
 Background: Although the standard positioning for intubation is supine in the sniffing position, there has been recent literature in the past decade that elevating the head of the bed to 25 to 30 degrees may be a preferable setup for direct laryngoscopy due to improved laryngeal view and reduced airway complications. These studies have been conducted in multiple settings and patient populations including the prehospital setting, the emergency department, and the operating room (for elective cases). Additionally, video-assisted laryngoscopy has been a relatively recent innovation in airway management: the first video laryngoscope produced commercially became available in 2001. Similarly, this technology has been studied in multiple settings including in the emergency department and in the operating room. Both head-elevated direct laryngoscopy and video-assisted laryngoscopy have been studied with a variety of outcomes including first-pass success rate, time to intubation, and mortality rates. However, despite video-assisted laryngoscopy becoming increasingly ubiquitous, its limitations include a high cost and the possibility of components becoming damaged. Both of these innovations in intubation—video-assisted laryngoscopy and elevating the head of the bed—remain debated within the field of emergency medicine.
Background: Although the standard positioning for intubation is supine in the sniffing position, there has been recent literature in the past decade that elevating the head of the bed to 25 to 30 degrees may be a preferable setup for direct laryngoscopy due to improved laryngeal view and reduced airway complications. These studies have been conducted in multiple settings and patient populations including the prehospital setting, the emergency department, and the operating room (for elective cases). Additionally, video-assisted laryngoscopy has been a relatively recent innovation in airway management: the first video laryngoscope produced commercially became available in 2001. Similarly, this technology has been studied in multiple settings including in the emergency department and in the operating room. Both head-elevated direct laryngoscopy and video-assisted laryngoscopy have been studied with a variety of outcomes including first-pass success rate, time to intubation, and mortality rates. However, despite video-assisted laryngoscopy becoming increasingly ubiquitous, its limitations include a high cost and the possibility of components becoming damaged. Both of these innovations in intubation—video-assisted laryngoscopy and elevating the head of the bed—remain debated within the field of emergency medicine.
What They Did:
- Single center, randomized, controlled, single-blind, non-inferiority trial in Malaysia
- Operating room setting in American Society of Anesthesiologists (ASA) I to III patients (n=138) undergoing elective surgery under general anesthesia with endotracheal intubation
- Anesthesia was induced with preoxygenation until ETO2 of 85% was achieved, followed by IV fentanyl 2 µg/kg and IV propofol 2–3 mg/kg followed by IV rocuronium 0.5–1.2 mg/kg or IV atracurium 0.5 mg/kg
- Obtained baseline direct laryngoscopy in the supine sniffing position, then compared direct laryngoscopy using a Macintosh blade (size 3 or 4) with the head elevated to 25 to 30 degrees to video-assisted laryngoscopy using a hyperangulated blade in the supine sniffing position
Patient Positioning & Definitions:
- Group BUHE patients were positioned in the BUHE position, which was achieved by breaking the operating table at the hip joint and elevating the head of the bed up to 20° to 30°, with end point being horizontal alignment between the patient’s external acoustic meatus and sternal angle.
- A 100% POGO score refers to visualization of the entire glottic opening from the anterior commissure of the vocal cords to the interarytenoid notch. A POGO score of 0% refers to no visualization of laryngeal structures.
- The Cormack-Lehane classification system has four categories: complete view of the glottis, partial view of the glottis, view of the epiglottis but not the glottis, and view of neither the glottis nor the epiglottis.
- Time required for intubation (TRI) was measured in seconds, from the moment the tip of the laryngoscope blade passes through the incisors to the first detected EtCO2, by a separate anesthesiologist not involved in the study.
- Failure to intubate was defined as failure after 3 attempts.
- Hypoxia was defined as SpO2 <92%, while hypotension was defined as MAP <60 mm Hg.
Outcomes:
- Primary: Laryngeal exposure as measured by the Percentage of Glottic Opening (POGO) score
-
Secondary:
- Cormack-Lehane classification
- Time required for intubation, as measured by time from the laryngoscope passes the teeth until the time end-tidal CO2 is detectable.
- Number of intubation attempts
- Need for airway adjuncts
- Need for external laryngeal manipulation
- Subjective effort during intubation ranked from 0 to 10
- Intubation complications (e.g., hypotension, hypoxia, esophageal intubation)
Inclusion Criteria:
- Age 18-75
- Undergoing elective surgery under general anesthesia with endotracheal intubation
- American Society of Anesthesiologists (ASA) classification I to III
Exclusion Criteria:
- History of ischemic heart disease, cerebrovascular disease, or respiratory disease
- Body mass index (BMI) >35
- Patients requiring rapid sequence induction
- Patients with an airway obstruction
- Patients with a small mouth opening
- Contraindication to neck extension
Results:
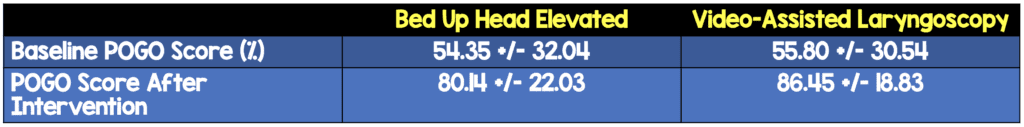
- Using a noninferiority margin of −15% for the difference in POGO scores between video-assisted laryngoscopy and bed-up-head-elevated direct laryngoscopy, bed-up-head-elevated direct laryngoscopy was found to be non-inferior to video-assisted laryngoscopy.
- The mean POGO scores for bed-up-head-elevated direct laryngoscopy was not significantly different from video-assisted laryngoscopy (80.14 +/- 22.03 and 86.45 +/-18.83 respectively), p= .073.
- Both video-assisted laryngoscopy and bed-up-head-elevated direct laryngoscopy provided better visualization of the glottis when compared to supine direct laryngoscopy.
- For video-assisted laryngoscopy, the mean POGO score increased from 55.80 +/- 30.54 (SD) to 86.45 +/- 18.83 when compared with baseline supine direct laryngoscopy.
- For bed-up-head-elevated direct laryngoscopy, the mean POGO score increased from 54.35 +/- 32.04 (SD) to 80.14 +/- 22.03 when compared with baseline supine direct laryngoscopy.
- Video-assisted laryngoscopy took an average of 8 seconds longer than bed-up-head-elevated direct laryngoscopy, as measured by time from the laryngoscope passes the teeth until the time end-tidal CO2 is detectable.
- There were no statistically significant differences between the groups in other secondary outcomes including number of intubation attempts, hypoxia, or esophageal intubation.
- Post-hoc subgroup analysis of the patients with a Cormack-Lehane score of 3 (patients in whom the epiglottis but not the glottic opening was visualized) found that both video-assisted laryngoscopy (n=11) and bed-up-head-elevated direct laryngoscopy (n=12) had better visualization of the glottis when compared to supine direct laryngoscopy. This was a very small subgroup of patients of patients who would traditionally be considered a difficult intubation, as 40 patients had already been screened out based on exclusion criteria before randomization.
Strengths:
- This was the first study to compare video-assisted laryngoscopy with bed-up-head-elevated laryngoscopy.
- Both groups had induction of anesthesia performed similarly.
- All investigators had >5 years of experience in the field of anesthesia and critical care.
- Investigators who evaluated laryngeal exposure in the baseline SSP were blinded to the laryngeal exposure in the treatment groups, and vice versa, by documenting the laryngeal exposure separately.
- The study used an intention-to-treat analysis, which reduces potential bias introduced by crossover and protocol violations. However, there was no crossover in this study, so a per protocol analysis would have resulted in the same findings.
- The patients in essence served as their own controls in assessing whether supine video-assisted laryngoscopy is better than supine direct laryngoscopy and whether bed-up-head-elevated direct laryngoscopy is better than supine direct laryngoscopy.
- Bonferroni correction was used to control for multiple comparisons for the superiority testing, which is a conservative method of controlling for multiple comparisons by in effect decreasing the level of significance based on the number of comparisons. However, this increases the likelihood of false negatives.
Limitations:
- The study was a non-inferiority study, which was perhaps not the right design. This is discussed further in the discussion section below.
- When registering the trial, the co-primary outcomes were POGO score and time-to-intubation. In the study writeup, the sole primary outcome was the POGO score, whereas the time-to-intubation was a secondary outcome. The Cormack-Lehane score was not mentioned when registering the trial, but was a secondary outcome in the writeup. Airway trauma was listed as a secondary outcome when registering the trial, but it was not mentioned in the results section. Given that the patients’ airways were manipulated twice, once for baseline supine laryngoscopy and once with the treatment method, this data would be particularly interesting.
- Only one person performed the intubations. The differences in POGO scores could have been because the two physicians who determined the baseline POGO scores were more generous with their scores that the physician who determined the POGO score during intubation. Additionally, individual familiarity with video-assisted laryngoscopy is a potential threat to external validity.
- This study was conducted in the operating room in patients undergoing anesthesia for elective surgeries, and the results may not be generalizable to the emergency department, e.g., in airways obstructed by blood or vomit, or other difficult airways.
- The study compared the hyperangulated video-assisted laryngoscopy blade with a traditional Macintosh blade. However, a comparison of a Macintosh blade in both groups would have perhaps been a better comparison due to eliminating differences in blade geometry.
Discussion:
- Non-inferiority studies are used to compare a standard therapy to a novel therapy because its characteristics would in some way be preferable given that both outcomes were equal (for example, the novel medication is cheaper than the standard medication). The non-inferiority design may have been chosen instead of a superiority trial because it had a higher probability of being statistically significant. The investigators addressed this by conducting superiority testing after conducting non-inferiority testing.
- The baseline characteristics of patients were not balanced. The bed-up-head-elevated group had a slightly higher mean BMI (26.24 vs 25.67), ASA class III (7.2% vs 2.9%), and Mallampati II patients (59.4% vs 52.2%) compared to video-assisted laryngoscopy group; however, despite these differences there was no real difference in baseline POGO scores at baseline between the video-assisted laryngoscopy and bed-up-head-elevated groups.
- A further direction of research that has not been published yet would be whether bed-up-head-elevated video-assisted laryngoscopy is better than supine video-assisted laryngoscopy, given that the biomechanics that make bed-up-head-elevated direct laryngoscopy preferable to supine laryngoscopy would presumably be the same.
Authors’ Conclusion:
“In the general population, BUHE intubation position provides a non-inferior laryngeal view to GLSC intubation. The laryngeal views obtained in both approaches were superior to the laryngeal view obtained in the sniffing position. In view of the many advantages of the BUHE position for intubation, the lack of proven adverse effects, the simplicity, and the cost-effectiveness, we propose that clinicians should consider the BUHE position as the standard intubation position for the general population.”
Clinical Take-Home Point:
Both video-assisted laryngoscopy and elevating the head of the bed with direct laryngoscopy can help improve visualization of the glottis during intubation.
References:
- Tsan et al. Comparison of Macintosh Laryngoscopy in Bed-up-Head-Elevated Position With GlideScope Laryngoscopy: A Randomized, Controlled, Noninferiority Trial. Anesth Analg. PMID: 31348051.
- Murphy DL et al. Inclined position is associated with improved first pass success and laryngoscopic view in prehospital endotracheal intubations. Am J Emerg Med. 2019. PMID: 30826211.
- Semler MW et al. A Multicenter, Randomized Trial of Ramped Position vs Sniffing Position During Endotracheal Intubation of Critically Ill Adults. Chest 2017. PMID: 28487139.
- Bhattacharjee S et al. A Comparison Between Video Laryngoscopy and Direct laryngoscopy for Endotracheal Intubation in the Emergency Department: A Meta-Analysis of Randomized Controlled Trials. J Clin Anesth 2018. PMID: 29549828
- Detsky ME, Jivraj N, Adhikari NK, et al. Will This Patient Be Difficult to Intubate?: The Rational Clinical Examination Systematic Review. JAMA 2019; 321:493. PMID: 30721300.
For More on This Topic Check Out:
- Journal Feed: Why Not Ramp All Intubations? New RCT Suggests We Should
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post Should Bed Up Head Elevated (BUHE) be the New Standard Position for RSI in the ED? appeared first on REBEL EM - Emergency Medicine Blog.
