

Background: The geriatric patient population is at high risk for undertreatment of pain (Hwang et al. 2010). Regrettably, they are less likely to receive pain medication and commonly experience longer delays in treatment (Hwang et al. 2010). Likewise, there are many important considerations when prescribing analgesics in this group. Factors such as concomitant anticoagulation use and a history of gastrointestinal bleeding are vital historical elements that would likely alter treatment. Furthermore, many emergency medicine clinicians are apprehensive about treating elderly patients with opiates out of fear of untoward side effects.
In 2010, the United States Food and Drug Administration (FDA) granted approval for intravenous (IV) acetaminophen as a pain management option. However, its use remained limited in emergency medicine due to exorbitant costs and stringent prescribing restrictions. A turning point occurred in 2016 when a generic formulation of IV acetaminophen became available, significantly reducing costs and potentially facilitating broader utilization in routine practice. Nevertheless, the comparative analgesic efficacy of IV acetaminophen versus opioids remains uncertain, warranting further investigation.
Article: Kolli S, Friedman BW, Latev A, et al. A Randomized Study of Intravenous Hydromorphone Versus Intravenous Acetaminophen for Older Adult Patients with Acute Severe Pain. Ann Emerg Med. 2022;80(5):432-439. PMID: 35965162
Clinical Question: In patients over 65, what is the effect of 1 gram of IV acetaminophen on the reduction of severe pain compared with 0.5mg IV hydromorphone?
What They Did:
- Double-blinded, parallel-group, randomized trial
- Performed in 2 urban EDs in the Bronx, New York.
- Drugs were mixed in 100 ml of normal saline and administered via a parenteral drip over 10 minutes, followed by a 2 ml NS push.
- Pain was measured on a verbal scale from 0 to 10 (10 being worst, 0 being no pain at all), and pain level was measured at baseline, 15, 30, 60, 90, and 120 minutes.
- Clinicaltrials.gov Registry number: NCT03521102
Population:
Inclusion:
- Patients ≥ 65 years of age experiencing acute pain defined as onset within 7 days of ED visit in whom the attending physician planned to treat with intravenous opioids.
Excluded:
- Patient use of opioids or tramadol within the last 7 days
- Use of acetaminophen or NSAIDs within the previous 8 hours
- Any prior adverse reaction to opioids or acetaminophen
- Any daily or frequently recurrent pain that lasted for 3 months or more
- Patients with dementia
- Patients with chronic liver or kidney disease
- Use of monoamine oxidase inhibitors
- Systolic blood pressure <100mmHg, HR<60bpm, O2 saturation <92% on room air
Intervention:
- Acetaminophen 1,000mg administered IV in a 100 mL bag of 0.9% saline
Comparator:
- Hydromorphone 0.5mg administered IV in a 100 mL bag of 0.9% saline
Outcomes:
Primary:
- Improvement in pain, measured on a 0 to 10 pain scale from baseline to 60 minutes later
Secondary:
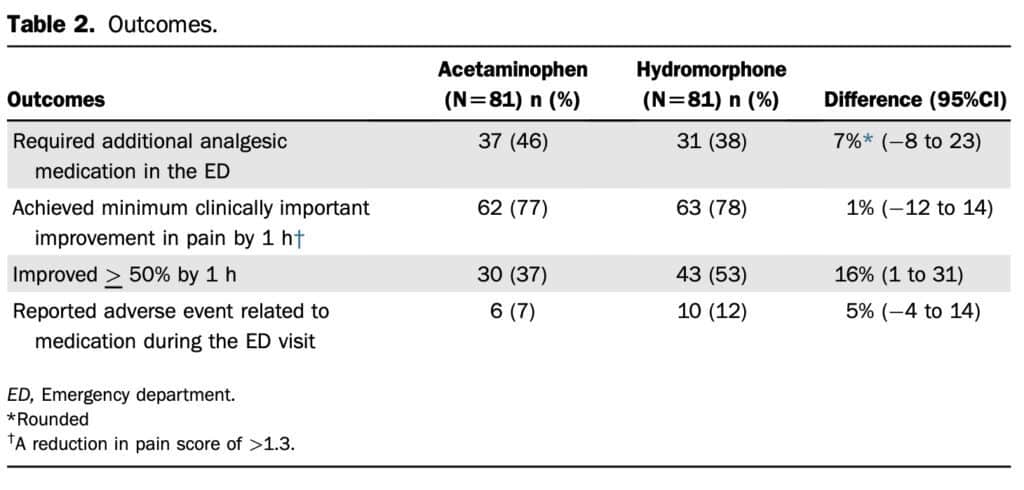
- Use of additional medication for the treatment of pain at any time during the ED course
- Percentage of patients who failed to achieve clinically important improvement in pain (<1.3)
- Percentage of patients who failed to achieve 50% improvement in their pain
- Absolute pain score at each time point
- Reported adverse event related to medication during the ED visit
Primary Results:
- 2 centers enrolled patients
- 2,363 patients were screened for participation though only 162 were enrolled
- Median Baseline pain rating 10/10
Critical Findings:
-
By 60 minutes:
- Patients receiving IV Acetaminophen improved by 3.6 (SD 2.9) on 0–10 pain scale
- Patients receiving IV Hydromorphone improved by 4.6 (SD 3.3) on 0–10 pain scale
- 95% CI for the difference of 1.0 was 0.1-2.0
Strengths:
- Investigators asked a patient-centered research question.
- Outcomes were patient-oriented
-
Double-blind, randomized trial design increases internal validity
- Patients, physicians, and outcome assessors were blinded to patient allocation
- Randomization occurred electronically by a random sequence generator
- Pharmacists prepared formulations away from the ED in a secure location, and clinical nurses retrieved them sequentially from a secure cabinet.
-
Medications were administered the same way—100 mL IV drip followed by 2 mL IV push.
- Medications appeared colorless and were indistinguishable to the eye
- Research staff was available 24 hours, 7 days a week
- Patients were analyzed in the group they were assigned
- Follow-up was complete
- The trial was registered, increasing transparency
Limitations:
- The study was performed within a single hospital system, limiting generalizability
- Patients were referred for inclusion by the attending physician which introduces selection bias.
- Investigators defined severe pain as an intention to use opiates which excludes patients to whom other meds were given, also introducing selection bias.
- The broad inclusion criteria lead to a heterogenous population which is difficult to compare.
- It is unclear how many patients were eligible for enrollment during the trial period but not enrolled.
- Investigators only studied one dose of each medication, and it is unclear how other doses would have performed.
-
There were important demographic considerations and patient population differences between the study’s two arms.
- Two-thirds of the population enrolled were women
- More 90-year-old patients were enrolled in the acetaminophen group.
- More patients with extremity pain were in the acetaminophen group.
- More patients with chest pain in the hydromorphone group.
Discussion:
- The study design necessitated a single parenteral dose of either hydromorphone or acetaminophen in each arm. Although 0.5 mg of IV hydromorphone is commonly considered the minimum dose for adult patients, it is crucial to recognize that various factors, most notably body weight, significantly influence the appropriate dosage of pain medications. It is reasonable to assume that a higher dose of hydromorphone would result in more pronounced analgesia, emphasizing the importance of individualized dosing strategies.
- Pain, an immensely diverse complaint with many causes, presents a substantial challenge. Beyond the patient’s age and location of pain, we know very little of the cause or prognosis in this paper. Moreover, we have insufficient knowledge regarding alternative interventions that could have alleviated pain. For instance, while pain resulting from extremity fractures and dislocations can often be relieved after reduction and splinting, abdominal pain poses a more elusive and complex scenario involving multiple contributing factors.
- Undoubtedly, some patients cannot tolerate oral medications and may benefit from parenteral administration. However, for individuals with a functional gastrointestinal tract, it remains unclear whether the intravenous formulation of acetaminophen offers any distinct advantages over its oral counterpart. Additionally, a recent systematic review encompassing six randomized controlled trials discovered no discernible difference in pain reduction between parenteral and oral formulations of acetaminophen when administered at equivalent doses (Jibril et al., 2015). Moreover, it is worth noting that even the now generic parenteral formulation of acetaminophen is considerably more expensive than its oral counterpart, raising questions about its cost-effectiveness and utility in practice.
Author’s Conclusions: “Although 0.5 mg of the intravenously administered hydromorphone was statistically superior to 1,000 mg of intravenous acetaminophen administered in older patients with acute severe pain in the ED, this difference was not clinically significant. Regardless of the medication received, many participants experienced minimal or incomplete pain relief.”
Our Conclusion:
We agree with the author’s conclusion. Investigators found no clinically significant differences in elderly patients with acute severe pain who received either 1,000 mg of IV acetaminophen or 0.5 mg IV hydromorphone. Nevertheless, it is imperative to acknowledge the intricate nature of pain, as a single dosage of any medication cannot be universally effective without considering the individualized aspects of each patient and the condition influencing their pain.
References:
- Montandon G. The pathophysiology of opioid-induced respiratory depression. Respiratory Neurobiology – Physiology and Clinical Disorders, Part I. Published online 2022:339-355. PMID: 35965031
- Acetaminophen. American Chemical Society. https://www.acs.org/molecule-of-the-week/archive/a/acetaminophen.html
- Hwang U, Richardson LD, Harris B, Morrison RS. The quality of emergency department pain care for older adult patients. Journal of the American Geriatrics Society. 2010;58(11):2122-2128. PMID: 21054293
- Platts-Mills TF, Esserman DA, Brown DL, Bortsov AV, Sloane PD, McLean SA. Older US emergency department patients are less likely to receive pain medication than younger patients: Results from a national survey. Annals of Emergency Medicine. 2012;60(2):199-206. PMID: 22032803
- Kolli S, Friedman BW, Latev A, et al. A randomized study of intravenous hydromorphone versus intravenous acetaminophen for older adult patients with acute severe pain. Annals of Emergency Medicine. 2022;80(5):432-439. PMID: 35965162
- Jibril F, Sharaby S, Mohamed A, Wilby KJ. Intravenous versus oral acetaminophen for pain: Systematic review of current evidence to support clinical decision-making. The Canadian Journal of Hospital Pharmacy. 2015;68(3). PMID: 26157186
Guest Post By:

Andrew Michalak, MD
PGY-1, Emergency Medicine Resident
Vassar Brothers Hospital, Poughkeepsie, New York
E-mail: Andrew.Michalak@nuvancehealth.org
Marco Propersi, DO FAAEM
Vice-Chair, Emergency Medicine
Assistant Emergency Medicine Program Director
Vassar Brothers Hospital, Poughkeepsie, New York
Twitter: @marco_propersi
Post-Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie), Anand Swaminathan, MD (Twitter: @EMSwami)
The post Managing Pain in the Elderly: Acetaminophen VS. Hydromorphone appeared first on REBEL EM - Emergency Medicine Blog.
