
 Background: Oxygen therapy is frequently used in the emergency department for the treatment of hypoxia and respiratory failure and can be delivered in a variety of ways. Conventional oxygen therapy (COT) via nasal cannula is often a first line treatment, but has some drawbacks, including inability to deliver a precise concentration and volume of oxygen, inability to deliver high enough concentration and volume of oxygen, inability to heat and humidify, and poor tolerance. While it is able to deliver more precise, high flow oxygen, noninvasive ventilation (NIV) also presents a comfort challenge for many patients. High flow nasal cannula (HFNC) has been introduced as an alternative to COT and NIV. It can be used to deliver heated, humidified oxygen at high rates (up to 60 L/min) and maintain a set oxygen fraction. Prior randomized controlled trials (RCTs) and meta-analysis comparing HFNC to COT and NIV have demonstrated conflicting results. Additionally, none of these previous meta-analyses have evaluated emergency department (ED) patients.
Background: Oxygen therapy is frequently used in the emergency department for the treatment of hypoxia and respiratory failure and can be delivered in a variety of ways. Conventional oxygen therapy (COT) via nasal cannula is often a first line treatment, but has some drawbacks, including inability to deliver a precise concentration and volume of oxygen, inability to deliver high enough concentration and volume of oxygen, inability to heat and humidify, and poor tolerance. While it is able to deliver more precise, high flow oxygen, noninvasive ventilation (NIV) also presents a comfort challenge for many patients. High flow nasal cannula (HFNC) has been introduced as an alternative to COT and NIV. It can be used to deliver heated, humidified oxygen at high rates (up to 60 L/min) and maintain a set oxygen fraction. Prior randomized controlled trials (RCTs) and meta-analysis comparing HFNC to COT and NIV have demonstrated conflicting results. Additionally, none of these previous meta-analyses have evaluated emergency department (ED) patients.
Article: Tinelli V et al. High Flow Nasal Cannula Oxygen Vs. Conventional Oxygen Therapy and Noninvasive Ventilation in Emergency Department Patients: A Systematic Review and Meta-Analysis. JEM 2019. PMID: 31421952
Clinical Question: In patients with acute respiratory failure in the ED, does conventional oxygen therapy vs high flow nasal cannula vs noninvasive ventilation reduce intubation requirements?
What They Did: A systematic review and meta-analysis of RCTs, comparing HFNC to COT and NIV for ED patients in acute respiratory failure (ARF).
Outcomes:
- Primary: Intubation requirement
-
Secondary:
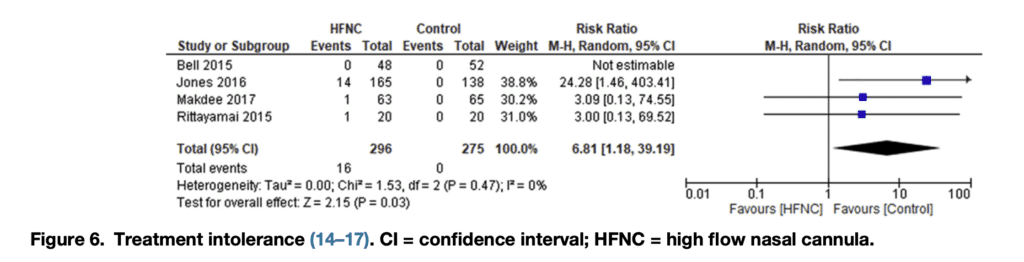
- Rate of treatment intolerance (i.e., interruption of treatment required by the patient for discomfort)
- Dyspnea improvement
- Treatment failure
- Hospitalization
- Longest follow-up all-cause mortality
Inclusion:
- Studies on adult patients with acute respiratory failure (Primary study author definitions) admitted and treated in the ED
- Investigating HFNC use vs COT or other modes of ventilation
- Presenting outcomes of interest
- Randomized controlled trials
Exclusion:
- Trials comparing HFNC vs oxygen or ventilation support outside the ED
- Studies published as a meeting abstract
- Nonrandomized studies
Results:
- 1287 articles identified in initial search, screening of titles and abstracts resulted in 26 articles for full-text assessment and five articles met inclusion criteria.
- Four articles compared HFNC to COT
- 296 HFNC patients
- 275 COT patients
- One article compared HFNC to NIV
- 104 HFNC patients
- 100 NIV patients
- Comparison of HFNC to COT – 4 studies
-
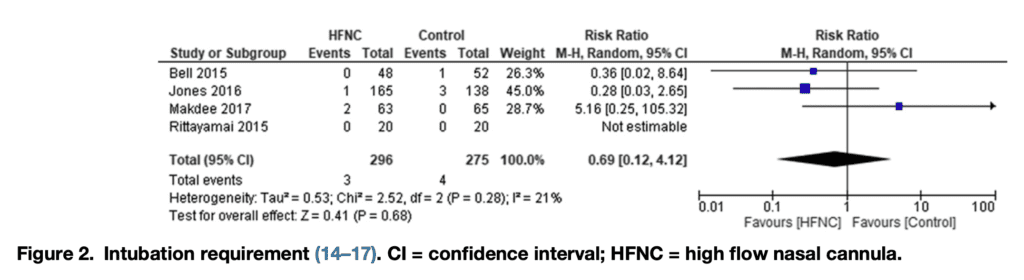
No differences in intubation requirements
- RR 0.69, 95% CI 0.12–4.12, p for effect = 0.68; p for heterogeneity = 0.28; I2 = 21%; with four included trials
-
No differences in intubation requirements
- Four articles compared HFNC to COT
-
-
-
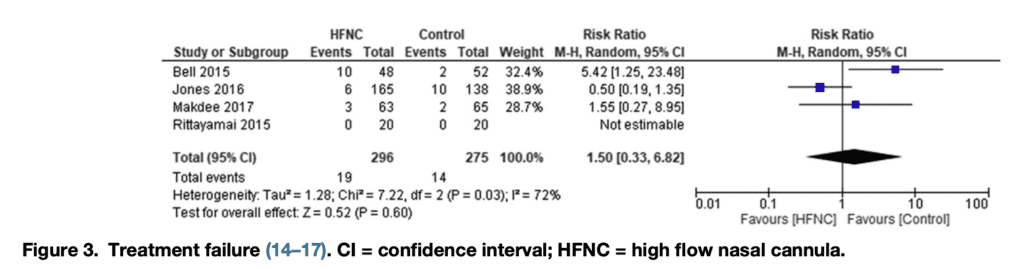
No differences in rate of treatment failure
- RR 1.49, 95% CI 0.33–6.82, p for effect = 0.60; p for heterogeneity = 0.03; I2 = 72%; with four included trials
-
No differences in rate of treatment failure
-
-
-
-
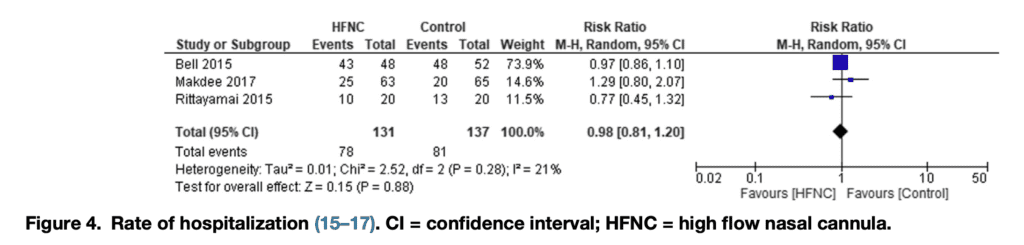
No differences in rate of hospitalization
- RR 0.99, 95% CI 0.81–1.19, p for effect = 0.88; p for heterogeneity = 0.28; I2 = 21%; with three included trials
-
No differences in rate of hospitalization
-
-
-
-
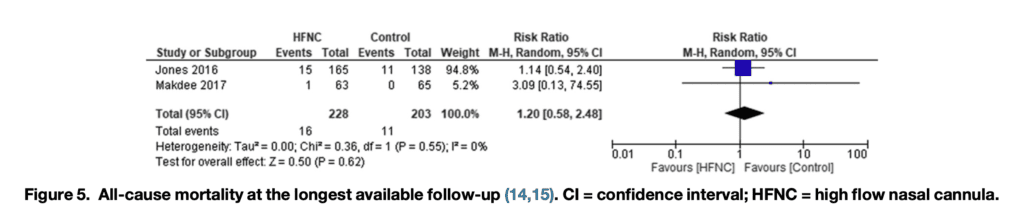
No differences in longest reported follow-up all-cause mortality
- RR 1.20, 95% CI 0.58–2.48, p for effect = 0.62; p for heterogeneity = 0.55; I2 = 0%; with two included trials
-
No differences in longest reported follow-up all-cause mortality
-
-
-
-
Significantly higher rate of treatment intolerance in HFNC group
- RR 6.81, 95% CI 1.18–39.19, p for effect = 0.03; p for heterogeneity = 0.47; I2 = 0%; with four included trials
-
Significantly higher rate of treatment intolerance in HFNC group
-
-
- Comparison of HFNC to NIV – 1 study
- No difference was found between HFNC and NIV in rates of intubation, treatment failure, vital signs, tolerance and dyspnea.
- Clinicians assigned better scores for respiratory response, patient comfort, and ease of the treatment to the HFNC group
- Comparison of HFNC to NIV – 1 study
Strengths:
- Asks a clinically important question
- Applied to ED specific population
- Has patient centered outcome measures (i.e. comfort)
- Performed a broad database search including PubMed/Medline, Embase, Cochrane Central Register of Controlled Trials database, and Google Scholar
- No language restrictions further including more studies
- Reference lists of all the selected studies, relevant reviews, and meta-analyses identified on the topic were also screened for additional RCTs
- All included trials had an assessment of the risk of bias using the Cochrane Collaboration’s Risk of Bias tool
- Used the I2 statistic, which describes the percentage of variation between studies that is due to heterogeneity
- 0% to 40% = might not be important
- 30% to 60% = may represent moderate heterogeneity
- 50% to 90% = may represent substantial heterogeneity
- 75% to 100% = considerable heterogeneity
- All data was evaluated with the intention-to-treat principle which is an unbiased approach to compare treatments groups as it avoids the effects of crossover, dropout, and is more like clinical practice
Limitations:
- Small number of included studies, all of which were quite small
- Etiology of respiratory failure was not specified, making it hard to determine which patients might benefit from which specific intervention. For example, COPD patients would benefit from NIV more than COT or HFNC. We just simply don’t know what types of acute respiratory failure patients we are treating in this meta-analysis
- Due to the obvious source of oxygen therapy, blinding of participants and personnel was not feasible. Although the authors do not feel this has a potential risk of bias, subjective outcomes can be biased by unblinding (i.e. performance bias). Criteria for respiratory failure and need for intubation are subjective and will vary from physician to physician
- There was poor blinding in terms of the outcome assessment (detection bias), and incomplete data (attrition bias) in many of the studies
Author Conclusion: “We did not find any benefit of HFNC compared with COT and NIV in terms of intubation requirement, treatment failure, hospitalization, and mortality; COT was better tolerated.”
Clinical Take Home Point: This meta-analysis does not answer the primary question of COT vs HFNC in acute respiratory failure in the ED, due to the small number of trials, the methodological issues mentioned above, and the heterogeneity in the causes of acute respiratory failure, which are not defined in the review. The best we can say, is use the oxygen delivery device that improves oxygen saturation, ventilation where needed, and most comfortable for the patient. This will most likely vary depending on the cause and severity of acute respiratory failure.
References:
- Tinelli V et al. High Flow Nasal Cannula Oxygen vs. Conventional Oxygen Therapy and Noninvasive Ventilation in Emergency Department Patients: A Systematic Review and Meta-Analysis. JEM 2019. PMID: 31421952
For More Thoughts on this Topic:
- Rebel EM – High Flow Nasal Cannula (HFNC) – Part 1: How It Works
- EMCrit – Podcast 152 – High Flow Nasal Cannulae – Just Blowin’ Hot Air?
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post Is All Oxygen Created Equal? appeared first on REBEL EM - Emergency Medicine Blog.
