 Before I set up the ventilator, I consider if my patient has one of the following 3 physiologic processes: severe metabolic acidosis, an obstructive process (Asthma or COPD), or refractory hypoxemia. If my patient doesn’t fit into one of these 3 categories then I will default to placing them in the refractory hypoxemia category (Part 5), which is simply a lung protective strategy that will be appropriate for patients. In this part we will discuss setting up your ventilator for the patient with a severe metabolic acidosis.
Before I set up the ventilator, I consider if my patient has one of the following 3 physiologic processes: severe metabolic acidosis, an obstructive process (Asthma or COPD), or refractory hypoxemia. If my patient doesn’t fit into one of these 3 categories then I will default to placing them in the refractory hypoxemia category (Part 5), which is simply a lung protective strategy that will be appropriate for patients. In this part we will discuss setting up your ventilator for the patient with a severe metabolic acidosis.
Severe Metabolic Acidosis:
Patients with severe metabolic acidosis such as DKA (who we try to never intubate, but occasionally are forced to do so), ingestions (ie Aspirin overdose), or renal failure among others are trying to compensate by maintaining extremely high minute ventilations. These patients may develop inability to protect their airways, increased work of breathing, or start to inadequately compensate. When we paralyze and sedate these patients for intubation, the ability for these patients to now compensate for their severe metabolic acidosis is now our responsibility.
Too often, I observe physicians successfully intubate, but then never communicate the underlying physiology to the respiratory therapist or get so focused on the procedure itself and forget what’s happening to the patient afterwards. The concern is that ventilator will be set up with a “normal” minute ventilation, but much too low for your patient to adequately compensate which may lead to a cardiac arrest.
In these patients, I have to try and match the patient’s minute ventilation before I intubated them as well as compensate for the apnea time during intubation that potentially causes an increase in CO2 which is a major challenge. Here is when I typically break out my acid-base physiology equations and calculate my goal PaCO2 in order to help my patient compensate adequately. There is a reason we learned winter’s equation in medical school!
Winter’s Equation (Goal C02) = 1.5 X HCO3 (Taken from the BMP) + 8 (+/- 2)
Winter’s equation tells you what your goal PaCO2 should be if your patient is adequately compensating for their metabolic acidosis. If you calculate their goal PaCO2 to be 20 mm Hg based on winter’s equation and your blood gas returns back showing a PaCO2 of 30 mm Hg then your patient is inadequately compensating. They have a combined metabolic acidosis (remember you are only doing winters equation when you have a metabolic acidosis) and now a respiratory acidosis as they are retaining too much carbon dioxide. Always think of carbon dioxide as an acid, so if you’re retaining too much acid (carbon dioxide) then your respiratory system is not compensating and this would be a combined respiratory acidosis. If you calculate your patients PaCO2 based on winter’s equation to be 30 mm Hg and your blood gas returns with PaCO2 20 mm Hg then your patient has a combined respiratory alkalosis. You shouldn’t say, my patient is just amazing and doing a bit extra because they are awesome. They are blowing off too much acid (carbon dioxide) and this is pathologic and abnormal.
Once I figure out what my goal PaCO2 level should be then I set up the minute Ventilation according to a rough calculation I was taught as a fellow.
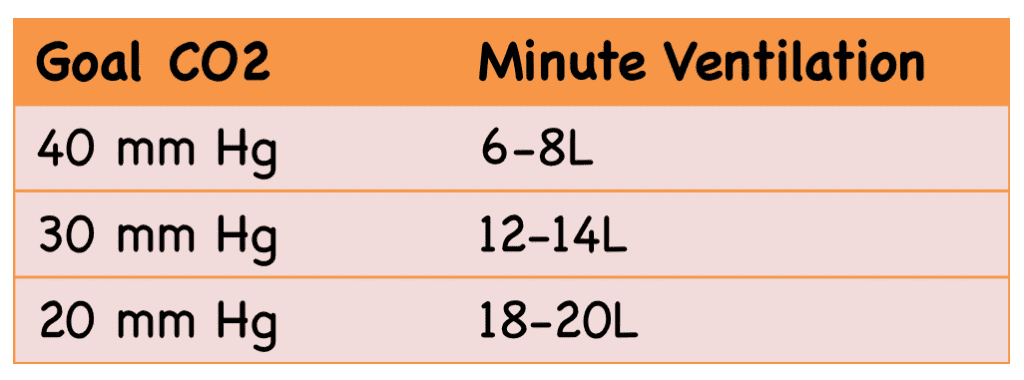
Table 1: Target minute ventilation to achieve a goal PaCO2 for adult patients.
Table 1 gives me a rough estimate of what I think my patient’s minute ventilation should be and this will usually be a good starting point for setting up my ventilator. However 20-30 minutes after intubation I get a blood gas to check my acid-base status, specifically checking my pH (Goal >7.25 – <7.45). Most of the time I come pretty close using this table, but I will then calculate my goal minute ventilation using equation below and re-adjust the minute ventilation set on the ventilator to achieve my goal.
Goal Minute Ventilation = [PaCO2 (from blood gas) x Minute Ventilation (Set on Vent)]/[Desired CO2 (Calculated from Winters Equation)]
For More on this Topic Checkout:
- Frank Lodeserto at REBEL EM: Simplifying Mechanical Ventilation – Part I
- Frank Lodeserto at REBEL EM: Simplifying Mechanical Ventilation Part 2 – Goals of Mechanical Ventilation & Factors Controlling Oxygenation and Ventilation
- Frank Lodeserto at REBEL EM: Simplifying Mechanical Ventilation Part 3 – Severe Metabolic Acidosis
- Frank Lodeserto at REBEL EM: Simplifying Mechanical Ventilation Part 4 – Obstructive Physiology
- Frank Lodeserto at REBEL EM: Simplifying Mechanical Ventilation Part 5 – Refractory Hypoxemia & APRV
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
Support the Show by Paying & Claiming 1.5hrs (Parts 1 – 5) of CME/CEH by Clicking on the Logo Below
The post Simplifying Mechanical Ventilation – Part 3: Severe Metabolic Acidosis appeared first on REBEL EM - Emergency Medicine Blog.