Take Home Points
REBEL Core Cast 60.0 – Pyomyositis
Click here for Direct Download of Podcast
Pyomyositis: A purulent infection of the skeletal muscles that arise from hematogenous spread. Unlike necrotizing fasciitis that spreads from the skins down to the fascia and muscles, pyomyositis starts in the muscles itself.
Predisposing factors:
- Immunodeficiency (HIV, DM, cirrhosis, malignancy)
- Trauma (including vigorous exercise): hematoma and iron in the muscle bed creates a favorable medium for bacterial overgrowth.
- IV drug use induced bacteremia (note: the muscles involved will not be near the local injection site)
- Concurrent infections
- Malnutrition
Microbiology
- Staphylococcus aureus is the most common cause of pyomyositis (including MRSA)
- Less commonly: non-group A, beta-hemolytis streptococci, pneumococcie, gram negative enteric bacilli, mycobacterium and polymicrobial
Clinical Manifestations
- Fever + pain with cramping localized to a single muscle group
- Usually the lower extremities are affected (thigh, calf, gluteal muscles) but any muscle group can be involved (iliopsoas, pelvic, trunk, paraspinal, upper extremity)
- 20% of cases can have multifocal infection involving more than one muscle group.
- Pyomyositis has 3 clinical stages:
- Crampy, local muscle pain, swelling, +/- low grade fever. The muscle may have a “woody” texture on palpation and may be indurated. No fluctuance is felt and aspiration may not yield purulent material.
- Occurs 10- 20 days after the initial symptoms and is characterized by fever, exquisite muscle tenderness and edema. A frank abscess may be apparent and aspiration usually yields pus.
- Systemic toxicity: the affected muscle is fluctuant. Complications of bacteremia such as septic shock, endocarditis, septic emboli, pneumonia, pericarditis, septic arthritis, brain abscess, acute renal failure, rhabdomyolysis all may be present.
Differential Diagnosis
- Muscle strain
- Contusion
- Hematoma
- Cellulitis
- Deep vein thrombosis
- Osteomyelitis
- Septic arthritis
- Neoplasm
- Clostridial myonecrosis
- Necrotizing fasciitis
- Spontaneous gangrenous myositis
- Diabetic muscle infarction
- Septic arthritis
Diagnosis
- Radiography
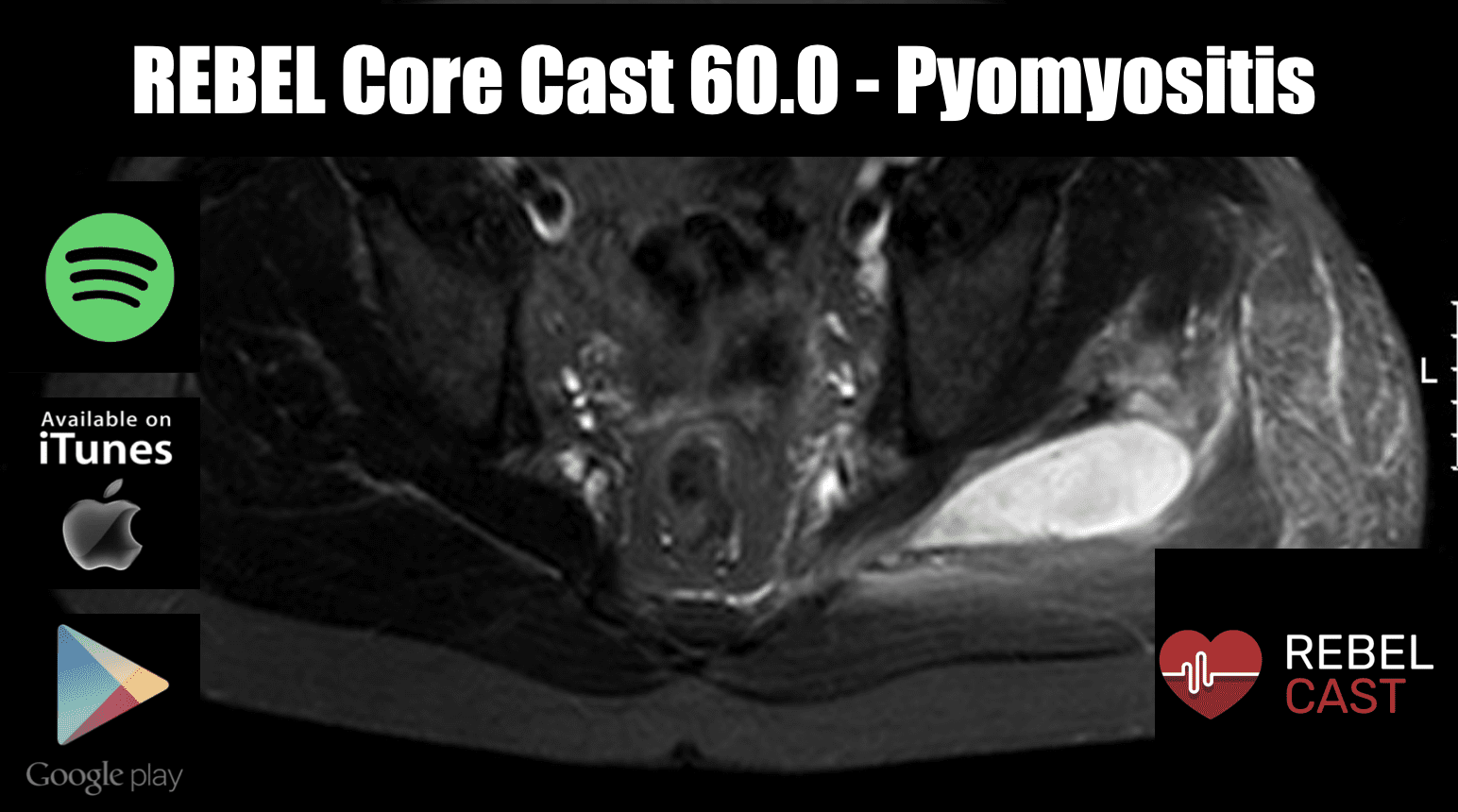
- MRI is the most optimal. Shows muscle inflammation even before abscess formation.
- CT scan with intravenous contrast will detect muscle swelling and well defined areas of fluid attenuation that display rim enhancement.
- Ultrasound with show diffuse muscle hyperechogenicity with or without local hypoechogenicity
- Cultures
- Laboratory data are nonspecific (e.g leukocytosis, elevated inflammatory markers)
Treatment
- Stage 1 can be treated with antibiotics
- Most patients will require both antibiotics and drainage or surgical intervention
- Initial empiric IV antibiotics directed at staphylococci (including MRSA and beta- hemolytic streptococci).
- In immunocompromised patients use broad coverage for gram-positive, gram-negative and anaerobic organisms.
- Clindamycin can be used in severe infection because it suppresses synthesis of bacterial toxins, and has longer post-antibiotic effects.
- 3-4 weeks parental IV therapy is usually sufficient. It can be longer in those with poorly drained infections or who have extensive disease.
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post REBEL Core Cast 60.0 – Pyomyositis appeared first on REBEL EM - Emergency Medicine Blog.