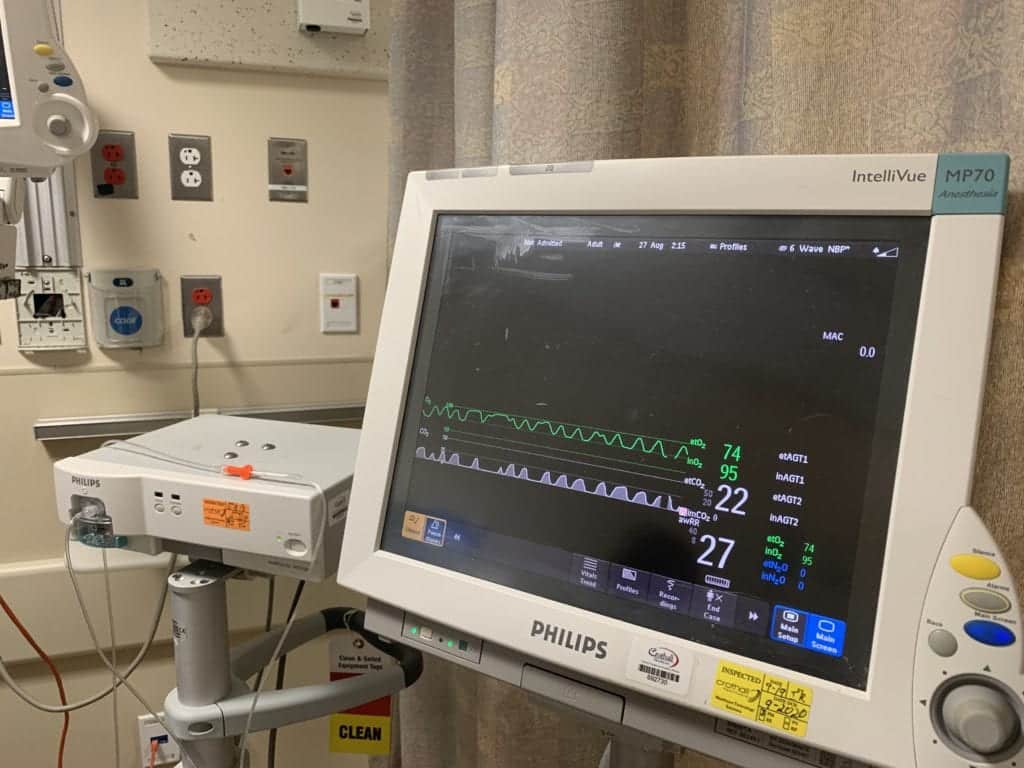
Preoxygenation is assessed in the ED but usually through pulse oximetry which is inadequate. In the operating room, anesthesiolgists use gas analyzers to quantify and optimize preoxygenation with ETO2. In critically ill patients, preoxygenation should be performed to achieve an ETO2 ≥85% based on the response to the 4th National Audit Project of the Royal College of Anaesthetists and Difficult Airway Society [2].
What They Did:
- Describe the preliminary use of ETO2 to assess quality of preoxygenation by various methods during RSI in the ED via a prospective observational cohort study at 2 academic EDs
- Used standard gas analyzer to measure ETO2
- ETO2 was measured before preoxygenation and at time of RSI medications (after preoxygenation)
- A minimum of 3 minutes of preoxygenation was mandated with either a BVM device or a NRB mask before RSI
- In the BVM group, PEEP could be provided via an end-expiratory pressure valve at pressures ranging from 1 to 20 cmH20
- In the NRB mask, O2 flow rate was set at 15LPM or flush rate (50 – 70 LPM at one site and 19LPM at the other site)
- Use of supplemental nasal cannula O2 was chosen by ED physician and ranged from 15LPM to flush rate
- Hypoxemia defined as SpO2 <90%
Outcomes:
- Primary: ETO2 level measured before preoxygenation and at induction (after preoxygenation)
- Secondary: SpO2 measured before and immediately after intubation
Inclusion:
- ≥18 years of age
- Undergoing rapid sequence intubation in the ED
Exclusion:
- Cardiac arrest
- Receiving noninvasive ventilation prior to intubation
- Intubated in the out-of-hospital setting
- Underwent awake intubation
Results:
- 100 patients included
- First pass success rate = 90% (All patients were intubated within 2 attempts)
- Median ETO2 level before preoxygenation = 53% (Range: 43 – 65%)
- Median ETO2 level after preoxygenation = 78% (Range: 64 – 86%)
- 25% of patients achieved an ETO2 ≥85%
- Median ETO2 Level:
- NRB: 80% (Range: 60 – 87%)
- BVM: 77% (Range: 65 – 86%)
- Highest Median ETO2 = NRB at flush rate oxygen 86% (Range 80 – 90%)
- Lowest Median ETO2 = NRB at 15LPM 57% (Range: 53 – 60%)
- SpO2 <90% at Any Time = 18pts (18%)
- Of these 14/18 (78%) did not reach ETO2 >85% at induction
- SpO2 <80% at Any Time = 2pts (2%)
- O2 saturation was higher during RSI when higher ETO2 levels were achieved by induction
Strengths:
- Study assesses the quality of preoxygenation prior to RSI intubation in critically ill patients
- ED physicians were blinded to the ETO2 data during the procedure
- Independent observers collected all ETO2 measurements
- Data collected in real time
- Used waveform capnography to verify that ventilation was occurring during ETO2 measurement
- Validated single vs continuous breath ETO2 measurements with a preliminary study using 4 healthy volunteers (attained 20 measurements at each site)
- Had objective definitions of preoxygenation interval and apnea time
- Tested interrater agreement for ETO2 and SpO2 by using the first 5 cases
Limitations:
- Study centers were academic EDs with training programs and thus the results may not generalize to nonacademic centers
- Differing techniques of preoxygenation were not associated with patient outcomes or adverse events
- Measurements of continuous monitoring may be slightly higher than single breath measurements in critically ill patients due to oxygen mixing from the source in the mask when the patient is not ventilating adequately
- ETO2 is a measure of the concentration of O2 in the functional reserve capacity.Critically ill patients may achieve a high ETO2 but still have a short safe apnea time due to reduced functional reserve capacity, increased oxygen consumption, or both
- Looked at a surrogate monitor-oriented outcome (MOO) not a patient oriented outcome (POO)
- ETO2 device is not readily available in the vast majority of EDs
Discussion:
- As this is the first study to try and quantify preoxygenation strategies in the ED, these results need to be validated prior to use
- The authors do a nice job explaining potential causes of the low percentage of patients achieving ETO2 levels ≥85%. Approximately 25% of patients were not able to be preoxygenated to an ETO2 of ≥85%. Causes for this include low FiO2 from inadequate oxygen flow or leaks in the face mask seal. Another cause may be that 3 minutes may not be sufficient for some patients to achieve denitrogenation
Author Conclusion: “ETO2 varied with different preoxygenation techniques employed in the emergency department. Most patients undergoing rapid sequence intubation did not achieve maximal preoxygenation. Measuring ETO2 in the emergency department may be a valuable adjunct for optimizing preoxygenation during emergency airway management.”
Clinical Take Home Point: Although the results of this study still need to be validated before implementation in critically ill patients in an ED setting, ETO2 shows promise in quantifying preoxygenation so that preoxygenation may be optimized during ED airway management.
Thoughts from Lead Author Nick Caputo, MD

Associate Chief, Department of Emergency Medicine NYC H+H/Lincoln
Associate Professor of Clinical Emergency Medicine, Weill Medical College of Cornell University
NYC H+H/Lincoln, South Bronx, NY
New York Presbyterian/Columbia University Medical Center, New York, NY
New York, NY
Twitter: @NickMD1980
Do you have any other thoughts on ETO2?
There’s not much to add to this write up. You guys did a great job. I would say that there are instances where the numbers will “lie”, i.e. if the patient is not ventilating then the FiO2 and the ETO2(FeO2) will quickly equalize. In these cases you are not preoxygenating the patient, its just the sampler reading the gas stuck in the line from lack of flow. This is why it is important to look at the waveforms. If there’s no waveform, there no flow. Also, you are correct, you can have a high ETO2 and yet still desat rapidly, especially if you have not attained a SpO2 of 100% (fully saturating the hemoglobin-which is the start of preox, not the end!). In these situations, it is likely the patient has major shunting (>25% of lung volume) going on and supplement will not overcome that without positive pressure ventilation. The point being, ETO2 in itself gives us an objective measure of one aspect of optimizing our patients for RSI. We can not ignore SpO2, ETCO2 or waveforms. All are equally important to optimize our patients for RSI.
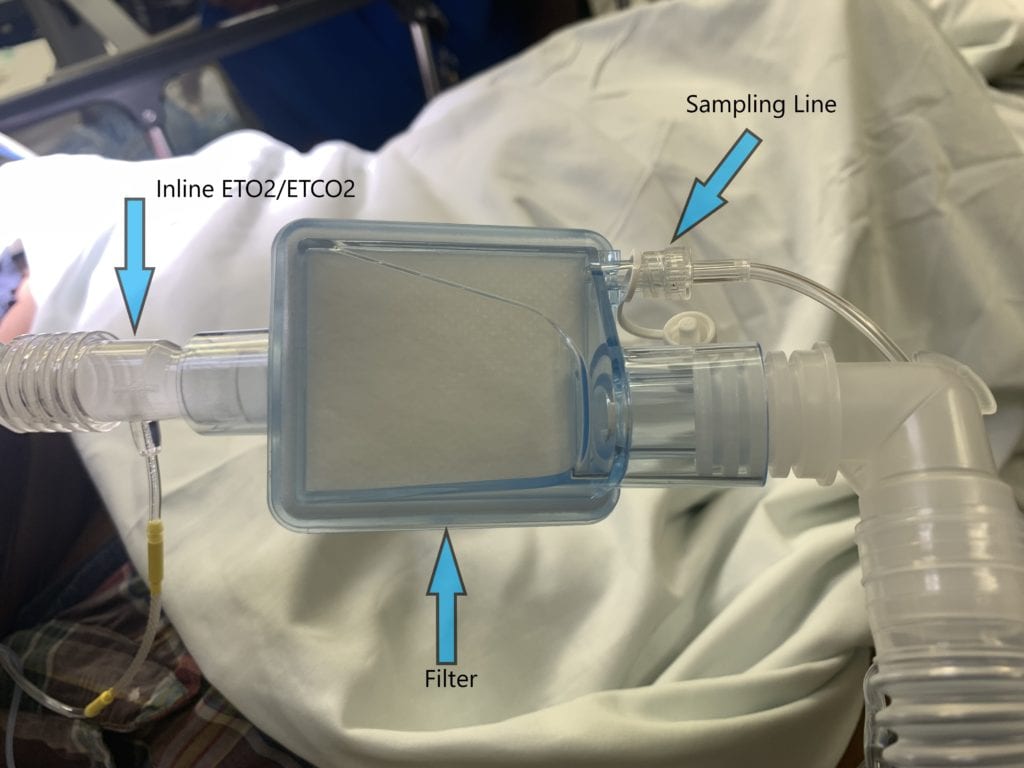
Do you have pictures of the ETO2 analyzer and willing to share and describe how you apply this onto the patient at the bedside as many ED providers, including myself may not be familiar with the device?
The process of set up is similar to that of ETCO2. If the patient is intubated you connect the sampling line to the filter on the vent tubing, or if you do not have a filter on the vent tubing you can use the same inline connector that you would use for your ETCO2. If the patient is not intubated than you connect the sidestream nasal cannula to the sampling line.

What is the future work you are doing on ETO2?
Currently our group has finished the second phase of this three phase study. Phase 1 (the current publication) sought to determine what the efficacy of current conventional preox is that we are performing everyday in ERs across the world. Phase 2 looked to determine whether or not having access to ETO2 improved preox/denitrogenation by means of an objective measure (ETO2 monitoring) like is done in the OR (spoiler alert, we found that when using ETO2 monitoring the average ETO2 was higher and the rates of attaining the goal of ETO2 >85% was better as compared to the Phase 1 data. We also found less desaturation rates when ETO2 was higher. Phase 3 of the study is a planned RCT using the data from Phase 1 and 2 to generate a sample size and power analysis to test whether or not the difference found are true.
We are also conducting a study on de-oxygenation. Basically with the debate about whether or not we should be bagging through the apnea period, we wanted to see what impact does breathing having on ETO2 levels (i.e. you just spent at least 3 minutes washing out nitrogen from the FRC to maximize duration of apnea without desaturation. If the patient is breathing for some time through the early stages of the apnea period, how much of that washout did you just loose?). We are doing this by preoxygenating healthy volunteers to an ETO2 >85%, then measuring the ETO2 every 5 seconds to determine the delta ETO2 or rate of loss of ETO2.
References:
- Caputo N et al. Use of End Tidal Oxygen Monitoring to Assess Preoxygenation During Rapid Sequence Intubation in the Emergency Department. Ann Emerg Med 2019. PMID: 20879700
- Higgs A et al. Guidelines for the Management of Tracheal Intubation in Critically Ill Adults. Br J Anaesth 2018. PMID: 29406182
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post ETO2: The Future of RSI Preoxygenation in the ED? appeared first on REBEL EM - Emergency Medicine Blog.

