 Background: Here we go again with another “Time is Brain,” acute ischemic stroke study. The authors start out by saying that earlier administration of intravenous tPA in acute ischemic stroke is associated with reduced mortality by the time of hospital discharge and better functional outcomes at 3 months. These statements are based on flawed studies [3][4] (Check out Ken Milne discussing these issues HERE). Additionally, tPA has not been demonstrated to decrease mortality in any randomized clinical trial though it does increase early mortality. If you can’t tell, I am very skeptical about the spin of this trial.
Background: Here we go again with another “Time is Brain,” acute ischemic stroke study. The authors start out by saying that earlier administration of intravenous tPA in acute ischemic stroke is associated with reduced mortality by the time of hospital discharge and better functional outcomes at 3 months. These statements are based on flawed studies [3][4] (Check out Ken Milne discussing these issues HERE). Additionally, tPA has not been demonstrated to decrease mortality in any randomized clinical trial though it does increase early mortality. If you can’t tell, I am very skeptical about the spin of this trial.
REBEL Cast Episode 84 – Here We Go Again with Time is Brain
Paper: Man S et al. Association Between Thrombolytic Door-to-Needle time and 1-Year Mortality and Readmission in Patients with Acute Ischemic Stroke. JAMA 2020. PMID: 32484532
Clinical Question: Is shorter door-to-needle times with tPA for acute ischemic stroke in patients ≥65 years associated with improved long-term outcomes?
What They Did:
- Retrospective cohort study of Medicare beneficiaries ≥65 years of age treated for acute ischemic stroke with intravenous tPA within 4.5 hours from the time last known well with 1 year follow up
- Patients collected from the Get With the Guidelines-Stroke Participating hospitals (See discussion for issues with this)
- Compared tPA administration at >45 min vs ≤45min and > 60 min vs ≤ 60 min
Outcomes:
-
Primary:
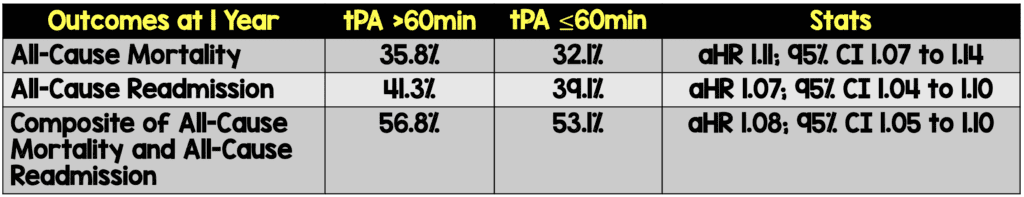
- 1-year all-cause mortality
- 1-year all-cause readmission
- 1-year composite of all-cause mortality or readmission
-
Secondary:
- 1-year cardiovascular readmission (primary discharge diagnosis of HTN, CAD, MI, CHF, abdominal or aortic aneurysm, valvular disease, and cardiac arrhythmias)
- Post-Hoc Secondary:
- Readmission for TIA, ischemic and hemorrhagic cc stroke, carotid endarterectomy or stenting, but not for direct complications of index stroke
Inclusion:
- ≥65 years of age
- Discharge diagnosis of acute ischemic stroke
- Treated with tPA within 4.5hrs since last known well
- Documented door-to-needle time
- 1st admission for stroke during the study period
Exclusion:
- Not treated with tPA
- Treated with concomitant therapy (i.e. intra-arterial reperfusion therapy)
- Missing onset-to-treatment time or treatment occurred >4.5hrs
- Missing door-to-needle time or treatment occurred >4.5hrs
- Transferred to another acute care hospital, left AMA, or without a documented site of discharge disposition
Results:
- 61,426 patients treated with tPA within 4.5hrs
- Median age = 80 years
- Median door-to-needle time = 65 min (Range 49 to 88 min)
- tPA >45 min = 48,666 (79.2%)
- tPA > 60 min = 34,367 (55.9%)
- 61,426 patients treated with tPA within 4.5hrs
- Median age = 80 years
- Median door-to-needle time = 65 min (Range 49 to 88 min)
- tPA >45 min = 48,666 (79.2%)
- tPA > 60 min = 34,367 (55.9%)
-
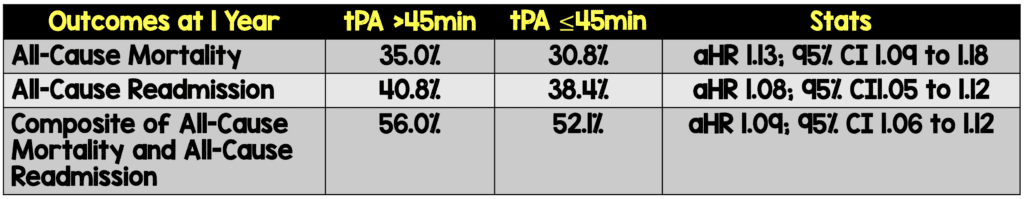
Every 15-minute increase in door-to-needle time was significantly associated with:
- Higher all-cause mortality aHR 1.04; 95% CI 1.02 to 1.05 within 90 min, but not after 90 min aHR 1.01; 95% CI 0.99 to 1.03
- Higher all-cause readmission aHR 1.02; 95% CI 1.01 to 1.03
- Higher composite of all0-cause mortality or readmission aHR 1.02; 9% CI 1.01 to 1.03
Strengths:
- Prior audit showed the overall accuracy of GWTG-Stoke registry above 90% for most variables, time-related performance measures had excellent reliability (k ≥0.75), and door-to-needle times within 60 minutes also had good reliability (k = 0.72)
- Patients treated during the 2015 – 2016 time frame (when endovascular thrombectomy use was increasing) were analyzed in the sensitivity analyses but excluded from the primary analysis
- No missing outcomes data
- NIHSS scores were well balanced at baseline between different time frames of door-to-needle times as was onset of symptoms to arrival time
- Further analyses performed in 15-minute increments in addition to the recommended treatment targets of 45 and 60 minutes
Limitations:
- Retrospective, observational trial which could result in residual unmeasured confounders including hospital resources and therefore can only be an association without causation
- Not an RCT of < 45 vs >45 years of age
- Factors that may have affected outcomes:
- It is unclear why patients were delayed (may have been because the diagnosis wasn’t clear, it was busier when the patients presented, or a host of other systems issues that could affect outcomes aside from the drug in question
- More delayed groups appeared to be sicker at baseline than the groups treated earlier (i.e. more hypertension)
- The combination of more difficulty in determining eligible patients and sicker patients are the exact patients that we should be taking more time to ensure no bad outcomes
- Most patients treated at teaching hospitals (77.7%) and primary stroke centers (73.2%) which decreases generalizability of results to smaller, rural, community settings
- 41,195 patients aged ≥65 who were treated with tPA within 4.5hrs of symptoms onset at GWTG-Stoke hospitals during the study period who met eligibility criteria were excluded due to inability to match to Medicare claims file data. These patients included a higher proportion of racial/ethnic minorities
- Data entry was manually done and self-reported by participating hospitals making the dataset only as good as what was recorded
- The results of this trial may not extrapolate to younger patients as this was a study of patients ≥65 years of age
- It is unclear how stroke diagnosis was made and how it was defined. Some proportion of patients may not have had acute ischemic stroke
- Selection bias: 8195 patients (13%) were excluded due to missing data on disposition, onset-to-treatment time, or door-to-needle time. We have no idea what happened to these patients
- We have no information on quality of life and functional outcomes
- The statistical significance in all categories was modest at best (i.e. close to crossing over 1)
- It is unclear what the cause of death was in these patients (i.e. from the tPA itself?)
Discussion:
- My issues with the Get With the Guidelines-Stroke participating hospitals:
- Reporting bias: submitting stroke mimic cases to the registry were encouraged but optional, meaning many mimic cases may not have been documented (i.e. we don’t know what happened to these patients).
- Selection bias: Limited to hospitals that were submitting at least 10 IV alteplase cases and 5 stroke mimic case per month. (i.e. smaller community hospitals with lower volumes were excluded)
- Voluntary program: Only hospitals that are interested in quality improvement in stroke care or had the capacity to fulfill requirements participated
- Pushing for more rapid administration will result in more patients with mimics getting tPA, more patients that aren’t eligible to get tPA (i.e. clinicians will miss exclusion criteria) and can result in worse outcomes. Interestingly, it is also more likely that stroke mimics get tPA if the push is to go faster (not taking to actually figure it out). This will both expose some patients to dangerous therapies they shouldn’t get while simultaneously making mortality and outcome measures look better since these patients will get better at a higher rate than true strokes.
Author Conclusion: “Among patients aged 65 years or older with acute ischemic stroke who were treated with tissue plasminogen activator, shorter door-to-needle times were associated with lower all-cause mortality and lower all-cause readmission at 1 year. These findings support efforts to shorten time to thrombolytic therapy.”
Clinical Take Home Point: I disagree with the authors conclusions of this trial. It is essentially impossible to draw any conclusions from this observational trial. Pushing for more rapid administration of tPA will include more stroke mimic cases making the earlier times look better and the more difficult patients with more comorbid disease (HTN) look worse in the later times of administration. Additionally, all the long-term outcomes were barely statistically significant, almost crossing 1.
References:
- Man S et al. Association Between Thrombolytic Door-to-Needle time and 1-Year Mortality and Readmission in Patients with Acute Ischemic Stroke. JAMA 2020. PMID: 32484532
- Fanari Z et al. Aggressive Measures to Decrease “Door to Ballon” Time and Incidence of Unnecessary Cardiac Catheterization: Potential Risks and Role of Quality Improvement. Mayo Clin Proc 2015. PMID: 26549506
- Emberson J et al. Stroke Thrombolysis Trialists’ Collaborative Group. Effect of Treatment Delay, Age, and Stroke Severity on the Effedts of Intravenous Thrombolysis with Alteplase for Acute Ischaemic Stroke: A Meta-Analysis of Individual Patient Data From Randomised Trials. Lancet 2014. PMID: 25106063
- Wardlaw J et al. Thrombolysis for acute Ischaemic Stroke. Cochrane Database Syst Rev 2014. PMID: 25072528
For More Thoughts on This Topic Checkout:
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post REBEL Cast Ep84: Here We Go Again with Time is Brain appeared first on REBEL EM - Emergency Medicine Blog.