
 Background: Spontaneous coronary artery dissection (SCAD), once thought of as a rare “zebra” diagnosis that was universally fatal, is now being increasingly recognized as a cause of acute coronary syndrome (ACS), particularly in women due to increased vigilance, greater utilization of coronary angiography and advanced imaging. Despite these advances, SCAD still remains one of the most enigmatic syndromes in cardiology. It carries a high misdiagnosis and mistreatment rate with lack of consensus on investigation or treatment. Here we review the salient features of SCAD to increase awareness of this disease entity and further our understanding of this unique disease process.
Background: Spontaneous coronary artery dissection (SCAD), once thought of as a rare “zebra” diagnosis that was universally fatal, is now being increasingly recognized as a cause of acute coronary syndrome (ACS), particularly in women due to increased vigilance, greater utilization of coronary angiography and advanced imaging. Despite these advances, SCAD still remains one of the most enigmatic syndromes in cardiology. It carries a high misdiagnosis and mistreatment rate with lack of consensus on investigation or treatment. Here we review the salient features of SCAD to increase awareness of this disease entity and further our understanding of this unique disease process.
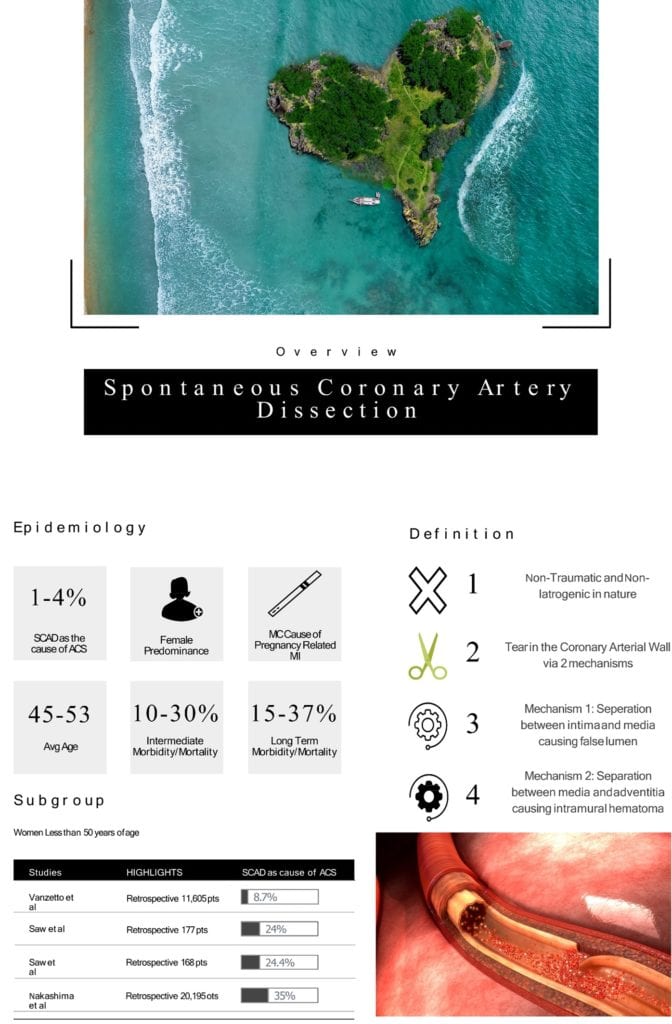 Definition: SCAD is defined as a non-traumatic and non-iatrogenic tear in the coronary arterial wall. This may manifest as either separation between the intima and media or the media and adventitia of the coronary arterial wall. These mechanisms lead to formation of either a false lumen or an intramural hematoma resulting in compromised coronary blood flow and myocardial infarction (MI) (Hayes 2018, Janssen 2019).
Definition: SCAD is defined as a non-traumatic and non-iatrogenic tear in the coronary arterial wall. This may manifest as either separation between the intima and media or the media and adventitia of the coronary arterial wall. These mechanisms lead to formation of either a false lumen or an intramural hematoma resulting in compromised coronary blood flow and myocardial infarction (MI) (Hayes 2018, Janssen 2019).
Epidemiology: True incidence and prevalence is unknown and has been historically underestimated.
Incidence: It has been suggested that SCAD may be the cause up to 1 – 4% of ACS cases overall (Hayes 2018).
- It is most common among women typically lacking classic cardiac disease risk factors.
- Highest incidence is within the subgroup of women less than 50 years of age, ranging from 8.7% to 35% (Yang 2020, Vanzetto 2009, Saw 2014, Hayes 2018, Nakashima 2016).
- SCAD has also been identified as the most common cause of pregnancy-associated MI (Hayes 2018).
Age: Average age ranges from 45 to 53 years of age (Hayes 2018).
Gender: Clear female to male predominance is seen in SCAD.
Morbidity/Mortality: High rates of intermediate, long term, and 10-year major adverse cardiac events and recurrent MI (Hayes 2018).
Poor Prognostic Factors:
- Identification of poor prognostic factors or risk factors is difficult due to small sample sizes of studies (see overview graphic).
- Severe anatomical coronary tortuosity has been identified as the only risk factor for recurrence (Hayes 2018).
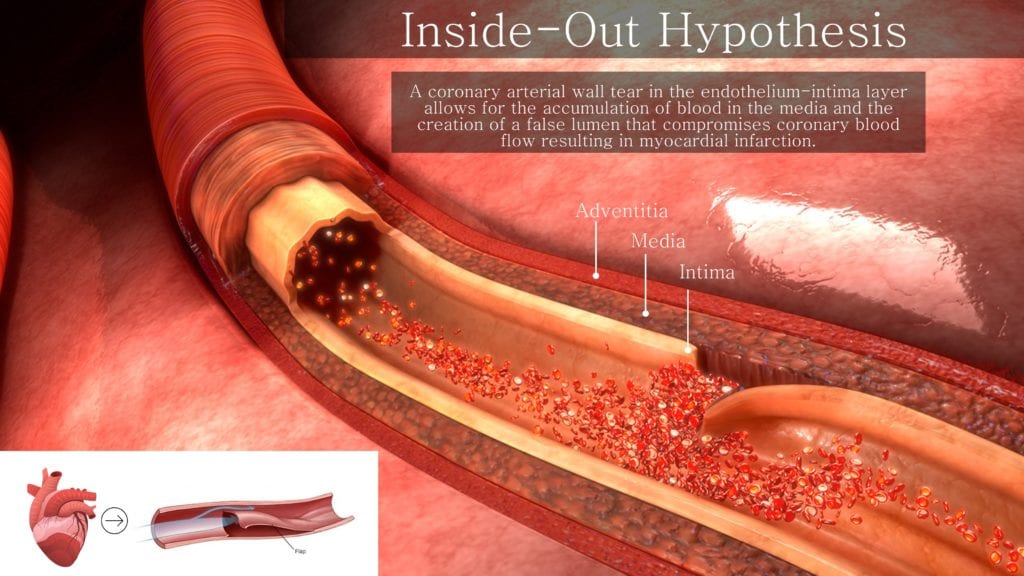
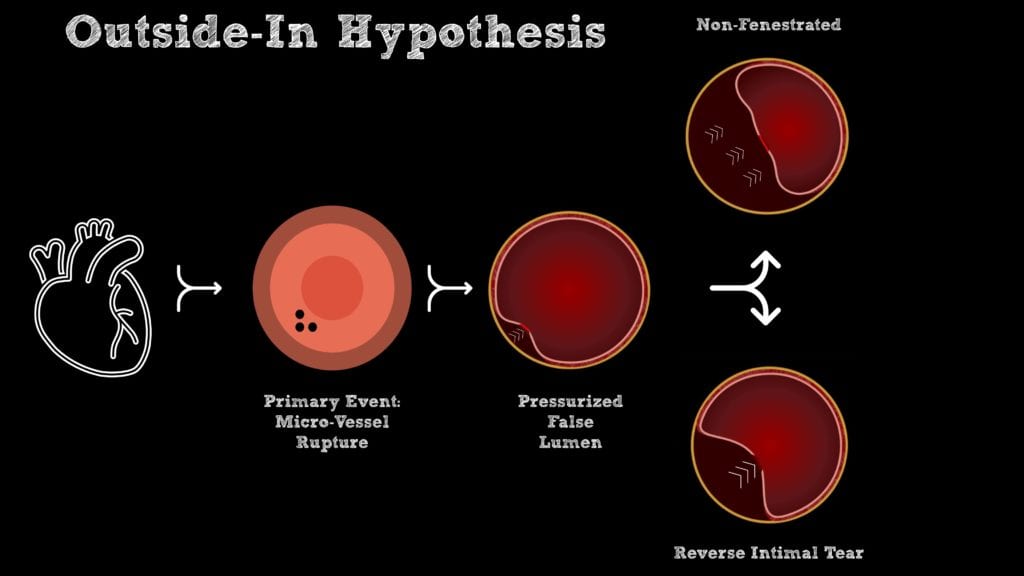
Pathogenesis: The true pathophysiology of SCAD is still being elucidated but two principle mechanisms have been proposed:
-
Inside-Out Hypothesis:
- A coronary arterial wall tear in the endothelium-intima layer allows for the creation of a false lumen that compromises coronary blood flow (Jackson 2019).
-
Outside-in Hypothesis:
- A primary event outside the intima leads to expanding intramural hemorrhage and creation of a false lumen that that compromised coronary blood flow (Jackson 2019).
- Two potential phenomena may manifest at this juncture:
- Rupture of the intima-media membrane creates fenestrations, allowing for pressure equalization between the true and false lumen (Jackson 2019).
- In the absence of fenestrations, the pressurized false lumen continues to compromise blood flow in the true lumen (Jackson 2019).
History and Physical:
 Risk Factors: SCAD has a unique demographic, risk factor profile and women are at greater risk.
Risk Factors: SCAD has a unique demographic, risk factor profile and women are at greater risk.
-
Fibromuscular Dysplasia (FMD): A non-inflammatory and non-atherosclerotic vascular disorder that affects arterial walls, manifesting as stenosis, aneurysms, tortuosity, or dissection (Hayes 2018).
- FMD is the most common extra-coronary vascular abnormality in patients with SCAD.
-
Pregnancy: Pregnancy-associated SCAD is the most common cause of MI among pregnant and postpartum patients (Hayes 2018, Elkayam 2014).
- Majority of SCAD occurs in the third trimester or early post-partum period.
-
Systemic Inflammatory Disorders: Case reports have attributed systemic inflammatory disorders, autoimmune, and rheumatologic disease with SCAD.
- These may not be a true association as case reports and small series did not control for the prevalence of these conditions in the general population.
- Inherited Arteriopathies and Connective Tissue Disorders: An infrequent cause of SCAD.
Precipitating Factors: Although not present in all patients with SCAD, there appears to be a link between certain potential triggers and precipitants that may initiate spontaneous intimal tears or mediate intramural hematoma formation (Hayes 2018).
-
Extreme Physical or Emotional Stress: The most commonly reported precipitants before the patient’s SCAD event.
- Intense Exercise
- Intense Emotional Stress
- Valsalva Activities
- Recreational Drugs (Cocaine, Amphetamines)
-
Hormone-Mediated Triggers: These triggers have less supportive data, but associations have been reported in the literature (Hayes 2018).
- Oral Contraceptive Pills
- Postmenopausal Hormone Therapy
- Infertility Treatment
- High-Dose Corticosteroid Administration
Symptoms/Physical Examination: Patients present with symptoms and physical examination that are consistent with ACS and frequently exhibit increased levels of cardiac enzymes (Hayes 2018).
Diagnosis:
- Diagnosis is difficult and patients may be mistakenly discharged or have an incomplete work-up done due to their relatively young age and lack of risk factors for ACS.
- Accurate diagnosis in the acute stages of ACS is paramount as the management and investigation of SCAD is different from other causes of ACS (Hayes 2018).
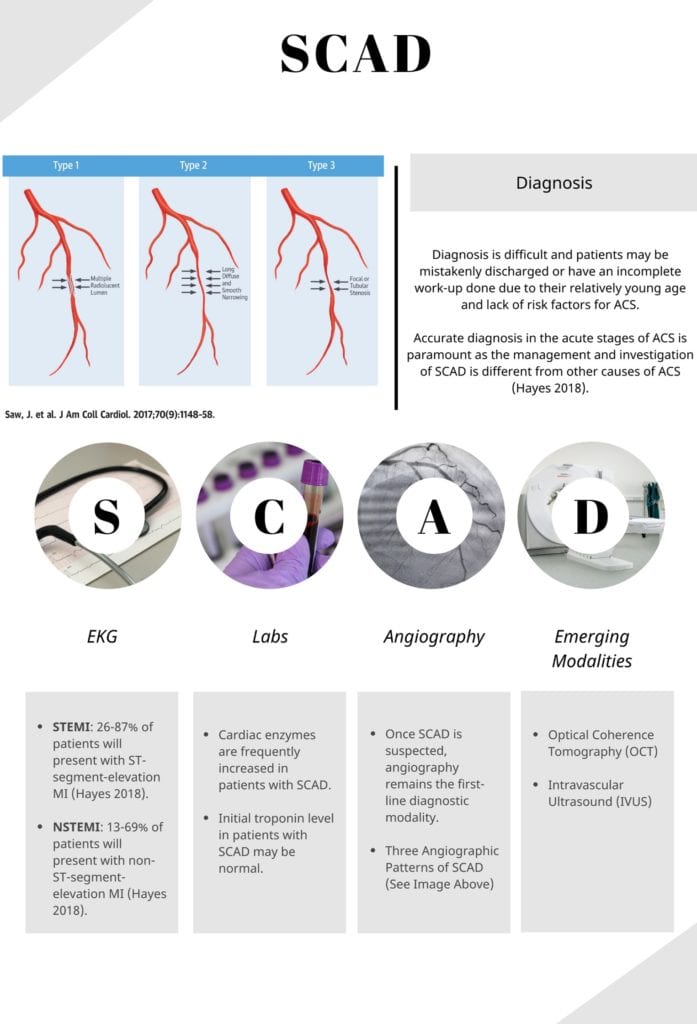 EKG: A normal EKG does not rule out SCAD, but EKGs are typically consistent with STEMI or NSTEMI.
EKG: A normal EKG does not rule out SCAD, but EKGs are typically consistent with STEMI or NSTEMI.
- STEMI: Distribution of ST-Segment changes will correspond to dissecting coronary artery.
- LAD is the most commonly involved vessel in SCAD: Thus, look for convex ST-segment elevations in the anterior leads
- NSTEMI: Transient ST elevation, ST depression, new T wave inversions, or other EKG changes with elevations in cardiac enzymes.
Labs: Cardiac enzymes are frequently increased in patients with SCAD.
- Initial troponin level in patients with SCAD may be normal.
- Other labs are drawn to assist inpatient management and rule out other etiologies
- CBC, CMP, Coagulation Panel, HCG
- Autoimmune Workup, Inherited Arteriopathies and Connective Tissue Disorders Workup
Cardiac Diagnostics:
- Coronary Angiography: Once SCAD is suspected, angiography remains the first-line diagnostic modality.
- Most commonly involved vessels: Left Anterior Descending > Left Circumflex > Right Coronary Artery (Yang 2020).
- Three Angiographic Patterns of SCAD (Yang 2020):
- Type 1: Multiple visualized lumens within the arterial wall along with extraluminal contrast staining
- Type 2: Most commonly seen and can be missed on angiography. Arterial caliber is noted to have areas of long, diffuse narrowing
- Type 3: Visualization of focal or tubular stenosis of the involved artery
- Limitation:
- Does not image the arterial wall in great detail and carries a higher risk of catheter-induced coronary artery dissection in patients with SCAD due to underlying arterial fragility.
- Intracoronary Imaging: Provide detailed visualization and aids in diagnosis of SCAD but have additional risks, costs, and availability drawbacks.
- Optical Coherence Tomography (OCT): Allows for detailed coronary arterial wall visualization.
- Intravascular Ultrasound (IVUS): Excellent spatial resolution for coronary arterial wall visualization.
- Coronary Computed Tomography Angiography (CCTA):
- Role of CCTA in SCAD has not been adequately studied at this time.
- Not recommended as first-line for diagnosis of SCAD.
Management:
-
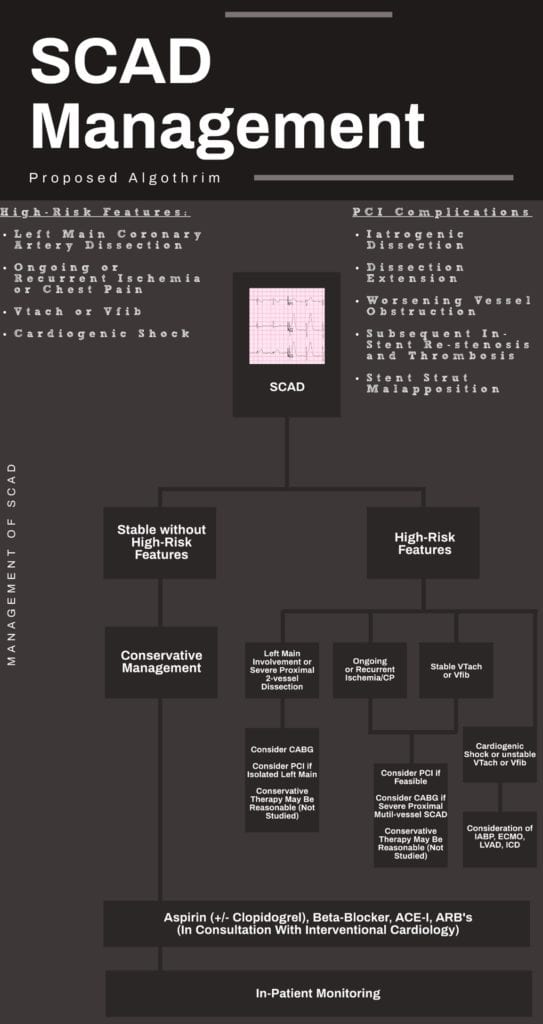 Conservative Management: Mainstay of management in those without high-risk features.
Conservative Management: Mainstay of management in those without high-risk features.
- Majority of patients have angiographic healing of SCAD lesions without intervention.
- Conservatively managed patients who have recurrent MI may require emergency revascularization.
- Medical Therapy:
- Dual-Antiplatelet Therapy (Hayes 2018, Amsterdam 2014):
- Patients with SCAD who undergo revascularization should receive dual-antiplatelet therapy
- Evidence for dual-antiplatelet therapy for SCAD patient who do not undergo coronary intervention is currently lacking.
- Expert opinion currently is to recommend dual-antiplatelet therapy for at least 1 year after occurrence of SCAD and lifelong aspirin.
- Beta-Blockers (Hayes 2018):
- Recommended in SCAD patients with evidence of HTN, arrhythmias, or LV dysfunction.
- Expert opinion advocates for use of beta-blockers after selecting out those at risk for adverse effects.
- Angiotensin-Converting Enzyme Inhibitors and Angiotensin Receptor Blockers (Hayes 2018):
- Should be considered if LV systolic dysfunction is noted.
- Concern for teratogenicity in female patients of reproductive age.
- Anticoagulation (Hayes 2018, Yip 2015):
- If systemic anticoagulation is started at initial presentation, consideration for discontinuation is reasonable once SCAD is diagnosed based on expert opinion.
- Statins:
- Not routinely recommended after SCAD.
- SCAD patients with high-risk features:
- High-Risk Features (Yang 2020, Saw 2016):
- Left Main Coronary Artery Dissection
- Ongoing or Recurrent Ischemia or Chest Pain
- Ventricular Tachycardia or Ventricular Fibrillation
- Cardiogenic Shock
- High-Risk Features (Yang 2020, Saw 2016):
- Dual-Antiplatelet Therapy (Hayes 2018, Amsterdam 2014):
- Majority of patients have angiographic healing of SCAD lesions without intervention.
- Percutaneous Coronary Intervention (PCI) or Coronary Artery Bypass Grafting (CABG) should be considered (Hayes 2018).
- PCI: Due to coronary artery fragility observed in SCAD, PCI is associated with increased risk of complications and variables outcomes.
- CABG: Described for SCAD patients with left main or proximal dissection, those with failure of attempted PCI, and those with refractory ischemia despite conservative approach (Hayes 2018).
Guest Post By:
Muhammad Durrani, DO, MS
Assistant Clerkship Director, Assistant Research Director
Inspira Medical Center Emergency Department
Vineland, NJ
Twitter: @IbbyDurrani
References:
- Hayes S et al. Spontaneous Coronary Artery Dissection: Current State of the Science: A Scientific Statement From the American Heart Association. Circulation. 2018. PMID: 29472380
- Janssen E et al. Spontaneous coronary artery dissections and associated predisposing factors: a narrative review. Neth Heart J. 2019. PMID: 30684142
- Yang C et al. Spontaneous Coronary Artery Dissection: Latest Developments and New Frontiers. Curr Atheroscler Rep. 2020. PMID: 32734349
- Vanzetto G et al. Prevalence, therapeutic management and medium-term prognosis of spontaneous coronary artery dissection: results from a database of 11,605 patients. Eur J Cardiothorac Surg. 2009. PMID: 19046896
- Saw J et al. Spontaneous coronary artery dissection: association with predisposing arteriopathies and precipitating stressors and cardiovascular outcomes. Circ Cardiovasc Interv. 2014. PMID: 25294399
- Saw J et al. Nonatherosclerotic coronary artery disease in young women. Can J Cardiol. 2014. PMID: 24726091
- Nakashima T et al. Prognostic impact of spontaneous coronary artery dissection in young female patients with acute myocardial infarction: A report from the Angina Pectoris-Myocardial Infarction Multicenter Investigators in Japan. Int J Cardiol. 2016. PMID: 26820364
- Jackson R et al. Spontaneous Coronary Artery Dissection: Pathophysiological Insights From Optical Coherence Tomography. JACC Cardiovasc Imaging. 2019. PMID: 30878439
- Saw J et al. Spontaneous coronary artery dissection: prevalence of predisposing conditions including fibromuscular dysplasia in a tertiary center cohort. JACC Cardiovasc Interv. 2013. PMID: 23266235
- Rogowski S et al. Spontaneous Coronary Artery Dissection: Angiographic Follow-Up and Long-Term Clinical Outcome in a Predominantly Medically Treated Population. Catheter Cardiovasc Interv. 2017. PMID: 26708825
- Prasad M, Tweet MS, Hayes SN, et al. Prevalence of extracoronary vascular abnormalities and fibromuscular dysplasia in patients with spontaneous coronary artery dissection. Am J Cardiol. 2015. PMID: 25929580
- Elkayam U et al. Pregnancy-associated acute myocardial infarction: a review of contemporary experience in 150 cases between 2006 and 2011. Circulation. 2014. PMID: 24753549
- Tweet M et al. Clinical features, management, and prognosis of spontaneous coronary artery dissection. Circulation. 2012. PMID: 22800851
- Lindor R et al. Emergency Department Presentation of Patients with Spontaneous Coronary Artery Dissection. J Emerg Med. 2017. PMID: 27727035
- Prakash R et al. Catheter-Induced Iatrogenic Coronary Artery Dissection in Patients With Spontaneous Coronary Artery Dissection. JACC Cardiovasc Interv. 2016. PMID: 27609262
- Awadalla H et al. Catheter-induced left main dissection incidence, predisposition and therapeutic strategies experience from two sides of the hemisphere. J Invasive Cardiol. 2005. PMID: 15831980
- Saw J et al. Contemporary Review on Spontaneous Coronary Artery Dissection. J Am Coll Cardiol. 2016. PMID: 27417009
- Tweet M et al. Spontaneous coronary artery dissection: revascularization versus conservative therapy. Circ Cardiovasc Interv. 2014. PMID: 25406203
- Lettieri C et al. Management and Long-Term Prognosis of Spontaneous Coronary Artery Dissection. Am J Cardiol. 2015. PMID: 25937347
- Yip A et al. Spontaneous coronary artery dissection-A review. Cardiovasc Diagn Ther. 2015. PMID: 25774346
- Amsterdam E et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014. PMID: 25249586
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami) and Salim R. Rezaie, MD (Twitter: @srrezaie)
The post Spontaneous Coronary Artery Dissection (SCAD) appeared first on REBEL EM - Emergency Medicine Blog.
