
 In this 14-minute presentation from Rebellion in EM 2021, Dr. Tarlan Hedayati, MD discusses the shift from the paradigm of STEMI/NSTEMI to OMI/NOMI.
In this 14-minute presentation from Rebellion in EM 2021, Dr. Tarlan Hedayati, MD discusses the shift from the paradigm of STEMI/NSTEMI to OMI/NOMI.

Tarlan Hedayati, MD
Emergency Medicine
Cook County Health
Twitter: @HedayatiMD
Objectives
1. Review the history of STEMI/NSTEMI designation and current OMI/NOMI paradigm
2. Discuss the risks of management decisions based on the STEMi/NSTEMI designation
2. Review the evidence regarding advantages of the OMI/NOMI paradigm
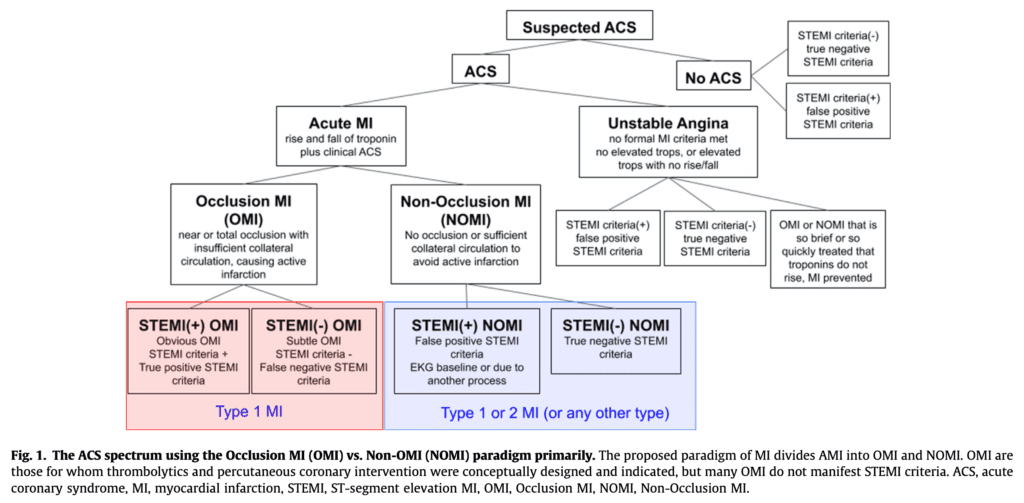
Redefining Coronary Ischemia (OMI vs NOMI)
- ST-Elevation Myocardial Infarction (STEMI) doesn’t always equal occlusion myocardial infarction (OMI)
- OMI doesn’t always manifest as ST-elevation on the ECG (i.e. hyperacute T waves, etc…)
- 2014 AHA/ACC guideline (Amsterdam et al, Circ 2014) for the management of patients with NSTEMI indicated that there are some NSTEMI patients that would benefit from:
- Immediate invasive strategy (i.e. <2hrs)
- Refractory Angina
- Recurrent Angina
- Sustained VT/VF
- Hemodynamically Unstable
- Early invasive strategy (i.e. 2 – 24hrs)
- Dynamic ECG (i.e. New ST depression)
- Rising Troponin
- Delayed invasive strategy (i.e. 24 – 72hrs)
- DM
- CKD
- EF <40%
- CABG/PCI <6mo
- Post-MI pain
- Systematic Review and Meta-Analysis (Khan et al, Eur Heart J, 2017):
- 7 studies with 40,777 patients with NSTEMI
- 5% had an occluded culprit artery
- These patients had increased risk of increased short-term and long-term mortality
- Comparison of STEMI/NSTEMI vs OMI/NOMI (Meyers et al, J Emerg Med, 2021)
- Immediate invasive strategy (i.e. <2hrs)
-
-
- 467 patients
- 448 cardiac catheterization
- 108 had OMI
- 67 had STEMI
- 41 patients (38%) didn’t not meet STEMI criteria but had OMI
- Median time to cath:
- STEMI (+) OMI: 41min
- STEMI (-) OMI: 437min
-
- Retrospective Case-Control Study (Meyers et al, IJC Heart and Vasc, 2021):
- 808 patients with suspected acute coronary syndrome
- 49% had acute myocardial infarction
- 33% OMI
- 16% NOMI
- 265 patients with OMI
- 108 patients met STEMI criteria
- Sensitivity = 41%
- OMI ECG Criteria not Meeting STEMI Criteria:
- Subtle STE: 83%
- Reciprocal ST depression and/or negative hyperacute T waves: 82%
- Terminal QRS distortion: 53%
- Inferior STE and any STD/TWI in aVL: 50%
- Hyperacute T waves: 49%
- STD maximal in V1 – V4: 45%
- Acute pathologic Q waves: 47%
- DIFOCCULT Trial (Aslanger et al, IJC Heart and Vasc, 2020):
- 1000 STEMI patients
- 1000 NSTEMI patients
- 1000 control patients
- Of the 1000 NSTEMI patients, 282 (28.2%) were reclassified as OMI
- Reclassified NSTEMI patients were more like STEMI patients than non-reclassified NSTEMI patients
- Acute Coronary Occlusion:
- STEMI: 85%
- Re-Classified NSTEMI: 61%
- Non-Re-Classified NSTEMI: 25%
- In-Hospital Mortality:
- STEMI: 8%
- Re-Classified NSTEMI: 5%
- Non-Re-Classified NSTEMI: 2%
- Long-Term Mortality:
- STEMI: 14%
- Re-Classified NSTEMI: 11%
- Non-Re-Classified NSTEMI: 4%
- OMI/NOMI is not perfect and still missed 17% of acute coronary occlusions, but significantly better than STEMI/NSTEMI criteria
- Acute Coronary Occlusion:
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post Rebellion21: Time to Evolve – Redefining Coronary Ischemia – The OMI/NOMI Paradigm via Tarlan Hedayati, MD appeared first on REBEL EM - Emergency Medicine Blog.
