
 Background: Rapid sequence intubation (RSI) induction agent selection remains a heavily debated matter. Etomidate causes adrenal suppression in critically ill patients triggering a groundswell of support in favor of ketamine. (Albert 2011, Jabre 2009) However, the existing literature comparing etomidate and ketamine is conflicting.
Background: Rapid sequence intubation (RSI) induction agent selection remains a heavily debated matter. Etomidate causes adrenal suppression in critically ill patients triggering a groundswell of support in favor of ketamine. (Albert 2011, Jabre 2009) However, the existing literature comparing etomidate and ketamine is conflicting.
In 2017, a single-centered, retrospective study found a lower incidence of clinical hypotension with ketamine compared to etomidate following endotracheal intubation in septic patients. (Van Berkel 2017) In 2020 the NEAR study reported peri-intubation hypotension rates of 18.3% in the ketamine cohort compared to 12.4% in the etomidate cohort. (April 2020) RebelEM recently reviewed The EvK trial, which found a higher 7-day survival rate with ketamine but no difference in 28-day survival. However, the numerous methodological concerns and high risk for bias trigger skepticism about the validity of the results. (Matchett 2022).
In this post, we critically appraise the first systematic review and meta-analysis to compare the safety and efficacy of etomidate and ketamine as induction agents for RSI in the ED and prehospital setting.
Article: Sharda SC et al. Etomidate Compared to Ketamine for Induction during Rapid Sequence Intubation: A Systematic Review and Meta-analysis. Indian J Crit Care Med 2022. PMID: 35110853
Clinical Questions: Which induction agent (etomidate or ketamine) for RSI causes higher rates of post-induction hypotension?
What They Did:
- Performed a search of the following databases: Pubmed, Embase, Cochrane, and ClinicalTrials.gov up to and including June 1, 2021.
- The articles were analyzed and extracted for data points relevant to post-intubation hypotension and first-pass intubation success rates.
- Patients were excluded with pre-induction hypotension defined as SBP <100 mmHg. Immediate post-induction hypotension (<1h) was prioritized as a data point over delayed hypotension at any interval over 24 h. Pooled data from ED and prehospital were evaluated using an odds ratio with a 95% confidence interval.
Inclusion:
- Articles compared the safety and efficacy of etomidate compared to ketamine, in patients of all age groups, as induction agents for RSI in the Emergency Department (ED) and prehospital settings.
Exclusion:
- Articles were excluded if they included combinations of two or more induction agents.
Outcomes:
- Primary Outcome: Incidence of post-induction hypotension
- Secondary Outcome: First-pass success rate of endotracheal intubation
Primary Results:
- 84 articles were identified for potential inclusion.
- Articles removed were duplicates, contained irrelevant outcomes, or had a significant risk for bias.
- 9 studies were included in the meta-analysis.
Post-Induction Hypotension
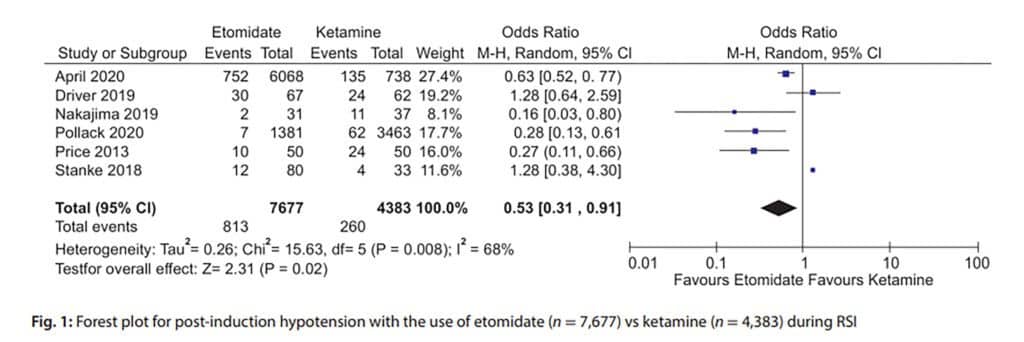
- Data from 6 of 9 studies were pooled with 12,060 patients prehospital and ED.
- Etomidate was shown to have a statistically significant decreased risk of post-induction hypotension vs. ketamine (OR: 0.53, 95% CI: 0.31 – 0.91; p = 0.02)
First-Pass Success
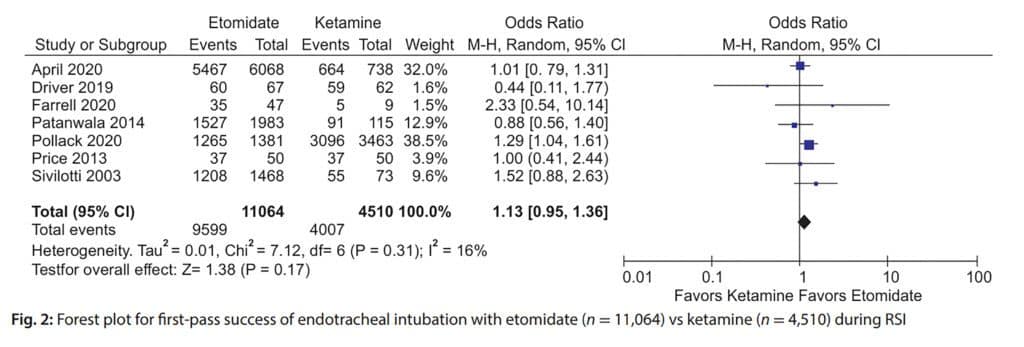
- Data from 7 of 9 studies were pooled with 15,574 patients prehospital and ED.
- There was no difference in first-pass intubation success when comparing the etomidate vs. ketamine. (OR: 1.13; 95% Cl: 0.95-1.36; p = 0.17)
Strengths:
- Investigators asked a patient-centered, narrowly focused, heavily debated clinical question.
- Performed a comprehensive search of multiple large databases (Pubmed, Embase, Cochrane, and ClinicalTrials.gov).
- Investigators used a validated tool to assess the quality of evidence—Oxford Centre for Evidence-Based Medicine: Levels of Evidence.
- All included studies received a level 3 or higher—equivalent to Grade recommendation B.
- The authors provided an analysis of bias and explicitly described the risk of bias in each included study.
- Assessed the consistency of results across studies with heterogeneity variance evaluation.
- The pooled sample sizes from included studies were large, with >12,000 patients for hypotension and >15,000 patients for first-pass success.
Limitations:
- Non-English papers were excluded.
- Bibliographies of included studies were not searched.
- Investigators did not report on how disagreements from reviewers were resolved.
- It is unclear if researchers followed specific validated systematic review process guidelines such as PRISMA.
- It is unclear what tool for bias assessment was used, such as the Cochrane collaboration risk of bias assessment.
- Only 2 of the 9 included studies were randomized controlled trials, and only 1 of the remaining 7 studies was a prospective comparative study.
- Included trials were mostly observational or retrospective. There are lots of confounding variables not accounted for, such as difficult airway, the experience of the intubating physician, the use of difficult airway adjuncts, etc.
- Granular details of the dosing of induction agents were not given.
- Why one agent was chosen over another in the non-RCT trials is not given.
- The environment, operator-related factors, and equipment are different in a pre-hospital vs. ED setting. Combining these two into one meta-analysis doesn’t make sense.
- Included studies were further limited by selection bias, small sample sizes, lack of blinding, and reporting bias.
- All included studies were from the USA, which limits the external validity.
- Included studies assessed patients in the emergency department and prehospital setting, which limits the external validity to other treatment areas such as the ICU.
Discussion:
Inside the Numbers:
- Investigators found a statistically significant decrease in risk of post-induction hypotension with etomidate vs. ketamine (OR: 0.53, 95% CI: 0.31 – 0.91; p = 0.02). Based on the data, patients receiving etomidate were half as likely to experience post-induction hypotension. However, the meta-analysis included only 2 RCTs. In an unblinded, nonrandomized cohort study, it’s possible one agent was used in a sicker cohort compared to another, thereby biasing the results.
- In fact, trials representing 2/3rds of the weight of the meta-analysis are biased to favor etomidate. April 2020 NEAR registry study represents 1/3rd the weight of this meta-analysis. The groups were unbalanced, with more patients with sepsis and more patients with difficult airway characteristics in the ketamine group.
- Pollack 2020 retrospective observational trial was 38% of the weight of this review. 2/3rds of the population were trauma patients, and more patients in the ketamine arm had shock, hypoxemia, extremes of size, and anatomic challenges, potentially biasing the results to favor etomidate.
- Lastly, it’s unclear whether the first-pass success rate has anything to do with the agent used.
Heterogeneity:
- In addition to the significant flaws mentioned above, the included trial had a great deal of heterogeneity. Test of heterogeneity (I2) allows us to determine the consistency of results across all included studies in a meta-analysis. If there is a significant amount of variation in the study results, we may be uncomfortable combining the results of multiple studies to obtain a single pooled summary effect. When I2 is above 50%, there is concern that studies have too much variability to pool the results. In addition, a low P value (for I2) < 0.05 raises concern that differences are less likely due to chance. I2 = 68% and P = 0.008 for post-induction hypotension in this paper. Indicating a high degree of heterogeneity with a low likelihood that differences are due to chance.
REBEL Rant:
- Induction agent selection is nuanced, with many factors to consider. It seems near impossible for one medication to outperform another for all patients when considering the innumerable potential diseases which may eventually lead to intubation. Furthermore, it’s undeniable that intubating a patient with an undifferentiated disease is remarkably different than intubating in the ICU with a full panel of diagnostics to reflect upon. We accept that a single antibiotic will not eradicate all bacteria, yet we curiously continue to search for a single agent for RSI induction.
Authors Conclusions: “Findings from the meta-analysis suggest that the use of etomidate is associated with decreased risk of post-induction hypotension during RSI compared with ketamine, while the choice of induction agent has no effect on first-pass intubation success. ”
Our Conclusions:
The data presented adds to the growing body of literature about RSI induction. However, due to the lack of high-quality RCTs and the large impact and weighting of flawed studies included in the meta-analysis, we remain skeptical of the findings…The debate continues.
References:
- Albert SG, Ariyan S, Rather A. The effect of etomidate on adrenal function in critical illness: a systematic review. Intensive Care Med. 2011;37(6):901-910. PMID: 21373823
- Jabre P, Combes X, Lapostolle F, et al. Etomidate versus ketamine for rapid sequence intubation in acutely ill patients: a multicentre randomised controlled trial. Lancet. 2009;374(9686):293-300. PMID: 19573904
- Van Berkel MA, Exline MC, Cape KM, et al. Increased incidence of clinical hypotension with etomidate compared to ketamine for intubation in septic patients: A propensity matched analysis. J Crit Care. 2017;38:209-214. PMID: 27974285
- April MD, Arana A, Schauer SG, et al. Ketamine Versus Etomidate and Peri-intubation Hypotension: A National Emergency Airway Registry Study. Acad Emerg Med. 2020;27(11):1106-1115. PMID: 32592205
- Matchett G, Gasanova I, Riccio CA, et al. Etomidate versus ketamine for emergency endotracheal intubation: a randomized clinical trial. Intensive Care Med. 2022;48(1):78-91. PMID: 34904190
- Pollack MA, Fenati GM, Pennington TW, et al. The Use of Ketamine for Air Medical Rapid Sequence Intubation Was Not Associated With a Decrease in Hypotension or Cardiopulmonary Arrest. Air Med J. 2020;39(2):111-115. PMID: 32197687
Guest Post By:

Anthony Ascione, DO
PGY 3, Garnet Health Medical Center, Middletown, NY
Email: aascione@garnethealth.org
Thomas Liu, MS, DO, FACOEP
Core Faculty, Emergency Medicine Residency
Garnet Health Medical Center, Middletown, New York
Instagram: Middletowngem

Marco Propersi, DO, FAAEM
Vice-Chair, Emergency Medicine
Vassar Brothers Hospital, Poughkeepsie, New York
Twitter: @marco_propersi
Post-Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post Etomidate Vs. Ketamine: A Systematic Review and Meta-Analysis appeared first on REBEL EM - Emergency Medicine Blog.
