
Background: In an older study published in Resuscitation 1998 [1], ED physicians, ICU physicians, and nurses tried to identify a carotid pulse in a healthy male volunteer with normal blood pressure. 43.1% of the health professionals required >5 seconds to detect the carotid pulse and another 4.3% required >10 seconds. Something I have advocated for in cardiac arrest is the death of pulse checks, as our fingers are poorly sensitive for detecting which patients have a pulse in a shock state. A visible rhythm on the monitor, along with the absence of a pulse with digital palpation, does not always indicate the presence of true pulseless electrical activity (PEA). Our reflexive action when we don’t feel a pulse is to begin CPR and give 1mg epinephrine which may not be beneficial in these patients. Patients in profound shock don’t necessarily need cpr and 1mg of epinephrine, they need augmentation of cardiac output with either push dose pressors or hemodynamically driven epinephrine drips. Now another study published in Resuscitation looked to compare the efficiency of cardiac ultrasonography (CUSG), doppler ultrasonography (DUSG) and manual pulse palpation to check the pulse in cardiac arrest patients [2].
What They Did:
- Single center, prospective observational study of 137 patients undergoing cardiopulmonary resuscitation (CPR)
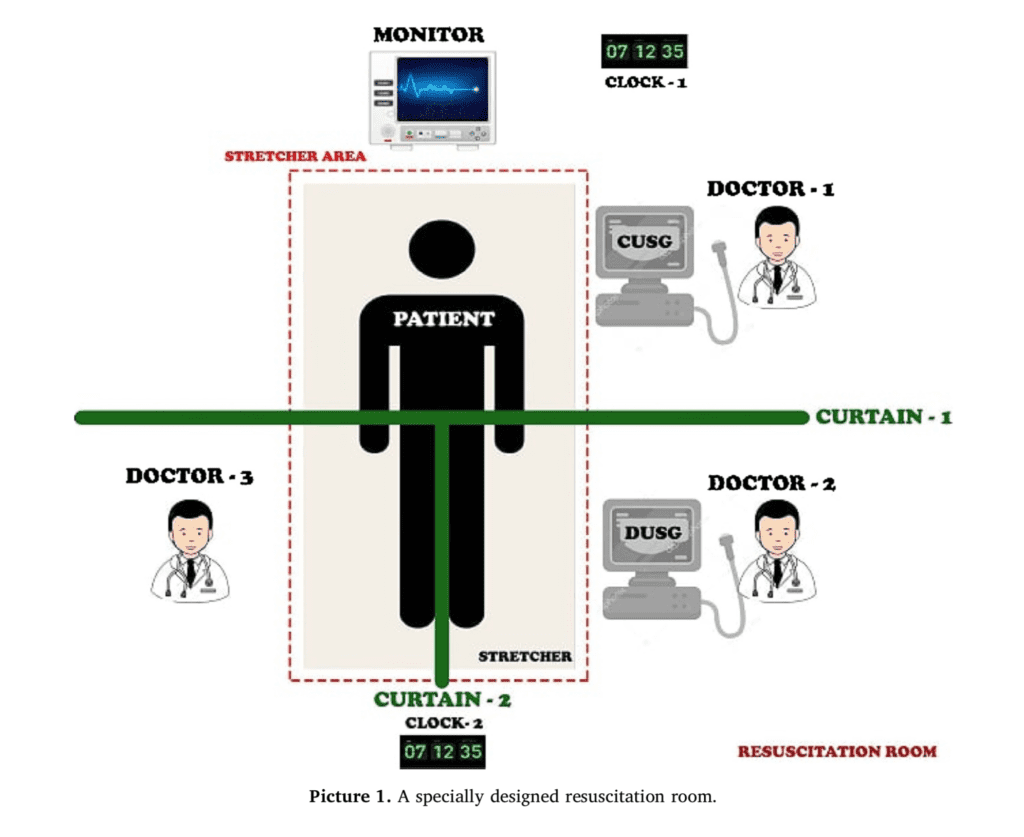
- CUSG, DUSG, and manual pulse palpation were done simultaneously and recorded at the first minute, 15 minutes, and termination of CPR
- CUSG was performed through a subxiphoid view, DUSG was performed through the left femoral artery
Outcomes:
- Efficiency of CUSG vs DUSG vs manual pulse palpation in cardiac arrest patients
Inclusion:
- Age ≥16 years
- Cardiac arrest
- Physicians completing 16 hours of theoretical and applied focus ultrasound training and 8hr of basic cardiac ultrasonography
Exclusion:
- No ultrasonography performed
- Technical or anatomic difficulties
Results:
- 3% (n = 99) of CA incidents occurred out-of-hospital
- 2% (n = 125) of CA incidents were non-traumatic
- 2% (n = 29) of CA incidents achieved ROSC
- The overall average duration of CPR was 37.2 +/- 13.2 minutes, and in patients achieving ROSC was 22.9 +/- 17.1 minutes
- Duration of intervention: CUSG (≈4sec) < DUSG (≈8sec) < Manual palpation (≈10sec)
- 37 patients found to be in PEA on Initial Evaluation with Manual Pulse Palpation:
- CUSG = 18.9% did not have true PEA
- DUSG = 13.5% did not have true PEA; 1 out of 30 (3.3%) patients with true PEA falsely found to have a pulse
- Manual Pulse = 7 patients with pulse detected by manual palpation: 6 (85.7%) found to have asystole and 1 with VF on CUSG
- 29 patients found to be in PEA on 15-minute Evaluation with Manual Pulse Palpation:
- CUSG = 20.7% did not have true PEA
- DUSG = 13.8% did not have true PEA; Missed pulse in 1 pt with ROSC & falsely found 2 pts with pulse who were in true PEA
- Manual Pulse = 4 patients found to have a pulse with manual pulse palpation actually had asystole
- 4 patients found to be in PEA on Last Inspection with Manual Pulse Palpation:
- All 4 patients (100%) had true PEA
- DUSG had a false negative rate for pulse of 10.3% and false positive rate of 0.9%
- Manual palpation had a false negative and false positive rate of 0%
Strengths:
- Study done in real time and prospectively
- Special curtain system which came down from the ceiling and divided the body into three parts was used so evaluators were blinded to each other
- CUSG, DUSG, and manual pulse palpation was completed in maximum of 10seconds
- US images recorded for further evaluation
Limitations:
- Single center study
- Physicians completed 16 hours of theoretical and applied focus ultrasound training and 8hr of basic cardiac ultrasonography. These providers also had >1 year of experience with US in resuscitation and cardiac arrest. Many providers in community settings may not have this much training and can affect ultrasound interpretations
- Incomplete ultrasound results in some cases, which were excluded from the study
- Adjudication of cardiac ultrasonography not performed. There is poor inter-rater agreement about what cardiac standstill is and we have covered this before on REBEL EM
Discussion:
- In this current study all patients with no cardiac activity identified by CUSG died. No cardiac activity is a poor prognostic indicator, however from prior studies (i.e The REASON Trial) the accuracy of no cardiac activity predicting death is closer to 2 – 3%. Use of no cardiac activity should be taken in combination with other predictors of poor outcomes such as prolonged downtime, unwitnessed arrest, and EtCO2 <20mmHg when deciding to cease resuscitation efforts and not used alone.
- Interestingly in this study CUSG was performed in about 4 seconds. This may have been due to the training of the physicians prior to the study. Several studies in the past have shown that comfort with the ultrasound can decrease duration and this result should be taken with a grain of salt for providers who are not as well versed in ultrasound
Author Conclusion:“The use of real-time CUSG during resuscitation provides a substantial contribution to the resuscitation team. CUSG will allow earlier and more accurate detection of pulse than manual pulse palpation and DUSG.”
ClinicalTake Home Point: Manual pulse palpation alone can result in incorrect decisions in management of cardiac arrest patients and should stop being used in clinical practice as it is not sensitive or specific for pulses in cardiac arrest. DUSG is a nice secondary modality compared to CUSG but can have false positives and negatives for pulse detection. Some institutions have started using TEE, which would be the optimal tool for the job, however the majority of ED providers do not have access to TEE so it seems, in appropriately trained providers, CUSG > DUSG > Manual Palpation would be the preferred modalities, in descending order, for pulse detection in cardiac arrest.
References:
- Ochoa FG et al. Competence of Health Professionals to Check the Carotid Pulse. Resuscitation 1998. PMID: 9715777
- Zengin S et al. Comparison of Manual Pulse Palpation, Cardiac Ultrasonography and Doppler Ultrasonography to Check the Pulse in Cardiopulmonary Arrest Patients. Resus 2018. PMID: 30253230
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post Pulse Checks in Cardiac Arrest Should be Dead appeared first on REBEL EM - Emergency Medicine Blog.
