 Background: Syncope, the sudden, brief loss of consciousness followed by spontaneous, complete recovery is a common presentation to the Emergency Department (ED). It represents a significant portion of overall admissions to the hospital because while many cases are benign (i.e. vasovagal syncope), some may result from a life-threatening cause (ventricular tachydysrhythmia, myocardial ischemia, gastrointestinal bleeding etc). Admission or 24 hour observation is often sought for continuous dysrhythmia monitoring but they are infrequently found. A decision instrument directed at stratifying patients to high or low risk for a dysrhythmia causing syncope (and thus subsequent risk for a recurrent dysrhythmia) would be useful in managing patients with syncope.
Background: Syncope, the sudden, brief loss of consciousness followed by spontaneous, complete recovery is a common presentation to the Emergency Department (ED). It represents a significant portion of overall admissions to the hospital because while many cases are benign (i.e. vasovagal syncope), some may result from a life-threatening cause (ventricular tachydysrhythmia, myocardial ischemia, gastrointestinal bleeding etc). Admission or 24 hour observation is often sought for continuous dysrhythmia monitoring but they are infrequently found. A decision instrument directed at stratifying patients to high or low risk for a dysrhythmia causing syncope (and thus subsequent risk for a recurrent dysrhythmia) would be useful in managing patients with syncope.
Article: Thiruganasambandamoorthy V et al. Predicting short-term risk of arrhythmia among patients with syncope: the Canadian syncope arrhythmia risk score. Acad Emerg Med 2017. PMID: 28791782
Clinical Question: Can a decision instrument be developed for predicting the 30-day risk of dysrhythmia or death after ED presentation for syncope?
Population: Patients > 16 years of age who presented with syncope within 24 hours of the event. Syncope defined as a brief loss of consciousness (< 5 minutes)
Outcomes:
Primary: Death or dysrhythmia (including procedural interventions for dysrhythmia) within 30 days.
Design: Multicenter prospective cohort study
Excluded: Prolonged loss of consciousness (> 5 minutes), change in mental status after syncope, witnessed seizure, head trauma causing loss of consciousness, patients unable to provide proper history due to alcohol or drug intoxication or patients with a language barrier.
Primary Results:
- Enrolled patients: 5,358
- Incomplete outcomes assessment: 348/5358 (6.5%)
-
Inter-rater reliability assessment
- 207 patients (4.1%)
- Kappa = 0.89 (95% CI: 0.79-0.98)
- Admission rate: 9.5%
-
Comorbid Conditions
- Hypertension (31.6%)
- Diabetes (10.0%)
- CAD (11.6%)
- Congestive Heart Failure (3.6%)
Critical Findings:
-
Primary outcome at 30-days (death or dysrhythmia)
- 2.1% (106/5010) 95% CI 1.7 – 2.5%)
- 0.9% (45/5010) suffered primary outcome after discharge from the hospital
- 0.57% (29/5010) had pacemaker placement performed
-
Decision tool derivation
- Researchers identified 39 candidate predictors
-
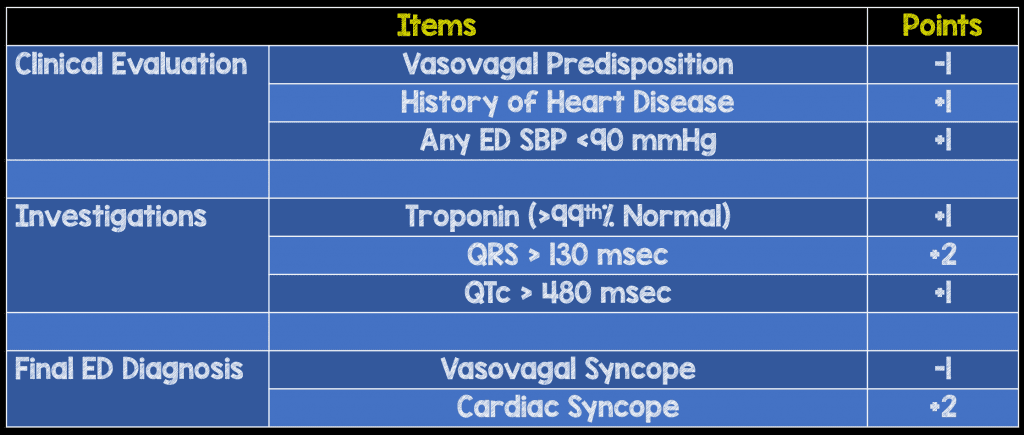
Final model with eight predictors
- Three clinical evaluation predictors, three investigation predictors and two final ED diagnoses
- Vasovagal predisposition (warm-crowded place, prolonged standing, fear, emotion or pain)
-
Decision tool score
- Ranges from -2 to +8 (lower score = lower risk)
-
Threshold Scores
-
Score > 0
- Sensitivity: 97.1% (95% CI: 91.6 – 99.4%)
- Specificity: 53.4% (95% CI: 52.0 – 54.9%)
- (+) LR = 2.0
- (-) LR = 0.05
-
Score > 6
- Sensitivity: 9.8%
- Specificity: 99.6%
- (+) LR = 245
- (-) LR = 0.91
-
Score > 0
Strengths:
- Large, prospective study addressing an important clinical question that can potentially affect millions of patients
- First study of it’s kind to attempt to identify risk factors for short term development of dysrhythmia or death
- Primary outcome is patient centered
- Used the validated, European Society of Cardiology (ESC) guidelines for arriving at the final ED diagnosis
-
Researchers worked extensively to track down patients to gauge outcomes
- Structured review of all medical records related to index and subsequent ED visits, hospitalizations and hospital record deaths
- Scripted telephone follow-up at 30-days
- Reviewed health records at all local adult hospitals in Ontario and administrative health database (NetCare)
- Ontario coroner’s office records reviewed
Limitations:
- Although multi-center, was single system and single country
- Primary outcome was a composite where the outcomes weren’t of equivalent impact on the patient (death and dysrhythmia)
- Requires external validation that includes sites in various countries prior to implementation
- 20% of eligible patients were not enrolled in the study
- Patients were overall young (mean age 53.4 years) and relatively healthy limiting application of the decision tool
- “Vasovagal Predisposition” is subjective and may be difficult to reliably gauge. This factor will require further study for inter-rater reliability
- Final diagnosis of vasovagal and cardiac syncope subjective (though inter-observer agreement in this study was high)
- Vasovagal predisposition and vasovagal syncope as the final diagnosis are likely interdependent factors and not independent items
- Incomplete data on parts of decision tool (i.e. only 54.2% of patients had troponin performed)
- Troponin assays were different at different institutions and difficult to compare directly
Authors Conclusions:
“The Canadian Syncope Arrhythmia Risk Score can improve patient safety by identification of those at-risk for arrhythmias and aid in acute management decisions. Once validated, the score can identify low-risk patients who will require no further investigations.”
Our Conclusions:
This prospectively derived decision instrument may be helpful in stratifying syncope patients to high or low risk for dysrhythmia but requires external validation prior to consideration for implementation.
Potential to Impact Current Practice:
Because dysrhythmia is a common reason for admission to hospital and further workup of patients presenting with syncope, this decision tool has the potential to be used to support a decision of discharge and follow up and avoid low yield inpatient evaluations if externally validated.
Clinical Bottom Line:
The prospective derivation of this decision instrument is a positive step towards risk stratification of syncope patients for subsequent dysrhythmias. It is critical to remember that there are numerous other causes of syncope (ectopic pregnancy, PE, ACS, aortic dissection, GI bleeding etc) that should be considered in patients as well. Additionally, because the population in this study was relatively young and healthy, evaluation of a higher risk cohort would be useful in future studies.
For More on This Topic Checkout:
- ALiEM: Management of Syncope
- Ryan Radecki at EM Lit of Note: Predicting Poor Outcomes After Syncope
Post Peer Reviewed By: Salim Rezaie (Twitter: @srrezaie)
The post Predicting Dysrhythmias After Syncope appeared first on REBEL EM - Emergency Medicine Blog.