
Background: Pneumothorax management is a common clinical condition in the emergency department (ED) occurring in patients of varying ages and caused by multiple etiologies, including spontaneous, traumatic, and iatrogenic pneumothorax. Regardless of the cause, a thoracostomy is often required for treatment (Currie 2007). Traditionally, all pneumothoraces were treated with large bore chest tubes (LBCT) defined as any tube > 14 F. The benefits of a small bore catheter (ie a pigtail catheter (PC) include less trauma to the chest wall and less patient pain. Additionally, small-bore catheter placement is performed via the Seldinger technique;’ a skill possessed by all Emergency Physicians (Bauman 2018). The decision to use a LBCT vs. a PC in the treatment of pneumothorax has been widely studied over the last decade, yet clinical practice still varies.
Article: Chang, Su-Huan et al. “A Systematic Review and Meta-Analysis Comparing Pigtail Catheter and Chest Tube as the Initial Treatment for Pneumothorax.” Chest vol. 153,5 (2018): 1201-1212. PMID: 29452099 Prospero: CRD42017078481
Clinical Question: Is a pigtail catheter (PC) more effective than a large bore chest tube (LBCT) for treating pneumothorax?
What They Did
- Systematic review and meta-analysis using multiple databases: PubMed, Embase, and Cochrane Library.
- Searched for randomized control trials and cohort studies published up to October 9, 2017, using search terms: pneumothorax, pneumothoraces, thoracentesis, drainage catheter, pigtail catheter, chest tube, and thoracostomy.
Population
Inclusion Criteria
- RCTs or cohort studies (prospective or retrospective)
- Articles that reported outcomes including success rate, recurrence rate, complication rates, hospital stay or prognosis in patients with pneumothorax
- Articles that included both small bore PC and LBCT drainage for initial pneumothorax treatment
Exclusion Criteria
- Pneumothorax in neonates
- Articles that only reported PC drainage OR LBCT drainage
Intervention
- Pigtail catheter
Comparator
- Chest tube
Outcomes
Primary Outcome
- Success rate for PC and LBCT for all types of pneumothorax
- Recurrence rate of pneumothorax
Secondary Outcomes
- Complication rates
- Drainage duration
- Hospital stay
Results
- 604 studies identified
-
489 were screened after duplicated records were removed
- 457 articles were deemed ineligible
- 32 full-text articles were reviewed
-
11 articles were deemed eligible and included in the study.
- 875 patients from Africa, Asia, Europe, and North America
- RCTs or retrospective cohort studies
Strengths
- Researchers followed PRISMA guidelines.
- They performed a comprehensive search of multiple large databases.
- Researchers used multiple reviewers to assess the eligibility of included studies and used arbitrators to settle disputes.
- The meta-analysis includes a large number of patients and increases external validity.
- Included studies were conducted on four continents, increasing external validity.
- Two bias tools (Newcastle-Ottawa and Cochrane) were used to evaluate for bias in cohort trials and RCTs.
- Heterogeneity was 0% for the primary outcome, and overall heterogeneity was low for secondary outcomes, which increases external validity.
- Investigators assessed publication bias depicted as a funnel plot.
Limitations
- There is no mention of whether authors checked reference lists of articles or searched for registered but unpublished trials.
- Did not quantitatively report on agreement among reviewers.
- While investigators used two tools to assess for bias in cohort studies and RCTs, they did not explicitly describe bias in each included study.
- There is no clear definition of “success” or “complication” for either PC or LBCT application.
- While clinically relevant and heavily debated, the primary outcome is disease-oriented and not patient-oriented.
- Researchers included all types of pneumothoraces in the study, which assumes the pathophysiology and treatment are the same for all pneumothoraces.
- Only 2 of 11 papers in the meta-analysis were RCTs—62 patients.
- The other nine included papers were retrospective cohort studies—813 patients.
- Due to the nature of the intervention, patients and physicians were likely not blinded.
- Many subgroups represent data heavily weighted with retrospective cohort studies and relatively few events from spontaneous pneumothorax papers.
- The funnel plot is based on a small number of studies. Fewer studies decrease the confidence we have in the data.
Discussion
Inside The Numbers
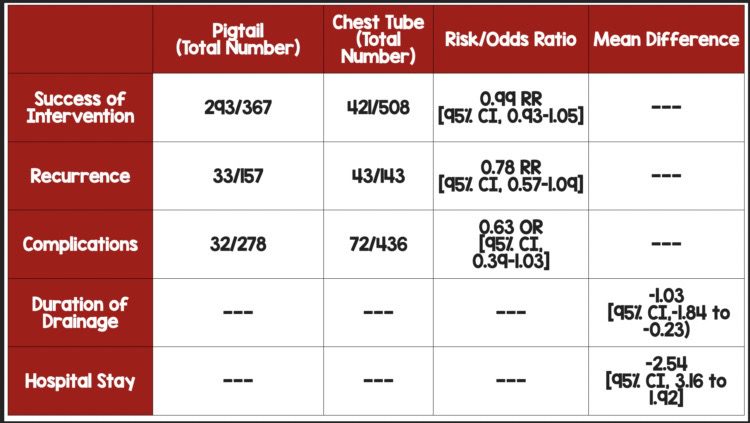
- Success Rates: There was no difference in PC and LBCT in success rate for the treatment of pneumothorax (RR, 0.99 [95% CI, 0.93–1.05]). Heterogeneity (I2) was 0%, indicating that variability was low and we should feel comfortable pooling the data from multiple studies.
- Complication Rates: Patients treated with PC were approximately ⅔ as likely to have a procedure-related complication compared to LBCT (Peto OR, 0.63 [95% CI, 0. 39-1.03]; I2 26%). The number needed to treat (NNT) using PC vs. LBCT is 20. Therefore, one complication may be avoided for every 20 patients treated with PC rather than LBCT. However, 77.2% of the weighting came from studies on spontaneous pneumothorax, which included just 1 RCT of 22 patients. Finally, the wide confidence intervals cross 1, adding uncertainty about whether the PC truly confers any benefit over LBCT concerning complication rates.
- The weighting of Trials: Investigators found a significantly shorter length of stay in the PC group compared to LBCT (MD, -2.54 [95% CI, -3.16 to -1.92]; P < .001; I 0%) and significantly shorter drainage duration in PC compared to LBCT (MD, -1.03 [95% CI, -1.84 to -0.23]; P= .01; I2 =51%). However, the secondary outcomes were heavily driven by the data from trials on spontaneous pneumothorax. The weighting from spontaneous pneumothorax was nearly 55% for drainage duration, 77% for complication rates, 96% for hospital length of stay, and 100% for recurrence rates.
Air is Air?
- Investigators assume that pneumothorax is a homogeneous disease process. Since air resistance is negligible, smaller tube diameters should be sufficient to evacuate all potential pneumothoraces. However, this assumption does not account for accumulation rates. Does an iatrogenic pneumothorax from a lung biopsy accumulate at the same rate as an iatrogenic pneumothorax from subclavian central venous access? Compared to a broken rib, how about a traumatic pneumothorax from a stab wound? While spontaneous pneumothorax may be a homogenous disease process, etiology likely plays a critical role in the pathophysiology of other types of pneumothorax.
Advantages of Pigtail Catheter
- More recent trials found that patients with traumatic pneumothorax and hemothorax managed with PC compared to LBCT experienced less pain (Kulvatunyou 2021, Kulvatunyou 2014).
- Pigtail catheters are placed via guidewire with seldinger technique which is strikingly similar to central venous access and may increase procedural competency.
- Similarly, pigtail catheter placement may be accessible to more clinicians, which is ultimately better for patient care, especially those at critical access hospitals.
Author’s Conclusions: “We found that for spontaneous pneumothorax, the drainage duration and hospital stay are shorter in the PC group. Furthermore, for secondary spontaneous pneumothorax, the complication rate is significantly lower in the PC group. Collectively, results of the meta-analysis suggest that PC drainage may be considered as the initial treatment option for patients with primary or secondary spontaneous pneumothorax.”
Our Conclusion:
We agree with the author’s conclusion. PC performed as well as LBCT in terms of successful drainage and was associated with fewer complications, decreased drainage duration, and decreased length of hospital stay, driven by data on spontaneous pneumothorax.
References:
- Bauman ZM, Kulvatunyou N, Joseph B, et al. A Prospective Study of 7-Year Experience Using Percutaneous 14-French Pigtail Catheters for Traumatic Hemothorax/Hemopneumothorax at a Level-1 Trauma Center: Size Still Does Not Matter. World J Surg. 2018;42(1):107-113. doi:10.1007/s00268-017-4168-3 PMID: 28795207.
- Currie GP, Alluri R, Christie GL, Legge JS. Pneumothorax: an update [published correction appears in Postgrad Med J. 2007 Nov;83(985):722]. Postgrad Med J. 2007;83(981):461-465. doi:10.1136/pgmj.2007.056978. PMID: 17621614.
- Kulvatunyou N, Erickson L, Vijayasekaran A, et al. Randomized clinical trial of pigtail catheter versus chest tube in injured patients with uncomplicated traumatic pneumothorax. Br J Surg. 2014;101(2):17-22. PMID: 24375295
- Kulvatunyou N, Bauman ZM, Zein Edine SB, et al. The small (14 Fr) percutaneous catheter (P-CAT) versus large (28-32 Fr) open chest tube for traumatic hemothorax: A multicenter randomized clinical trial. J Trauma Acute Care Surg. 2021;91(5):809-813. doi:10.1097/TA.0000000000003180. PMID: 33843831.
Guest Post By:

Jessica DiPeri, MD
PGY-3, Chief Emergency Medicine Resident
Saint Joseph’s University Medical Center, Paterson, New Jersey
Email: jtilzer12@gmail.com

Marco Propersi, DO FAAEM
Vice-Chair, Emergency Medicine
Vassar Brothers Hospital, Poughkeepsie, New York
Twitter: @marco_propersi
Post-Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami) and Salim R. Rezaie, MD (Twitter: @srrezaie)
The post Pigtail Catheter vs Large Bore Chest Tube for Pneumothorax appeared first on REBEL EM - Emergency Medicine Blog.
