
 Background: Pulseless electrical activity (PEA) is an organized electrical activity without a palpable pulse. 1/3 of cardiac arrest cases will be pulseless electrical activity and the overall prognosis of these patients is worse than patients who have shockable rhythms (ventricular fibrillation or pulseless ventricular tachycardia). It can be a challenge to decide when to terminate or continue resuscitation efforts in PEA arrest. Palpating pulses is difficult in the setting of a code situation, neither sensitive nor specific based on current literature. The use of POCUS could help split PEA patients into Pseudo-PEA (cardiac activity on US = profound shock) vs True-PEA (no cardiac activity on US) in determining the potential for ROSC.
Background: Pulseless electrical activity (PEA) is an organized electrical activity without a palpable pulse. 1/3 of cardiac arrest cases will be pulseless electrical activity and the overall prognosis of these patients is worse than patients who have shockable rhythms (ventricular fibrillation or pulseless ventricular tachycardia). It can be a challenge to decide when to terminate or continue resuscitation efforts in PEA arrest. Palpating pulses is difficult in the setting of a code situation, neither sensitive nor specific based on current literature. The use of POCUS could help split PEA patients into Pseudo-PEA (cardiac activity on US = profound shock) vs True-PEA (no cardiac activity on US) in determining the potential for ROSC.
REBEL Cast Episode 54 – What the Heck is Pseudo-PEA?
Click here for Direct Download of Podcast
What They Did: This was a systematic review and meta-analysis of studies that used US to predict ROSC
Outcomes: The major primary outcome was ROSC in this study.
Inclusion:
- Adult patients with PEA
- Cardiac US performed during resuscitation
- ROSC was the primary outcome
- Prospective, observational studies
- Written in English
Exclusion:
- Incomplete data
- Retrospective studies
Results:
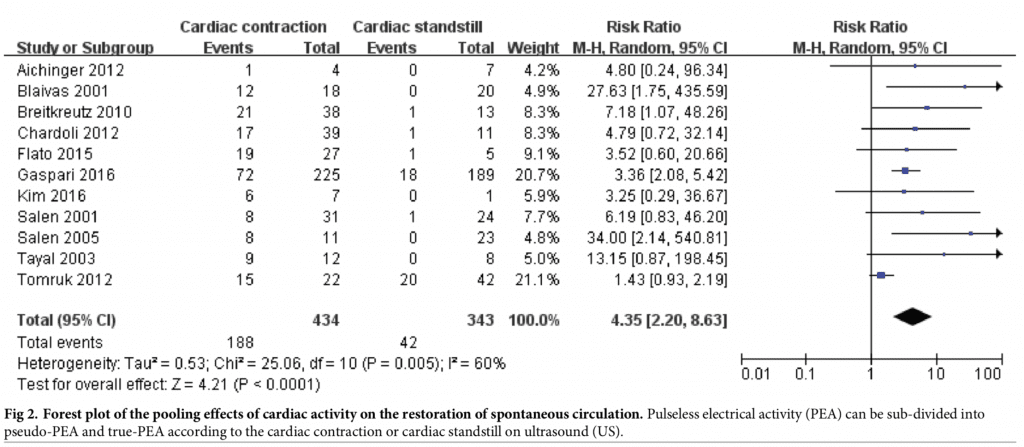
- 11 studies with 777 PEA patients were included in this analysis, with 230 patients achieving ROSC. Of the patients who achieved ROSC (81.7%), 188 of them had US identified cardiac activity (Pseudo PEA).
- PEA Cardiac Arrest Patients Achieving ROSC:
- Cardiac Activity on US: 188/434 (43.3%)
- No Cardiac Activity on US: 42/343 (12.2%)
- RR 4.35; 95% CI 2.20 – 8.63; p < 0.00001
- PEA patients with cardiac activity were 4.35x more likely to experience ROSC than one with cardiac standstill.
- PEA Cardiac Arrest Patients Achieving ROSC:
Strengths: This study asks a clinically important question and is the first analysis to evaluate PEA cardiac arrest patients alone. The authors also took into account heterogeneity between studies and performed a meta-regression analysis to analyze where the heterogeneity was stemming from.
Limitations: Things not assessed in this meta-analysis include downtime, time down without CPR, CPR duration, and medications used, all of which can affect outcomes in cardiac arrest. Also the major outcome was ROSC, which is the first step in evaluating cardiac arrest patients, but do to the limited data, survival and survival with good neurologic outcomes could not be completely assessed, which should always be the final common pathway in studies like this. Next the pooled sample size is still small, which is why the confidence intervals are so wide, limiting the results of this study. >40% of the patients included in this meta-analysis were from two studies, the other nine studies were all small trials. Another issue with this study is that, definitions of ROSC and “cardiac motion” on ultrasound were not consistent between studies adding to the heterogeneity. Finally, US evaluation results were not blinded to providers performing them which adds an additional layer of bias in whether to continue or terminate resuscitation efforts.
Discussion: Interestingly, in their meta-analysis, the authors found that using just a subxiphoid view only was not associated with ROSC in PEA arrest, but using various other views (i.e. parasternal long axis, apical 4 chamber view, etc) was associated with ROSC in PEA. This may be due to the inaccuracy of a single subcostal view, but this needs to be balanced as time doing ultrasound is time away from the things that matter for patients, high-quality CPR with limited interruptions.
Author Conclusion: “In cardiac arrest patients who present with PEA, bedside US has an important role in predicting ROSC. The presence of cardiac activity in PEA patients may encourage more aggressive resuscitation.”
Clinical Take Home Point: POCUS is an important tool in distinguishing pseudo-PEA (aka profound shock) from true-PEA, as differentiating having a pulse vs not having a pulse is difficult using palpation alone. Pseudo-PEA would benefit from pressor support as well, but use of POCUS should not delay high-quality CPR, and should not be used in isolation to determine whether to continue resuscitation efforts.
After Swami and I’s recording I was able to sit down with Joe Bellezzo and Scott Weingart to pick their brains about pulse checks, POCUS causing delays in CPR, 2 types of PEA, ECMO, and TEE. A quick summary of their thoughts are written below.
Special Guest

Joe “Hot Bear” Bellezzo
Chief of Emergency Medicine
Sharp Memorial Hospital
San Diego, CA
Blog: www.edecmo.org
Twitter: @edecmo
Pulse Checks
- Your Digitometer (Your Fingers) have a very low sensitivity at picking up pulses in profound shock
- If you don’t feel a pulse in profound shock your reflexive action is to resume CPR and give 1mg epinephrine, which may not be beneficial
- Use EtCO2 and arterial lines instead
POCUS Causing CPR Delays
- Do not let POCUS cause delays in CPR
- Delegate someone to count out loud to limit time off the chest doing CPR
- Cardiac Arrest Sonographic Assessment (CASA): Use a phased array probe in the subxiphoid view to look for: Pericardial Effusion, Right Heart Strain, and then Cardiac Activity. We don’t really have outcomes data with this and may never have outcomes data either
- We should stop remembering the H’s & T’s of PEA and instead look for the most common reversible causes with the use of POCUS. Almost all the T’s can be found with POCUS
- Joe likes to look for pericardial tamponade during his first rhythm check, then right heart strain at his second rhythm check (he prefers the parasternal long axis view for this), and cardiac activity on this third rhythm check. These are three biggest reversible causes of PEA that you can discover by POCUS
Two Types of PEA
- Pseudo PEA = Profound Shock –> Cardiac Activity Present; Patients with profound shock don’t necessarily need cpr and 1mg epinephrine, they need augmentation of cardiac output (i.e. push dose pressors)
- True PEA –> No Cardiac Activity Present
ECMO
- Candidates for ECMO are determined in a case by case manner
- ECMO is a bridge, by temporarily bypassing the heart and lungs, so that there is time to fix whatever the problem is that is causing shock
- The patients who benefit the most are PE or STEMI patients in profound shock
Special Guest

Scott “Hollywood” Weingart
Stony Brook Hospital
Stony Brook, NY
Clinical Associate Professor
Department of Emergency Medicine
Chief of the Division of Emergency Critical Care
Blog: EMCrit
Twitter: @emcrit
Pulse Checks
- Pulse checks are garbage in cardiac arrest
- A-lines in larger centers and in smaller centers US probe on femoral arteries during rhythm checks
POCUS Causing CPR Delays
- Don’t do multiple repeated ultrasounds of the heart as this increases hands off the chest time. In Scott’s opinion, you really only need one ultrasound to look for pericardial effusion generating tamponade.
- Scott went on to say that we shouldn’t bother looking for right heart strain because it is virtually impossible to differentiate PE vs no PE based on size of the right heart. Also during cardiac arrest we give intravenous fluids which will further increase the size of the right ventricle. This distinction can really only be made once the patient gets ROSC.
- Scott gets a single subxiphoid view while compressions are going on. When the rhythm then happens, Scott is able to get the view that he wants. One other tip he has learned is to hit record on the ultrasound machine so that when compressions resume, you can spend more time looking at the recording.
Two Types of PEA
- PRES (Pulseless with a Rhythm and Echocardiographic Standstill)
- PREM (Pulseless with a Rhythm and Echocardiographic Motion) –> This means patient has a functional heart but just not capable to produce a palpable pulse.
- At Scott’s shop they just run an epinephrine or norepinephrine infusion to give some background vasoconstriction. We did not discuss dose, however he is titrating to a MAP of 40mmHg. If this is not achieved then the patient needs CPR.
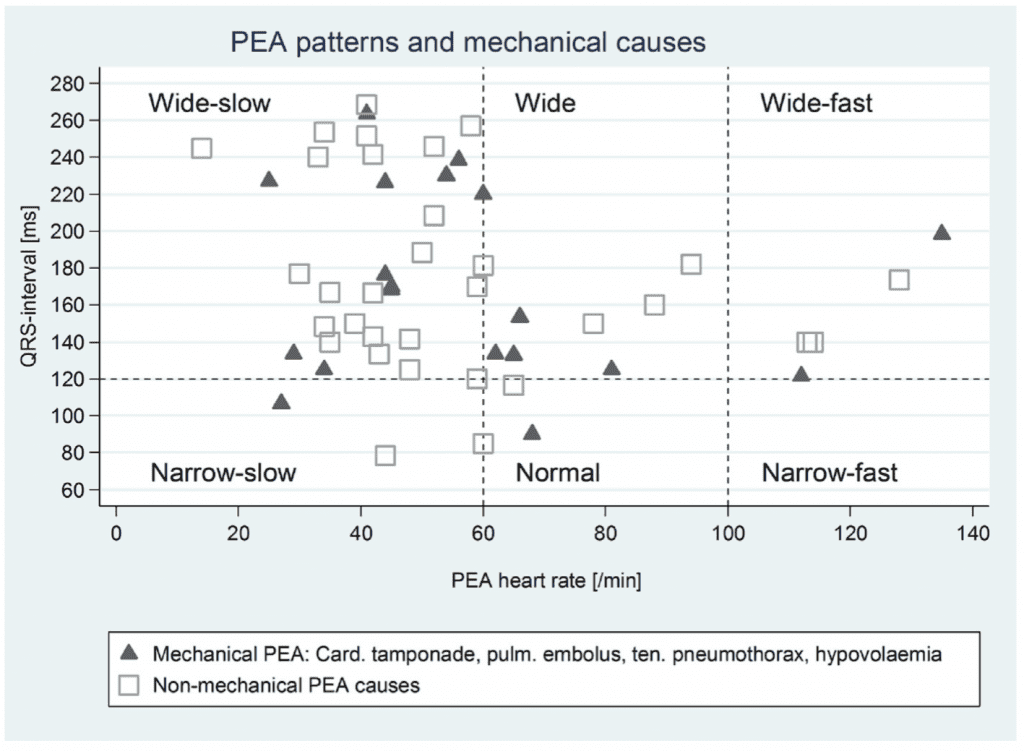
- Littman et al [3] wrote a paper in 2014 on a novel approach to PEA with the use of POCUS to determine the etiology of the PEA arrest. A QRS duration of ≥0.12 vs a QRS <0.12 was the initial branch point in determining etiology. The theory was narrow-complex PEA is generally due to mechanical problems caused by RV inflow or outflow obstruction and wide-complex PEA is typically due to metabolic problems, or ischemia, and LV failure. For more on this topic, checkout our REBEL EM blog post HERE. Scott and I also talked about a follow up study [2] to this (unfortunately after we finished recording) about QRS width not being a predictor of cause of PEA. In the follow up study 51 patients with IHCA and PEA arrest were prospectively observed. The key image from this publication is below, but the bottom line was no unique ECG patterns were associated with underlying cause of PEA (Consider this theory debunked).
TEE
- For the workshop on TEE checkout website: Resusitative TEE or the twitter handle @ResusTEEproject
- A 4 hour course is enough to get competency in TEE for ED cardiac arrest use
- The major hurdles for doing TEE are: Getting a probe, maintaining the probe, and hospital credentialing
- The reason this is a useful in cardiac arrest:
- Diagnosing the cause of the arrest
- Can see fine VF, which means shockable rhythm and not PEA
- Optimize the location of compressions
WARNING: Controversial Topic
- Scott thinks we should not be doing cardiac arrest at small EDs
- There is simply not enough man/woman power to offer things like ECMO, REBOA in viable arrest patients
- Post arrest care is different at cardiac arrest centers than it is in small EDs
- The reason this is so controversial is the hidden underlying message is that EMS should transport, potentially viable arrests to cardiac arrest centers and bypass the smaller EDs
References:
- Wu C et al. The Predictive Value of Bedside Ultrasound to Restore Spontaneous Circulation in Patients with Pulseless Electrical Activity: A Systematic Review and Meta-Analysis. PLos one 2018. PMID: 29364925
- Bergum D et al. ECG Patterns in Early Plulseless Electrical Activity- Associations with Aetiology and Survival of In-Hospital Cardiac Arrest. Resuscitation 2016. PMID: 27143124
- Littmann et al. A Simplified and Structured Teaching Tool for the Evaluation and management of Pulseless Electrical Activity. Med Princ Pract 2014. PMID: 23949188
For More Thoughts on This Topic Checkout:
- EDECMO: Does Pseudo-PEA Exist and What Should You Do About It
- Rory Spiegel at EMNerd (EMCrit): The Case of the Indiscriminate Wave Form
- Anton Helman at EM Cases: PEA Arrest, PseudoPEA, and PREM – With Simard and Weingart
- Scott Weingart at EMCrit: EMCrit 257 – Pulseless Electrical Activity (PEA) is Stupid
Post Peer Reviewed by: Anand Swaminathan, MD (Twitter: @EMSwami)
The post REBEL Cast Ep 54: What the Heck is Pseudo-PEA? appeared first on REBEL EM - Emergency Medicine Blog.
