
 This post is meant to accompany the REBEL Cast episode on The Crashing Asthmatic from June 2015. This blog post will also be simultaneously posted on the Core EM site here. Come over and check out our core content offerings. Thanks to the REBEL team for continuing to promote our site!
This post is meant to accompany the REBEL Cast episode on The Crashing Asthmatic from June 2015. This blog post will also be simultaneously posted on the Core EM site here. Come over and check out our core content offerings. Thanks to the REBEL team for continuing to promote our site!
Definition: An episode of wheezing, chest tightness or coughing resulting from variable airflow obstruction that is reversible. Underlying exacerbations are a chronic inflammatory disorder of the airways.
Management of Mild to Moderate Asthma Exacerbations
Epidemiology:
- 38.1 million Americans suffer from asthma
- 1.75 million ED visits/year
- 456,000 hospitalizations in the US (Akinbami 2011)
Pathophysiology:
- Stimuli (allergen and non-allergen) induce bronchoconstriction
- Bronchoconstricting stimuli result in edema, inflammation, airway smooth muscle hypertrophy and mucous production.
- Long-term permanent structural airway remodeling can develop
- Airway inflammation limiting airflow is the common final pathway
Symptoms: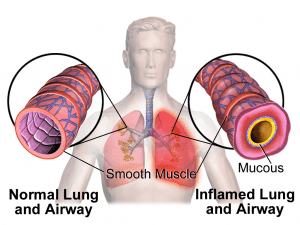
- Wheezing
- Cough
- Dyspnea
- Chest tightness
- Shortness of Breath
Physical Exam:
- Wheezing
- Tachypnea
- Tachycardia
- Retractions
- Use of accessory respiratory muscles
- Speaking in short sentences
Asthma Mimics: COPD exacerbations, Pulmonary edema, Anaphylaxis
Immediate Management:
Basics: ABCs with a focus on breathing. Supplementary O2 typically not needed in mild to moderate exacerbations.
Inhaled Beta2 Agonist (i.e. albuterol)
-
 Mechanism: Stimulate beta2 receptors in lungs leading to bronchodilation
Mechanism: Stimulate beta2 receptors in lungs leading to bronchodilation
- Nebulized albuterol solution
- Dose: 2.5 mg every 10-20 min
- Can be paired with an inhaled anticholinergic
-
Albuterol metered-dose inhaler (MDI) Equally effective to nebulized solution in mild exacerbations (Newman 2002, Cates 2013)
- Dose: 6-12 puffs every 10-20 min
- Side effects: tachycardia (beta1 stimulation), tremors, lactic acidosis (Lewis 2014)
Inhaled Anticholinergic (i.e. Ipratropium)
- Mechanism: Override smooth muscle constriction and secretory consequences of parasympathetic nervous system. Block reflex bronchoconstriction.
- Dose: 0.5 mg every 10-20 min (up to 3 doses)
- Impact: In combination with beta2 agonist, may avoid hospitalization in up to 1 in 11 treated patients (Plotnick 1998).
Systemic Corticosteroids
- Mechanism: Inhibit recruitment of inflammatory cells and mediators.
- Route: Evidence suggests that oral and intravenous corticosteroids are equally efficacious in patients with mild to moderate asthma exacerbations
-
Dose
- Prednisone: 1 mg/kg (typically up to 60 mg) PO
- Methylprednisolone sodium: 125 – 250 mg IV or IM
- Dexamethasone: 10-20 mg PO
- Impact: Numerous studies have shown reductions in admission rates as a result of systemic corticosteroid use in the ED (Rowe 1992). The majority of patients presenting to an ED for asthma exacerbation should receive systemic steroids.
Magnesium
- Mechanism: Bronchial smooth muscle relaxation
- Dose: 1-2 g over 30-60 min
- Impact: Modest decrease in hospital admission rate in patients refractory to standard management (Levy 2014)
- Reserved for moderate to severe exacerbations
Special Populations: Pregnancy
- Acute asthma exacerbations should be treated the same in pregnant patients as in nonpregnant patients.
- Fetal monitoring should be considered for patients with moderate to severe exacerbations in the 3rd trimester.
Diagnostics:
Asthma is a clinical diagnosis and patients with mild to moderate exacerbations rarely need any testing in the ED. Diagnostic tests may be useful in patients with asthma that is refractory to standard management as detailed above or if an alternate cause of symptoms is suspected.
Pulmonary Function Tests (PFTs)
- Measure forced expiratory volume in 1 second (FEV1) or peak expiratory flow rate (PEFR)
- Most helpful when patient knows their baseline performance
Chest Radiography
- The majority of patients with asthma exacerbations that are typical for them DO NOT need a chest X-ray performed.
- Consider X-ray in patients with more severe symptoms or those that do not resolve with standard treatment.
Lab Studies
- Rarely useful in mild to moderate (or even in severe) asthma exacerbations.
- Leukocytosis common as a result both of stress as well as steroid use
- Arterial Blood Gas
- Do not correlate with clinical outcomes
- Critical ABG data points (O2, CO2) can be obtained by other means (Pulse oximetry for O2, VBG for CO2)
Disposition
- Relapse after ED visits is common (up to 11% at 3 days) (Rosen’s 2014)
- Admission
- Incomplete response based on overall clinical picture or PFTs (< 70% improvement)
- Significant comorbidities
-
Discharge
- Airway inflammation continues after discharge and can take days to improve
- Medications
- Beta agonist inhaler (and demonstration of proper use). Consider giving all patients a spacer device as this improves drug delivery and thus efficacy.
- Steroids
- Short burst steroid treatment with prednisone for 5 days (no taper needed)
- Dexamethasone – 2 doses on days 1 and 2 shown to be non-inferior to 5 days of prednisone in one small study (Kravitz 2011)
- Short burst steroid treatment with prednisone for 5 days (no taper needed)
- Steroids
- Beta agonist inhaler (and demonstration of proper use). Consider giving all patients a spacer device as this improves drug delivery and thus efficacy.
- Follow-up
- Patients should contact their physician in 3-5 days and have follow-up arranged in 1-2 weeks
- Consider referral to an asthma specialist in patients with frequent exacerbations, frequent ED visits or frequent rescue inhaler use.
Take Home Points
- First line treatment for asthma exacerbations is inhaled beta agonists, inhaled anticholinergics and systemic corticosteroids.
- The majority of patients presenting to the ED with asthma exacerbations should be started on short-burst corticosteroids to control inflammation and prevent admission and relapse.
- Diagnostic testing is not required for the majority of patients with asthma exacerbations.
References:
- Nowak RM, Tokarski GF: Asthma in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 8. St. Louis, Mosby, Inc., 2014, (Ch) 73: p 941-58
- Akinbami LJ et al. Asthma prevalence, health care use, and mortality: United States, 2005-2009. Natl Health Stat Report 2011; 32:1-14. Link
- Newman KB et al. A comparison of albuterol administered by metered-dose inhaler and spacer with albuterol by nebulizer in adults presenting to an urban emergency department with acute asthma. Chest 2002; 121: 1036-41. PMID: 11948030
- Cates CJ et al. Holding chambers (spacers) versus nebulisers for beta-agnonist treatment of acute asthma (Review). Cochrane Database Syst Rev 2013. PMID: 24037768
- Lewis LM et al. Albuterol administration is commonly associated with increases in serum lactate in patients with asthma treated for acute exacerbations of asthma. Chest 2014; 145(1): 53-9. PMID: 23949578
- Plotnick LH, Ducharme FM. Should inhaled anticholinergic be added to B2 agonists for treating acute childhood and adolescent asthma? A systematic review. BMJ 1998; 317: 971-7. PMID: 9765164
- Rowe BH et al. Effectiveness of steroid therapy in acute exacerbations of asthma: a meta-analysis. Am J Emerg Med 1992; 10: 301-10 PMID: 1535500
- Levy Z, Slesinger TL. Does intravenous magnesium reduce the need for hospital admission among adult patients with acute asthma exacerbations. Ann Emerg Med 2014. PMID: 25128007
- Kravitz J et al. Two days of dexamethasone versus 5 days of prednisone in the treatment of acute asthma: a randomized controlled trial. Ann Emerg Med 2011; 58: 200-4. PMID: 21334098
Post Peer Reviewed By: Salim Rezaie (Twitter: @srrezaie)
The post Management of Mild to Moderate Asthma Exacerbations appeared first on REBEL EM - Emergency Medicine Blog.
