
 Take Home Points
Take Home Points
- Osteomyelitis is an infection in any part of a bone. It has a varied presentation including acute and chronic forms. Patients can present septic, or rather well appearing.
- Patients may present with fever, chills, musculoskeletal pain, erythema, swelling or drainage from an ulcer.
- Lab evaluation includes WBC, ESR and CRP, which we expect to be elevated in acute osteo, but less so in chronic.
- MRI is the best imaging modality, but XR and CT may have some findings that suggest osteo.
- Unstable patients should be started on broad spectrum antibiotics, usually vancomycin and cefepime, right away. Stable patients can be started on antibiotics in conjunction with your orthopedic consults.
REBEL Core Cast 25.0 – Osteomyelitis
Click here for Direct Download of Podcast
Osteomyelitis:
-
It is an infection in any part of the bone. It can be divided into acute and chronic
- Acute – symptoms for less than two weeks
- Chronic – symptoms for more than 6 weeks
- Appears to have a bimodal distribution, the incidence is high in those younger than 20 and older than 50. With rising incidence in the elderly likely due to complications from diabetes
Source of Infection:
-
Hematogenous spread is when it’s from the blood to the bone.
- Risk factors include endocarditis, indwelling intravascular devices, orthopedic hardware, IV drug use, HD and sickle cell disease.
- Staph aureus is the most common cause of acute and chronic hematogenous spread osteo
- In kids consider strep species
- Sickle cell disease, IV drug use and puncture wounds: consider Salmonella
-
Direct inoculation is when its spread directly from source to bone
- Secondary to trauma or surgery which allows bacteria direct contact to the bone.
- Diabetics who develop neuropathy, skin breakdown and ulcerations.
- Check patients who are bed or wheelchair-bound for pressure ulcers
Signs and Symptoms:
-
Acute Osteomyelitis
- Fever, chills, erythema, musculoskeletal pain, swelling
-
Chronic Osteomyelitis
- Low-grade fever, pain at the site of infection, chronic ulcer might have purulent drainage
- One study of patients with osteomyelitis from diabetic foot ulcers had 64% with no signs of inflammation on the exam.
Lab Tests:
-
CBC, ESR, CRP
- Acute osteomyelitis will typically have leukocytosis as well as elevation in their inflammatory markers
- Chronic osteomyelitis the inflammatory markers may not be elevated
- Lab tests are non-specific
- Blood cultures – especially important if concern for hematogenous spread
- Probe to Bone test – most sensitive test. You can see an examples of this being performed here.

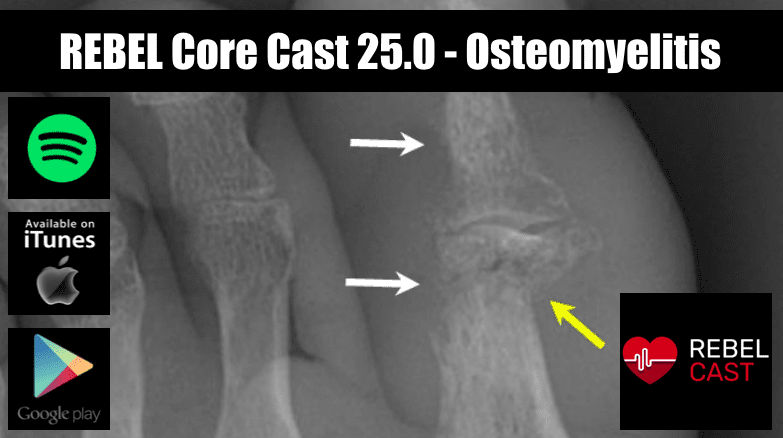
Imaging:
-
Start with Xray
- Swelling of the soft tissue, periosteal thickening or elevation, focal osteopenia
- Sensitivity is 43-75%, and the specificity is 75-83%, evidence of disease lags symptoms by about two weeks
-
CT scan
- thickened marrow density, intramedullary gas or areas of necrotic bone and soft tissue
- Sensitivity 67%, and specificity 50%
-
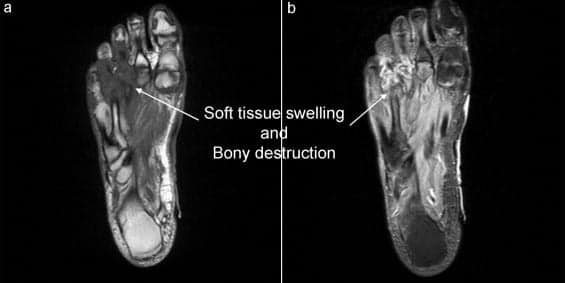
MRI
- Most difficult to get from ED
- Sensitivity 82-100%, and specificity 75-96%
Treatment:
-
Antibiotics
-
In stable patients, consult with orthopedics prior to antibiotic administration; may want to biopsy and culture site prior to antibiotics.
- You can tailor your antibiotics based on suspected organism using your hospitals guidelines and antibiogram. This article includes a great table of antibiotics by organism.
-
In unstable patients start antibiotics quickly and start broad
- Adult regimen: Vancomycin loading dose 25-30 mg/kg IV followed by 15-20 mg/kg q12h IV plus cefepime 2 g IV q8h.
- Pediatr ic regimen: Vancomycin 15 mg/kg IV q6h plus cefepime 50 mg/kg IV q12h if Pseudomonas is suspected.
-
In stable patients, consult with orthopedics prior to antibiotic administration; may want to biopsy and culture site prior to antibiotics.
-
Surgical debridement
- Discuss with orthopedics and will likely be necessary for patients with diabetic foot infections, direct inoculations, trauma complications, ortho hardware infections.
For More on This Topic Checkout:
- EM Docs: Osteomyelitis Making the diagnosis
References:
- Davenport Moira, Klein Matthew J. Osteomyelitis. In: Mattu A and Swadron S, ed. CorePendium. Burbank, CA: CorePendium, LLC. Link is HERE. Updated November 25, 2019. Accessed November 25, 2019.
- Hatzenbuehler J, Pulling TJ. Diagnosis and management of osteomyelitis. Am Fam Physician. 2011 Nov 1;84(9):1027-33. PMID 22046943
- Newman LG et al. Unsuspected Osteomyelitis in Diabetic Foot Ulcers. Diagnosis and Monitoring by Leukocyte Scanning with Indium in 111 Oxyquinoline. JAMA 1991. PMID: 1908030
- Lam K et al. Daignostic Accuracy of Probe to Bone to Detect Osteomyelitis in the Diabetic Foot: A Systematic Review. Clinical Infect Dis 2016. PMID: 27369321
- Rauker NP, Zink BJ. Bone and joint infections. In: Walls RM, Hockberger RS, Gasuche-Hill M, et al, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice. Vol 2. 9th ed. Philadelphia, PA: Elsevier; 2018:1693-1704.
Shownotes Written By: Miguel Reyes, MD (Twitter: @miguel_reyesMD)
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post REBEL Core Cast 25.0 – Osteomyelitis appeared first on REBEL EM - Emergency Medicine Blog.
