 In part 1, we discussed that the ventilator can deliver 3 types of breaths: controlled, assisted or spontaneous breaths. These breaths can be delivered either by a set pressure or a set tidal volume. Then we closed with a discussion of the common ventilator modes, which is simply just combining all these types of breaths together.
In part 1, we discussed that the ventilator can deliver 3 types of breaths: controlled, assisted or spontaneous breaths. These breaths can be delivered either by a set pressure or a set tidal volume. Then we closed with a discussion of the common ventilator modes, which is simply just combining all these types of breaths together.
There are many aspects to consider in post-intubation management such as hemodynamic variations, analgesia & sedation, confirmation of the correct position of your endotracheal tube, and setting up the ventilator based on your patients physiology. Too often physicians pay little or no attention to how our amazing respiratory therapists set up the ventilator. Respiratory therapists have expertise in setting up, weaning and trouble-shooting the ventilator, but clinicians need to communicate important clinical physiologic information and their goals for their patient on mechanical ventilation. If you don’t feel comfortable setting up the ventilator at this point you at the very least need to communicate with your respiratory therapist when the ventilator is being set up.
Before we can start spinning dials on the ventilator, I think it’s important to discuss the goals of mechanical ventilation, the factors that control oxygenation and ventilation (removal of carbon dioxide), and in the next few parts we will discuss the 3 main physiologies we need to consider before we can set up the ventilator.
As both a pediatric and adult critical care physician, I will discuss some of the pediatric considerations for mechanical ventilation, but the concepts I will discuss throughout will apply to both pediatric and adult patients.
Goal of Mechanical Ventilation:
The ventilator is not a magical therapy that makes patients better, but simply a supportive therapy used until more definitive therapies have time to work. Lets consider the practical indications for intubation and mechanical ventilation: (1) refractory hypoxemia, (2) increased work of breathing (3) apnea/hypopnea leading to inadequate ventilation (4) inability to protect their airway.
So the goals of mechanical ventilation are simply to provide adequate (not perfect) oxygenation and ventilation, reduce our patient’s work of breathing, and to minimize the damage to the lung caused by the ventilator known as ventilator induced lung injury (VILI).
Oxygenation & Ventilation:
It has been classically taught that oxygenation is controlled by 2 main factors, PEEP or positive end expiratory pressure, and the fraction of inspired oxygen (fi02). Ventilation (removal of carbon dioxide) is also controlled by 2 main factors, tidal volume (Vt) and respiratory rate (RR). You can more simply say that ventilation is controlled by 1 factor, minute ventilation, which is simply the RR multiplied by Vt.
These facts are taught to help simplify the understanding of mechanical ventilation, but unfortunately can limit your understanding especially in grasping advanced modes or techniques specifically targeted to improve oxygenation in patients with Acute Respiratory Distress Syndrome (ARDS).
The truth is that the main determinants of oxygenation are your mean airway pressure (MAP) and fi02. Your mean airway pressure is the average pressure your lung is exposed to during mechanical ventilation both during inspiration and expiration. Mean airway pressure improves oxygenation by allowing the re-distribution of oxygen from highly compliant alveoli (more stretchy) too less compliant alveoli (stiffer).
When the ventilator delivers a breath, regardless of whether it’s a volume or pressure delivered breath, the mean airway pressure is increased and therefore improves oxygenation. Since oxygenation occurs by simple diffusion, it actually occurs throughout the respiratory cycle both during inspiration and expiration. It’s classically taught that the main factor besides fi02, controlling oxygenation is PEEP because our inspiratory to expiratory ratio (I:E) is typically 1:2 or 1:3 and therefore we spend more time in exhalation and at PEEP. Since more time is spent in exhalation, the expiratory pressure in the airways (PEEP) is more heavily weighted when calculating the mean airway pressure.
If this doesn’t make sense, think about another MAP that you are more familiar with, mean arterial pressure. Your ventricle spends more time in diastole than it does in systole, so your diastolic blood pressure is more heavily weighted when calculating the mean arterial blood pressure. The systolic blood pressure is higher than the diastolic blood pressure, but your higher systolic blood pressure is maintained for much less time than your lower diastolic blood pressure. As a result, your mean arterial blood pressure is closer to your diastolic blood pressure.
To understand this analogy, you must think of ventricular systole, where the ventricle achieves a higher pressure (compared to diastolic pressure) for a shorter time (compared to diastolic time) similar to inspiration where your airway pressure is high (compared to your expiratory pressure/PEEP) but again, only stays high for a short period of time (compared to your time to expire). So our higher inspiratory pressure is maintained for a shorter period time compared to our lower expiratory pressure (PEEP), then our mean airway pressure is closer to the PEEP.
So why take the time to explain this? There are some ventilator maneuvers you can perform to increase oxygenation other than simply increase the fi02 and the PEEP. You can increase the inspiratory pressure and therefore increase the MAP, but that may cause barotrauma (high pressures that cause VILI) in the lungs and not the best idea. The other maneuver is to increase the inspiratory time, increasing the time at this higher inspiratory pressure (increased MAP) and helping to redistribute gas flow throughout the lungs and therefore improve oxygenation.
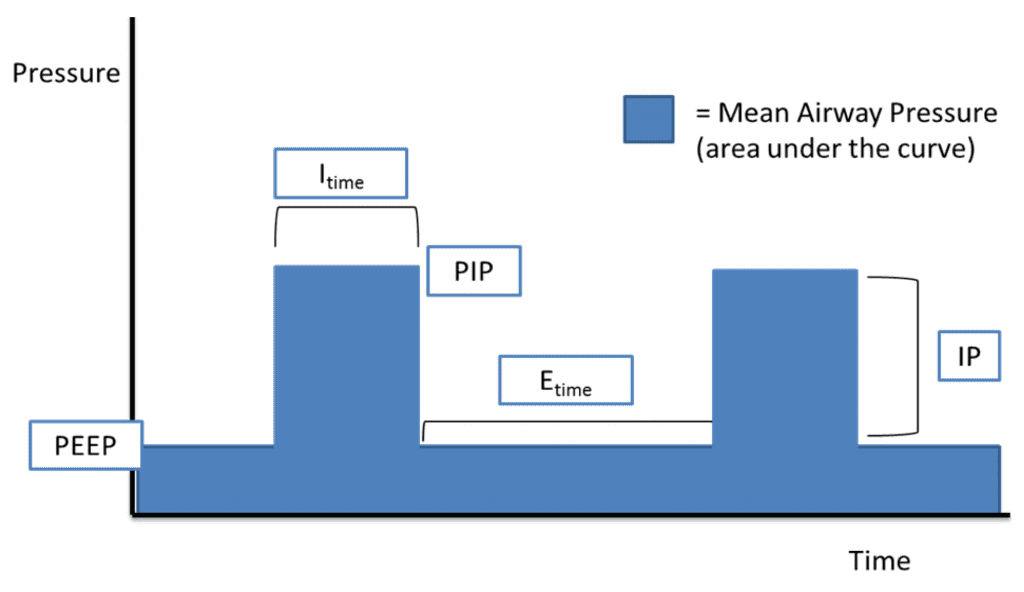 Figure 1: Mean Airway Pressure (Image from Kevin Kuo, MD – Link is HERE)
Figure 1: Mean Airway Pressure (Image from Kevin Kuo, MD – Link is HERE)
You can actually lengthen the inspiratory time and maintain this higher inspiratory Pressure for longer periods of time to improve oxygenation. In fact, you can lengthen the inspiratory time to be equal to the expiratory time, which is called inverse ratio ventilation (IRV) a maneuver used in ARDS to improve oxygenation. Another advanced mode, which we haven’t discussed yet, is airway pressure release ventilation (APRV), which delivers higher pressures (P-High) for a longer time (T-High) with very short pauses (T-Low) at low pressure (P-Low) to help exhale carbon dioxide. These are more advanced techniques and modes to improve oxygenation.
PEEP, or optimal PEEP, is highly important for many reasons other than just increasing mean airway pressure. Setting PEEP optimally is important so that during expiration your alveoli do not collapse (atelectasis) which will help maintain adequate alveolar surface area for oxygen diffusion to continue. Also, optimal PEEP will prevent higher pressures from being delivered from the ventilator to have to re-open closed alveoli.
Recall, during part 1, we compared our lungs to a balloon and described how hard it is to initially start blowing up a balloon, but once you expand that balloon it take a lot less pressure to inflate that balloon after this initial phase. We used this to discuss the concept of airway resistance and PIP, but here I want you to think about it in the context of inadequate PEEP and atelectasis. If you are going to breath air in and out of a balloon over and over, it will make your life easier if you do not let the balloon completely deflate. If the balloon completes deflates in between breaths, then you will have to blow harder each time you attempt to re-inflate the balloon. The key is to keep some air in the balloon, keeping the balloon partial inflated, and then you will save energy, as you don’t have to overcome that initial resistance each time.
Now imagine you let your alveoli completely collapse between breaths (inadequate PEEP), this will not allow for adequate oxygenation during expiration and you have give more pressure just to open the alveoli let alone then expand the lung. This repetitive opening and closing of the alveoli will lead to shear stress or atelectotrauma (another form of VILI) and can worsen the patient’s lung injury.
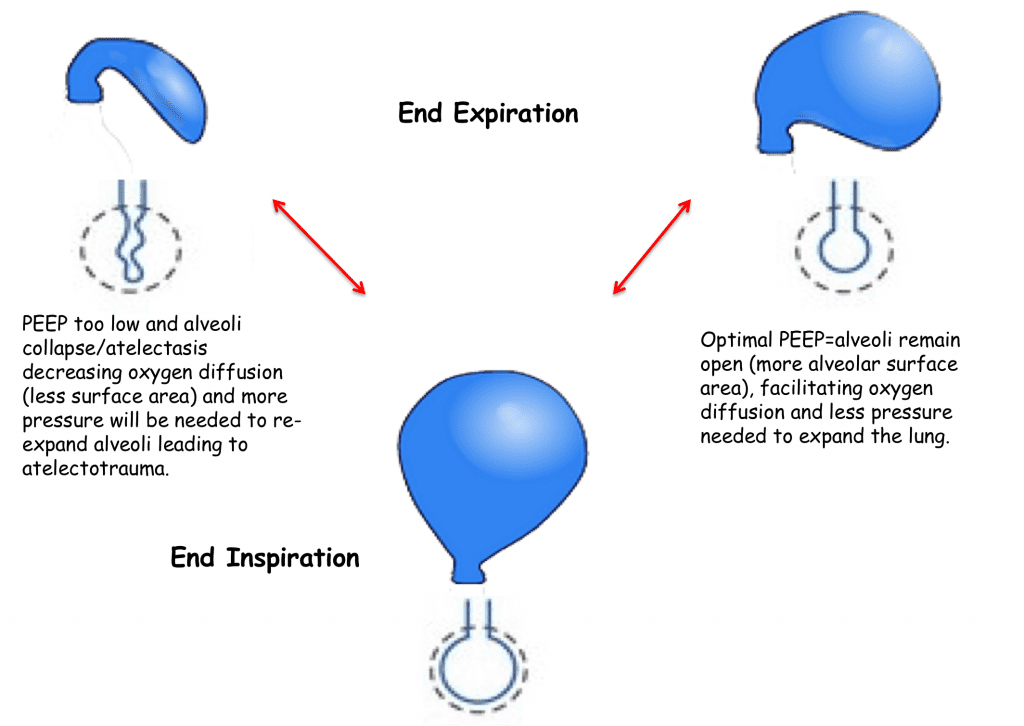
Figure 2: Optimal PEEP
For More on this Topic Checkout:
- Frank Lodeserto at REBEL EM: Simplifying Mechanical Ventilation – Part I
- Frank Lodeserto at REBEL EM: Simplifying Mechanical Ventilation Part 2 – Goals of Mechanical Ventilation & Factors Controlling Oxygenation and Ventilation
- Frank Lodeserto at REBEL EM: Simplifying Mechanical Ventilation Part 3 – Severe Metabolic Acidosis
- Frank Lodeserto at REBEL EM: Simplifying Mechanical Ventilation Part 4 – Obstructive Physiology
- Frank Lodeserto at REBEL EM: Simplifying Mechanical Ventilation Part 5 – Refractory Hypoxemia & APRV
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
Support the Show by Paying & Claiming 1.5hrs (Parts 1 – 5) of CME/CEH by Clicking on the Logo Below
The post Simplifying Mechanical Ventilation – Part 2: Goals of Mechanical Ventilation & Factors Controlling Oxygenation and Ventilation appeared first on REBEL EM - Emergency Medicine Blog.