Take Home Points
- No palpable pulse does not equal no perfusion. We aren’t great at feeling pulses
- Patients with moderate to severe signs and symptoms of lithium toxicity should be considered for hemodialysis
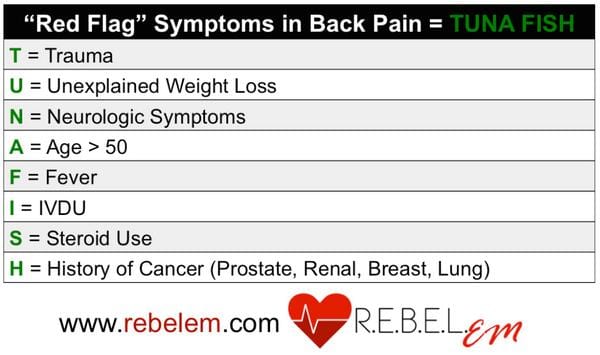
- Always consider serious causes of back pain before simply treating with analgesics
- Consider trauma as well as other toxic exposures (I.e. CO and CN) in patients with major burns
REBEL Core Cast 28.0 – Conference Pearls
Click here for Direct Download of Podcast
Sweat PEA – Dr. Eric Steinberg
-
Definition: the presence of organized rhythm without a palpable pulse
- No palpable pulse doesn’t = no perfusion (ie may be profound shock)
- Pulse palpation isn’t sensitive
-
We are bad at manually feeling for a pulse, instead use POCUS
- Use POCUS on carotid or femoral artery to look for pulse
- Establish an A-line
-
The biggest challenge is finding the cause
- 2014 established wide v. narrow complex causes. However, not well studied
- Use the RUSH exam to help determine cause
-
Patient Pre-Arrival
- Prep your Norepinephrine drip
- Equipment ready (airway, US, a-line, EtCO2)
- 2 people ready for CPR or mechanical device ready
- Get collateral info for cause
Lithium Toxicity – Dr. Monica Choski
-
Two forms of lithium
- Standard release peak 1-2 hours
- Extended release peak 4 hours
- 95% renal excretion
- Increased lithium levels often result outside of overdose when the patient takes a kidney hit (infection/medications) and GFR goes down.
-
Mild toxicity
- nausea, vomiting, hyperreflexia, agitation, muscle weakness
-
Mod toxicity
- stupor, rigidity, hypertonia, hypotension
-
Severe toxicity
- coma, convulsions
- Chronic Li toxicity – can develop nephrogenic DI
- Pearl: make sure you don’t send a lithium level in a lithium salt tube – typically a green top in the US
-
Management
- Get on the phone with consultant
- Activated Charcoal if the patient will take PO
- IV fluids to help GFR get back up
-
Dialysis
- Lithium >4
- Lithium >2.5 w/ renal insufficiency
- Moderate to severe signs of toxicity
Back Pain – Dr. Jim Gray
- Make sure the back pain isn’t from something dangerous; look for red flags
-
Medications
- First line: NSAIDs. Consider topical if patient cant systemic nsaid
- Trigger point injections
- Lidoderm patch
- Opiates and muscle relaxants never shown to be beneficial in comparison or addition to NSAIDs
- Send patients to follow up with PT & PMR
Burn Management – Dr. Jinal Sheth
- Major burn patients can have concomitant traumatic injuries along with tox exposures (CO, CN)
- Airway – intubate early if significant injuries because airway can be dynamic. Don’t just intubate if singed nose hairs – look for respiratory distress, stridor, hoarseness
-
Overestimate of BSA leads to excess fluid administration
- Use Lund-Browder chart
- Patient hand as an estimate, hand with fingers approximately 1%
-
Parkland may overestimate fluids needed
-
4ml/kg x %TBSA x body weight in kg
- First ½ in 8 hours, the second ½ in 16 hours
- Use Parkland for first 8 hours then titrate fluids to urine output of 0.5ml/kg
-
4ml/kg x %TBSA x body weight in kg
-
Aggressive pain management is key
- Consider ketamine if concomitant traumatic injury
-
Who to transfer to Burn Center
- Full Thickness burns
- Partial thickness burn >10%
- Burns to hand, face, genitalia, major joints, electrical/chemical burn, inhalation injury or special social needs
For More on These Topics Checkout:
- REBEL EM: What the Heck is Pseudo-PEA?
- LITFL: Lithium Toxicity
- LITFL: Burns
- Core EM: Nontraumatic lower back pain
Shownotes Written By: Miguel Reyes, MD (Twitter: @miguel_reyesMD)
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post REBEL Core Cast 28.0 – Conference Pearls appeared first on REBEL EM - Emergency Medicine Blog.
