
 I have started to split my time between the ED and ICU. Obviously these two areas of clinical care have their similarities, but also have their differences. So I decided to create this post to put things that I have found useful and recurrently coming back to when on my critical care time. This is not meant to be an EBM based post, but rather a clinical post of useful critical care/ICU information. I will continue to add to this post as I spend more time in the ICU and hopefully this becomes a nice repository of information for others.
I have started to split my time between the ED and ICU. Obviously these two areas of clinical care have their similarities, but also have their differences. So I decided to create this post to put things that I have found useful and recurrently coming back to when on my critical care time. This is not meant to be an EBM based post, but rather a clinical post of useful critical care/ICU information. I will continue to add to this post as I spend more time in the ICU and hopefully this becomes a nice repository of information for others.
Vaso/InoPressors
- Milrinone 0.125-0.75 mcg/kg/min
- Isoproteronol 2-10 mcg/min
- Dobutamine 2-20 mcg/kg/min
- Epinephrine 0.01-0.1 mcg/kg/min
- Norepinephrine 0.01-1 mcg/kg/min
- Phenylephrine 0.1-1.0 mcg/kg/min
- Vasopressin 0.01-0.06 U/min
Antiarrhythmics
- Amiodarone 150mg bolus followed by 1mg/min x6hrs, then 0.5mg/min x18hrs
- Digoxin 250mcg IV q2hrs x3, then 125 to 375mcg qday
- Esmolol 500mcg/kg IV bolus, then 50mcg/kg/min (titrate by 50mcg/kg/min q5min)(Max dose 200mcg/kg/min)
- Procainamide 10 – 20mg/kg IV bolus over 20min, then 1 to 4mg/min
- Lidocaine 1mg/kg (50 to 100mg) IV over 2 – 4 min, then 1 – 4mg/min
Sedation:
- Ketamine 0.5 – 2mg/kg IV bolus, then 0.05 – 0.4mg/kg/hr
- Dexmedetomidine 0.2 – 1.4mcg/kg/hr
- Propofol 0.5 – 1mg/kg IV bolus, then 5 to 80mcg/kg/min
Paralytic Infusions
- Vecuronium
- Bolus: 0.1mg/kg
- Infusion: 1mcg/kg/min adjust dose by 0.3 mcg/kg/min q15 minutes (MAX Dose 1.7mcg/kg/min)
- Cisatracurium
- Bolus: 0.2mg/kg
- Infusion: 1 mcg/kg/min, adjust dose by 0.5 mcg/kg/min q 15 minutes (MAX Dose 10mcg/kg/min)
Options to Reduce Pulmonary Vascular Resistance in RV Failure
- Esoprostenol 0.05mcg/kg/min
- iNO 20 – 40ppm
- Alternative Options
- Inhaled Milrinone (1mg/1mL) 5mg over 15min
- Inhaled NTG (1mg/1mL) 5mg over 15min
Things to Consider Prior to Extubation
- RSBI <100 = RR/TV (Liters)
- MV <10 = RR x TV
- Pick up Head
- PEEP <8
- FiO2 <50%
- PaO2 >60
- Cough
Follow Commands - Low Secretions
- Cuff Leak
Anticoagulation
- Bivalirudin
- Half-Life = 25min (with normal renal function)
- Mechanism of Action = Direct Thrombin Inhibition
- Protein Binding = None
- Metabolism/Excretion = Combo of proteolytic cleavage + Renal
- Monitor with PTT level
- No Antidote BUT short half life (back to baseline coagulation at ≈1hr)
- No risk of HIT
- Argatroban
- Half-Life = 45min (with normal liver function)
- Mechanism of Action = Direct Thrombin Inhibition
- Protein Binding = 20% albumin/30% alpha-acid glycoprotein
- Metabolism/Excretion = Liver
- Monitor with PTT level
- No Antidote BUT back to baseline coagulation at 2 – 4hrs
- No risk of HIT
Cardiac Indices:
- NORMAL
- CO = 4 – 8L/min
- CI = 2.5 – 4.2L/min/m2
- SVR = 900 – 1600 dynes/sec/cm-5
- PCWP = 6 – 12mmHg
- HYPOVOLEMIC
- Decreased CO + PWP + CVP
- Increased SVR
- CARDIOGENIC
- Increased SVR + PWP + CVP
- Decreased CO
- DISTRIBUTIVE
- Decreased SVR + PWP + CVP
- Increased CO
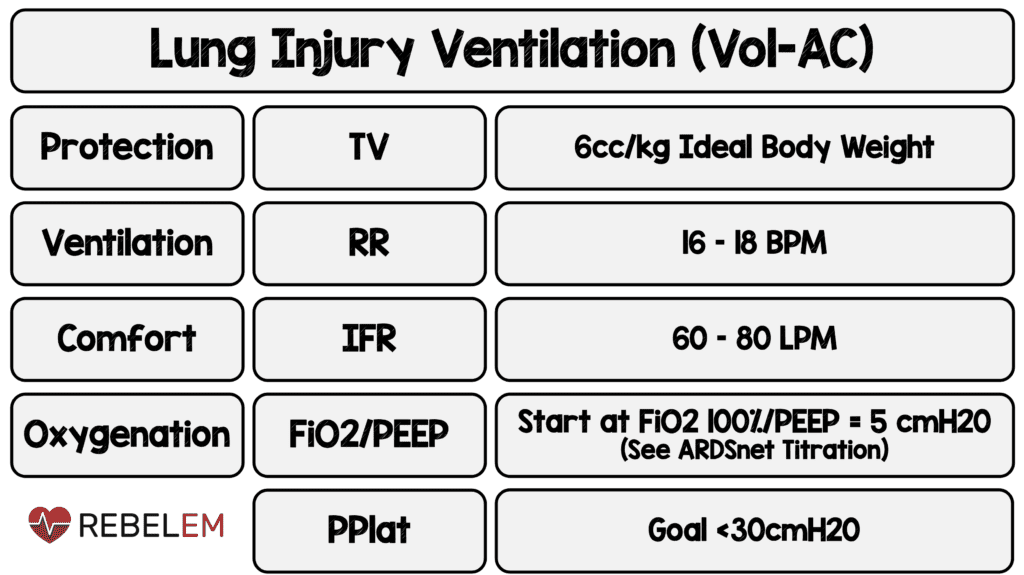
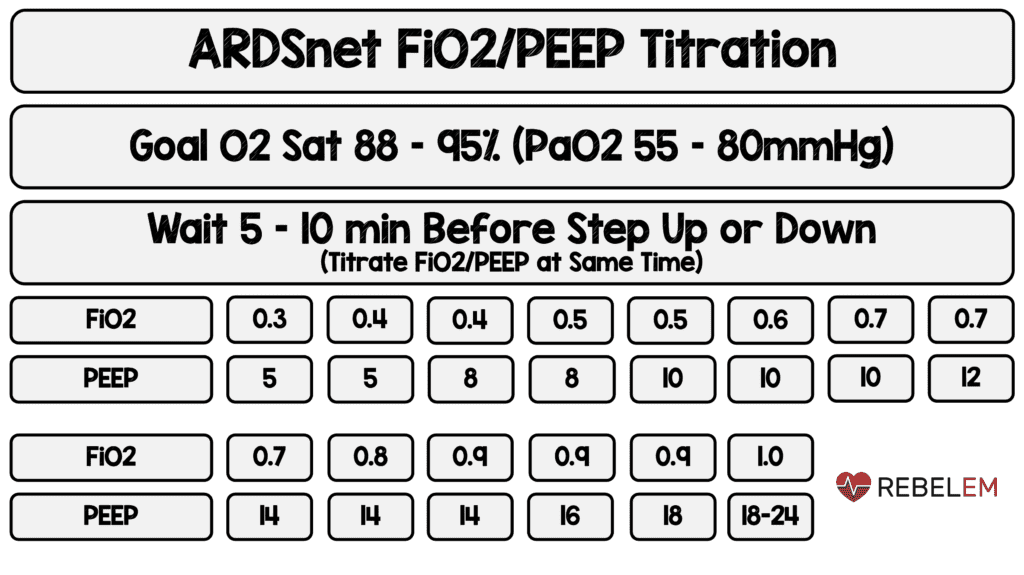
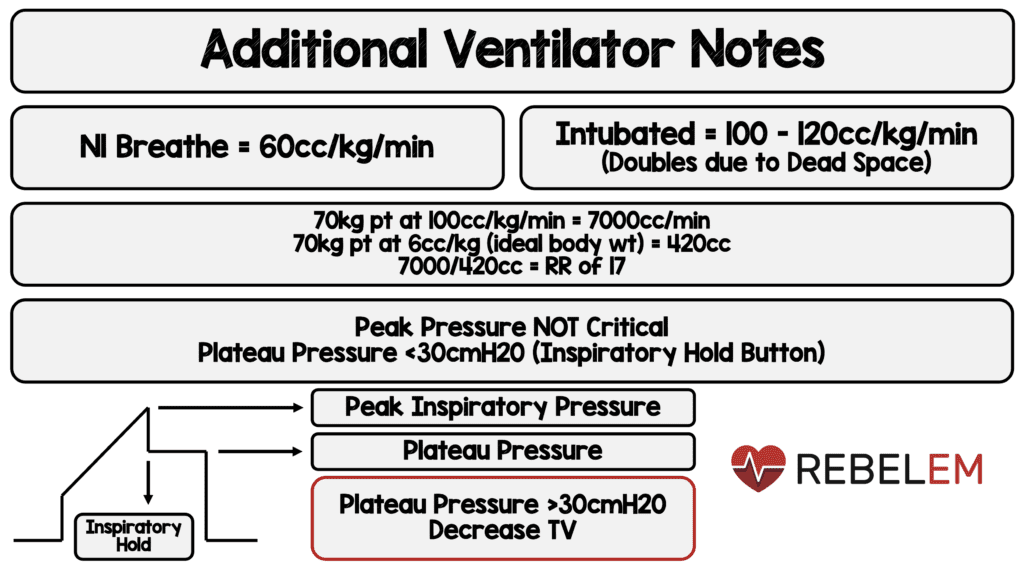
Invasive Mechanical Ventilation
ExtraVentricular Drains (EVDs)
SETUP:
Laser Beam —> Level with tragus
Proximal Stop Cock —> Clearance of blood products/infection
Collecting Chamber —> Up or down to set desired pressure
Distal Stop Cock —>
-“Off” to the right – Allows Drainage
-“Off” to the floor – Zeroing
-“Off” to the ceiling – Clamped
-20cmH20 ≈ 15mmHg
-20mmHg ≈ 27cmH20
Clamp EVD (“Off” to ceiling) for ICP pressure
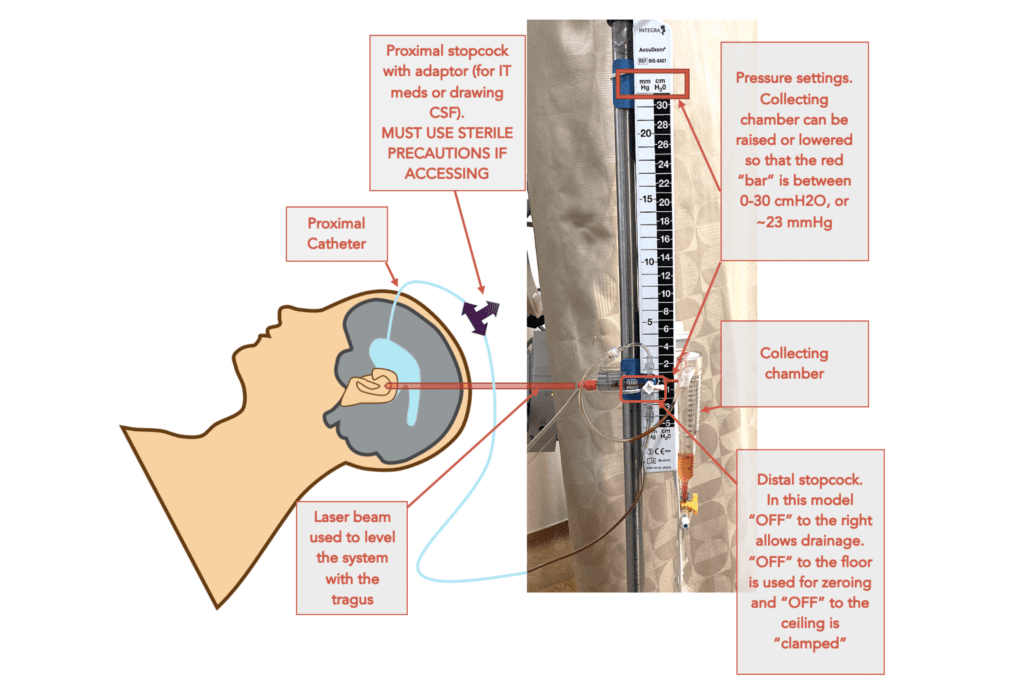 Image from EMCrit Site (Link is HERE)
Image from EMCrit Site (Link is HERE)
WAVEFORMS:
P2>P1 = Decreased Compliance
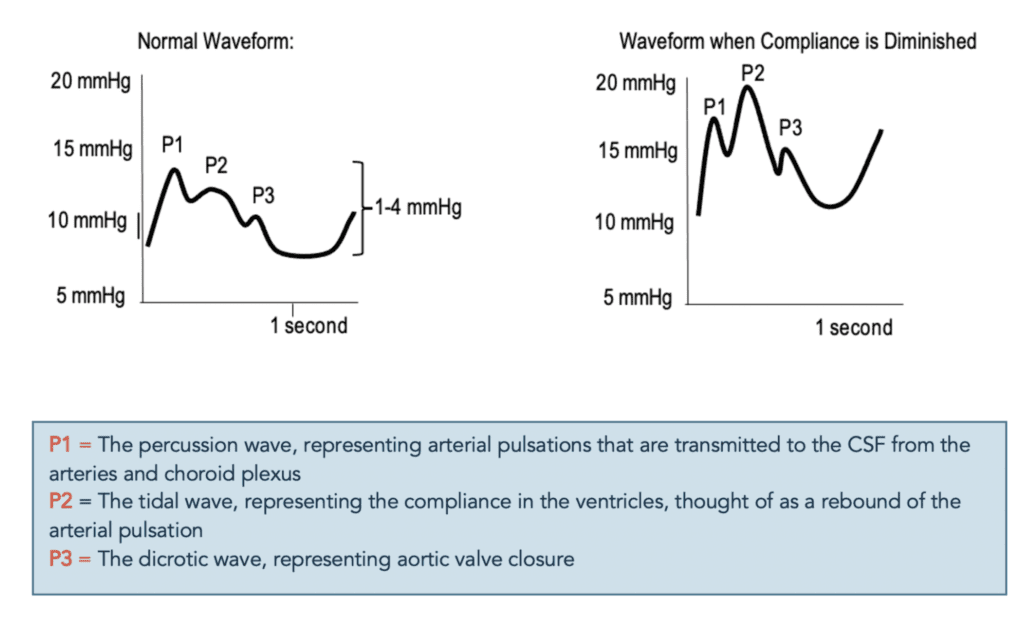
Image from EMCrit Site (Link is HERE)
CEREBRAL PERFUSION PRESSURE (CPP):
CPP = MAP – ICP
MAP from A-Line
ICP from EVD
COMPLICATIONS:
Ventriculitis —> Send CSF
Bleeding —> Head CT
Overdrainage —>
-CSF Made = 600cc/day or 20cc/hr
->350cc/day can lead to this
Catheter Occlusion —> Talk to Neurosurg
MONITORING:
ICP Value Range
ICP Waveform
CSF Color
Daily/Hourly Output
Coagulation Status
2 Options for Elevated ICP in Severe TBI
-
Mannitol
- Bolus Only
- Onset 30min
- Lasts 6hrs
- Causes Osmotic Diuresis
- Dose 0.25 – 2g/kg over 30 to 60min
-
HTS (3%)
- Bolus or Drip
- Onset 5min
- Lasts 12hrs
- No Diuretic Effect
- Dose 300mL over 1hr
The post REBEL EM Useful Critical Care/ICU Stuff appeared first on REBEL EM - Emergency Medicine Blog.
