
 Orbital compartment syndrome (OCS) is a rare, vision-threatening diagnosis that requires rapid identification and immediate treatment for preservation of vision.1-4 As with other compartment syndromes, rapidly increasing and sustained high intraocular pressures (IOP) can result in devastating consequences. OCS causes retinal and optic nerve ischemia due to increased pressure on those structures. Due to the time-sensitive nature of this condition, the emergency physician (EP) plays a critical role in the diagnosis and management of OCS.5 The definitive therapy for this condition is lateral canthotomy and inferior cantholysis (LCIC).
Orbital compartment syndrome (OCS) is a rare, vision-threatening diagnosis that requires rapid identification and immediate treatment for preservation of vision.1-4 As with other compartment syndromes, rapidly increasing and sustained high intraocular pressures (IOP) can result in devastating consequences. OCS causes retinal and optic nerve ischemia due to increased pressure on those structures. Due to the time-sensitive nature of this condition, the emergency physician (EP) plays a critical role in the diagnosis and management of OCS.5 The definitive therapy for this condition is lateral canthotomy and inferior cantholysis (LCIC).
We covered the basics of OCS and LCIC in REBEL Core Cast Episode 42.0 (Link is HERE). In this post, we are going to cover some pearls and pitfalls for the emergency physician.
Pearls
Pearl #1: Be Prepared for OCS and LCIC
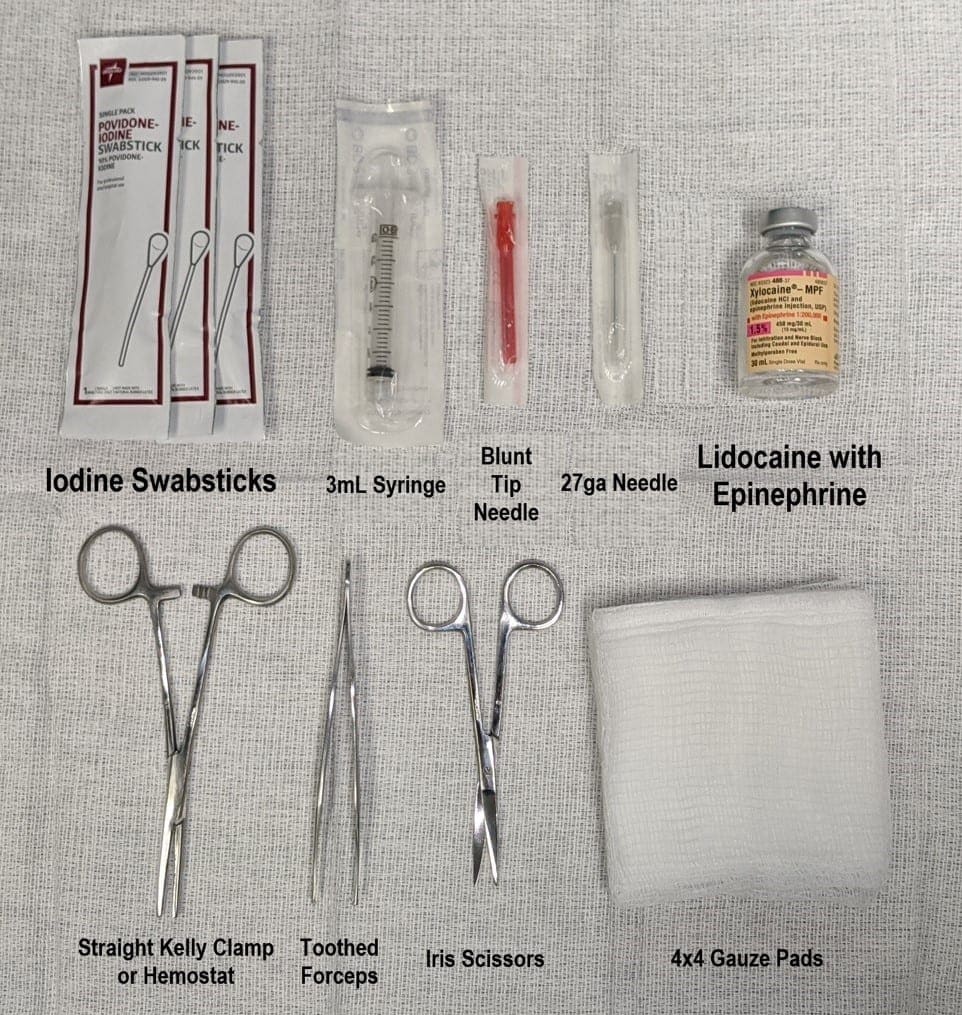
The time of diagnosis of OCS is not the time to be first learning the procedure, the necessary equipment, its indications and contraindications, and complications. A survey study suggested that over 90% of EPs felt inadequately trained in LCIC5. There are plenty of online resources that teach how to perform the procedure. Prepare yourself for the procedure by practicing on cadavers,6 animals,7 or low-fidelity simulation models.8 It can also be beneficial to create a kit with the necessary equipment for rapid access to the appropriate tools.
Pearl #2: Consult ophthalmology early
In all cases of OCS or suspected OCS, early consultation to ophthalmology is essential. It can be helpful to discuss the patient’s condition and potential management strategies with the eye experts. Furthermore, LCIC may incompletely relieve increased IOP, so the ophthalmologist may need to perform other procedures such as canthal cutdown, inferior orbital septal release, transcutaneous transseptal orbital decompression, or inferior anterior orbitotomy.9 Additionally, there may be associated injuries requiring ophthalmologist involvement such as hyphema, vitreous hemorrhage, or globe rupture.
Pearl #3: Take care to avoid iatrogenic injury during LCIC
Most patients with traumatic OCS have massive lid edema, ecchymosis, proptotic globes, and large subconjunctival hemorrhage, making LCIC a challenging procedure. Frequently, there is very little space to insert your instruments into the lateral canthus. Globe rupture is the most devastating complication of LCIC, but the procedure can also cause excessive bleeding, infection, damage to the lacrimal gland or artery, damage to the lateral rectus muscle, and ptosis from levator aponeurosis injury.10,11 Here are some ways to minimize complications:
- Consider procedural sedation, in addition to local intradermal (lidocaine with epinephrine) and topical ophthalmic anesthesia (proparacaine or tetracaine drops)
- Use a Morgan Lens as a shield to protect the globe; insertion can be challenging in patients with significant edema and ecchymosis
- When performing lateral canthotomy, point the instruments away from the eye laterally, aiming toward the lateral orbital rim
- When performing inferior cantholysis, use forceps to lift the inferior eyelid medially and anteriorly to tighten the inferior crus of the lateral canthal tendon
- After the first cut, bleeding may obscure your visual landmarks; attempt to “strum” the inferior canthal tendon with your scissors to identify the specific structure if you are unable to see it
- Aseptic technique is crucial, but you can also use empiric systemic antibiotics to prevent infections
Pitfalls
Pitfall #1: Failure to make OCS diagnosis and appropriately perform orbital decompression
Have a high level of suspicion for OCS in any patient with facial trauma or recent orbital surgery. Vision loss may be a late sign, so perform a thorough eye exam and measure the IOP early. IOP greater than 30mmHg necessitates a call to the ophthalmologist, while IOP greater than 40mmHg should be treated immediately with LCIC. Erickson et al. suggest a three-part decision tool to predict the need for LCIC: relative proptosis, “tight” eyelids that are difficult to open with finger pressure, and presence of a relative afferent pupillary defect in the traumatized eye.12
Pitfall #2: Delaying definitive surgical treatment for any reason
Delays in treatment of OCS are likely to result in permanent vision loss, so LCIC should be performed as soon as possible. None of the following should delay the procedure:
- Discussion with the ophthalmologist
- Discussion with the patient’s healthcare decision-maker (if the patient can participate in his or her own care, then it may be appropriate to explain the procedure quickly to get verbal consent)
- CT scans
- Ultrasound imaging: even though POCUS can be very fast, it does not add much to your current clinical picture and will likely not change your management
- Worsening visual acuity (a late sign of OCS and may be found in less than half of OCS cases13)
Delayed presentation shouldn’t prevent the EP from performing the procedure either. Dixon et al. found that 73% of OCS cases had return to baseline vision even with LCIC delayed beyond one hour after arrival.14 There are reports of vision recovery after delayed decompression, even up to 5 days!15
Pitfall #3: Failure to decrease IOP
Measure the IOP immediately after performing LCIC. The procedure does not always adequately decrease IOP, and if it is still elevated, then superior cantholysis can be performed. Take caution with this procedure because of the associated increased risk of globe rupture and lacrimal gland and artery injury. Medical management, although not very effective, can also be considered: mannitol, acetazolamide, high-dose methylprednisolone). 10,16 Despite these interventions, if the IOP is still elevated, the patient will need further surgical procedures performed by the ophthalmologist in the operating room (see Pearl #2 above).
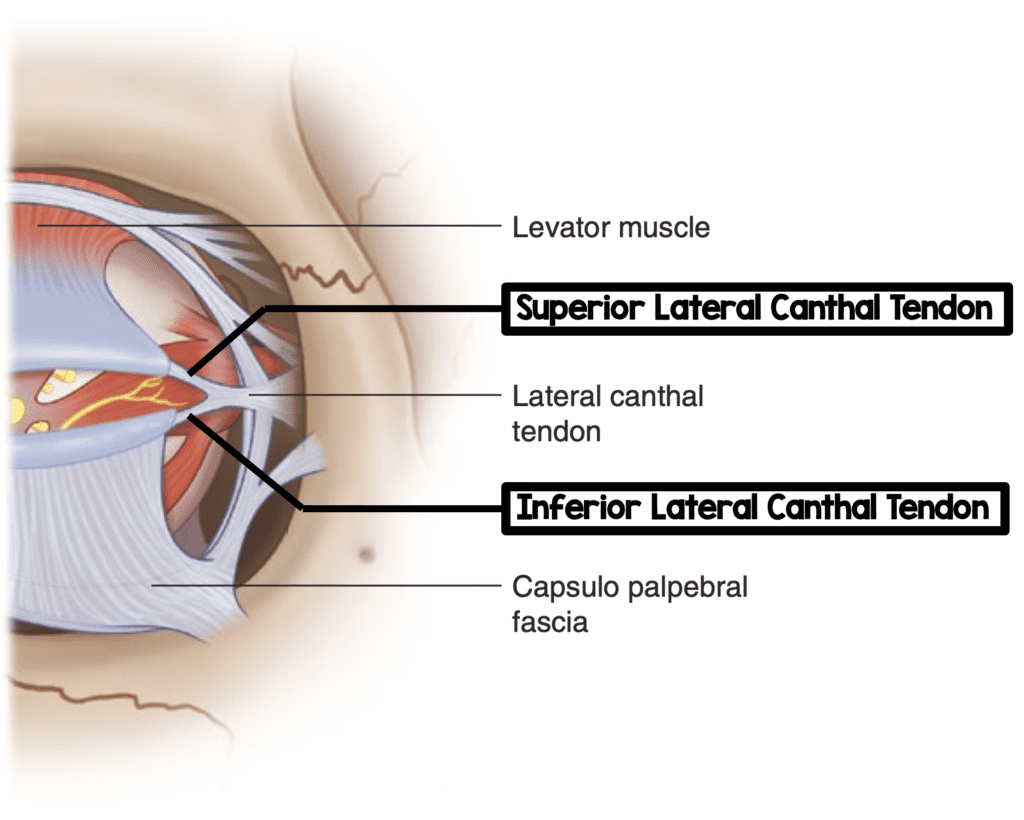
Components of the Lateral Canthal Tendon (Image modified from HERE)
Take-Home Points
- Orbital compartment syndrome is a vision-threatening condition that requires prompt recognition and emergent decompression with lateral canthotomy and inferior cantholysis
- Be prepared for the procedure by learning the steps, practicing it, and having the equipment ready
- Consult ophthalmology early so the patient can receive appropriate follow up in the hospital or other procedures in the OR
- Use some of the techniques listed above to prevent complications of LCIC
- Have a high level of suspicion for OCS and diagnose it early
- Don’t delay surgical treatment for any reason
- Measure the IOP immediately after LCIC and perform additional procedures as necessary
Here is a two minute video from our friends at EM:RAP going through the procedure
References:
- Larsen M et al. Acute orbital compartment syndrome after lateral blow-out fracture effectively relieved by lateral cantholysis. Acta Ophthalmol Scand 1999. PMID: 10321547.
- Popat H et al. Blindness following retrobulbar haemorrhage—it can be prevented. Br J Oral Maxillofac Surg 2007. PMID: 16099557
- Whitford R et al. Out-of-hospital lateral canthotomy and cantholysis: a case series and screening tool for identification of orbital compartment syndrome. Air Med J 2018. PMID: 29332783
- Li KK et al. Orbital compartment syndrome following orthognathic surgery. J Oral Maxillofac Surg 1995. PMID: 7629632
- Edmunds MR et al. Management of acute retrobulbar haemorrhage: a survey of non-ophthalmic emergency department physicians. Emerg Med J 2019. PMID: 30630842
- Patel SR et al. A human cadaveric model for effective instruction of lateral canthotomy and cantholysis. Orbit 2020. PMID: 31106640
- Suner S et al. A porcine model for instruction of lateral canthotomy. Acad Emerg Med 2000. PMID: 10917338
- Kong R et al. A low fidelity eye model for lateral canthotomy training. Afr J Emerg Med 2018. PMID: 30456160
- Lima V et al. Orbital compartment syndrome: the ophthalmic surgical emergency. Surv Ophthalmol 2009. PMID: 19539832
- Iserson KV et al. Orbital Compartment Syndrome: Alternative Tools to Perform a Lateral Canthotomy and Cantholysis. Wilderness Environ Med 2016. PMID: 26585073
- Shek KC et al. Acute retrobulbar haemorrhage: an ophthalmic emergency. Emerg Med Australas 2006. PMID: 16712542
- Erickson BP et al. Evidence-based algorithm for the management of acute traumatic retrobulbar haemorrhage [published online ahead of print, 2020 Jun 13]. Br J Oral Maxillofac Surg 2020. PMID: 32546417
- Christie B et al. Retrobulbar hematoma: A systematic review of factors related to outcomes. J Plast Reconstr Aesthet Surg 2018. PMID: 29239798
- Dixon JL et al. Visual outcomes after traumatic retrobulbar hemorrhage are not related to time or intraocular pressure [published online ahead of print, 2019 Nov 18]. Am J Emerg Med 2019. PMID: 31784392
- Mellington FE et al. Orbital compressed air and petroleum injury mimicking necrotizing fasciitis. J Emerg Med 2014. PMID: 24915744
- McAllister AS. A clinical review of orbital anatomy and its relevance to retrobulbar anesthesia. Cureus 2013. [Link to paper]
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post Orbital Compartment Syndrome: Pearls and Pitfalls for the ED Physician appeared first on REBEL EM - Emergency Medicine Blog.
