
 Take Home Points
Take Home Points
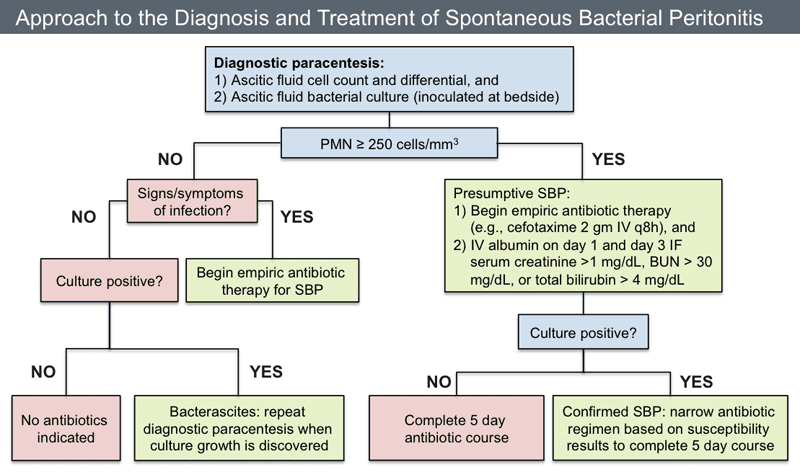
- Spontaneous Bacterial Peritonitis (SBP) is a difficult diagnosis to make because presentations are variable. Consider a diagnostic paracentesis in all patients presenting to the ED with ascites from cirrhosis
- An ascites PMN count > 250 cells/mm3 is diagnostic of SBP but treatment should be considered in any patient with ascites and abdominal pain or fever
- Treatment of SBP is with a 3rd generation cephalosporin with the addition of albumin infusion in any patient meeting AASLD criteria (Cr > 1.0 mg/dL, BUN > 30 mg/dL or Total bilirubin > 4 mg/dL)
REBEL Core Cast 89.0 – Spontaneous Bacterial Peritonitis
Definition: Acute infection of the ascitic fluid in a patient with liver disease without another source of infection
Epidemiology (Runyon 1988, Runyon 1988, Borzio 2001)
- Incidence
- 10-25% risk of at least one episode per year
- 20% risk in those with ascites admitted to the hospital
- Historically, mortality ~ 50%
Pathophysiology
- Not completely understood
- Increased portal systemic hypertension
- Causes mucosal edema of the bowel wall
- Increases transmural migration of enteric organisms into the ascitic fluid
- Impaired phagocytic function in the liver
- Impaired immunologic activity in ascitic fluid
Presentation
- Classic triad: fever, abdominal pain and increasing ascites. Presence of all three components uncommon
- Symptoms
- Fever or chills
- Abdominal pain
- Abdominal swelling
- Fatigue
- Malaise
- Signs
- Abdominal tenderness variable
- Typically diffuse
- Can be mild without peritoneal signs
- Can be severe with rebound and/or guarding
- Abdominal distension
- Altered mental status (from hepatic encephalopathy)
- Abdominal tenderness variable
Diagnostics
- Obtaining an ascitic fluid sample is critical in making the diagnosis
- Serum blood tests (i.e. WBC, CRP, ESR) are not helpful in making this diagnosis
- Due to variable presentations and considerable mortality associated with SBP, consideration should be made to perform paracentesis on ALL patients with ascitic fluid who are being admitted (Gaetano 2016)
- Diagnostic paracentesis (EM: RAP HD)
- Ascitic fluid assays
- Cell count
- Look for WBC > 250-500 cells/mm3 or neutrophil count > 250 cells/mm3
- Peritoneal dialysis patients: neutrophil count > 100 cells/mm
- pH < 7.34 more common in SBP (Wong 2008)
- Ascitic fluid gram stain (rarely positive) and culture
- Cell count
- If patient has fever (temp > 100oF) or abdominal pain/tenderness, empiric antibiotics should be given even if neutrophil count < 250 cells/mm3
Management
- Antibiotics
- Most common bacterial causes: E. Coli, S. Pneumoniae, Enterococci
- 3rd Generation Cephalosporin covers vast majority of cases
- Ceftriaxone 25 mg/kg up to 1 gm daily
- Cefotaxime 25 mg/kg up to 1 gm Q8
- Alternate antibiotic choices
- Ciprofloxacin 400mg IV BID
- Levofloxacin 750mg IV daily
- Piperacillin/Tazobactam 4.5g IV TID
- Ertapenem 1g IV qD
- Imipenem/Cilastatin 500mg IV QID
- Albumin Infusion (Runyon 2012)
- Recommended by American Association for the Study of Liver Disease (AASLD) in specific subgroups with SBP
- Presence of any of the following should prompt albumin administration
- Serum creatinine > 1 mg/dL
- Blood urea nitrogen (BUN) > 30 mg/dL
- Total Bilirubin > 4 mg/dL
- Impact of albumin infusion (Sort 1999)
- 25% reduction in renal failure
- 20% reducing n mortality
- Dose
- 1.5 grams/kg within 6 hours
- 1.0 grams/kg on day 3 of treatment
- Recommended by American Association for the Study of Liver Disease (AASLD) in specific subgroups with SBP
- Patients with a single episode of SBP should be considered for antibiotic prophylaxis (with norfloxacin, ciprofloxacin or TMP/SMX) (Runyon 2012)
Take Home Points
- SBP is a difficult diagnosis to make because presentations are variable. Consider a diagnostic paracentesis in all patients presenting to the ED with ascites from cirrhosis
- An ascites PMN count > 250 cells/mm3 is diagnostic of SBP but treatment should be considered in any patient with ascites and abdominal pain or fever
- Treatment of SBP is with a 3rd generation cephalosporin with the addition of albumin infusion in any patient meeting AASLD criteria (Cr > 1.0 mg/dL, BUN > 30 mg/dL or Total bilirubin > 4 mg/dL)
Read More
- Oyama LC: Disorders of the liver and biliary tract, in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 8. St. Louis, Mosby, Inc., 2010, (Ch) 90: p 1186-1205.
- EMRAP: C3 Live Paracentesis Video
- LITFL: Spontaneous Bacterial Peritonitis
- SinaiEM: SBP Pearls
- REBEL EM: Should You Give Albumin in Spontaneous Bacterial Peritonitis (SBP)?
- References
- Runyon BA et al. Ascitic fluid analysis in malignancy‐related ascites. Hepatology 1988; 8(5):
- 1104-1109. PMID: 3417231
- Runyon BA. Spontaneous bacterial peritonitis: An explosion of information. Hepatology 1988; 8: 171–175. PMID: 3338704
- Borzio M et al. Bacterial infection in patients with advanced cirrhosis: a multicentre prospective
- study. Dig Liver Dis 2001; 33(1): 41-48. PMID: 11303974
- Gaetano et al. The benefit of paracentesis on hospitalized adults with cirrhosis and ascites. Journal of Gastroenterology and Hepatology 2016. PMID: 26642977
- Wong CL et al. Does this patient have bacterial peritonitis or portal hypertension? How do I perform a paracentesis and analyze the results? JAMA 2008; 299(10):1166-78. PMID: 18334692
- Runyon BA. Management of Adult Patients with Ascites Due to Cirrhosis: Update 2012. AASLD Practice Guideline. Link
- Sort P et al. Intravenous albumin in patients with cirrhosis and spontaneous bacterial peritonitis.
- NEJM 1999; 341: 1773-4. PMID: 10432325
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post REBEL Core Cast 89.0 – Spontaneous Bacterial Peritonitis appeared first on REBEL EM - Emergency Medicine Blog.
