
 Background: In 2002, the New England Journal of Medicine published two studies that changed the management of post-cardiac arrest patients by showing improved outcomes in patients treated with therapeutic hypothermia (32°C-34°C) for at least 24 hours. (Bernard 2002, Hypothermia 2002). The landscape changed again in 2013 with the publication of the Targeted Temperature Management (TTM) trial in the New England Journal, which compared post-cardiac arrest hypothermia at 32-34°C and at 36°C and found no difference in outcomes (Nielson 2013). After the publication of the TTM trial, many hospitals changed their cooling protocols to a target temperature of 36°C, however, recently it has been shown that this may pose an increased risk of fever. (Cassamento 2016).
Background: In 2002, the New England Journal of Medicine published two studies that changed the management of post-cardiac arrest patients by showing improved outcomes in patients treated with therapeutic hypothermia (32°C-34°C) for at least 24 hours. (Bernard 2002, Hypothermia 2002). The landscape changed again in 2013 with the publication of the Targeted Temperature Management (TTM) trial in the New England Journal, which compared post-cardiac arrest hypothermia at 32-34°C and at 36°C and found no difference in outcomes (Nielson 2013). After the publication of the TTM trial, many hospitals changed their cooling protocols to a target temperature of 36°C, however, recently it has been shown that this may pose an increased risk of fever. (Cassamento 2016).
Clinical Question:
What is the impact of changing the target temperature post-ROSC from 33°C to 36°C?
Population:
Patients with non-traumatic ventricular fibrillation out-of-hospital cardiac arrest during the study period.
Outcome:
This was a descriptive paper that did not define a primary outcome. Rather, it made numerous comparisons between the treatments received, complications, temperatures and outcomes of patients in two different target temperature groups. The following are some of the comparisons made:
Design:
Retrospective, single center study
Excluded:
- Traumatic cardiac arrest
- Cardiac arrest with initial rhythm other than ventricular fibrillation
Primary Results:
- 76 patients with ventricular fibrillation out-of-hospital cardiac arrest included
- 24 patients in the 33°C period
- 52 patients in the 36°C period
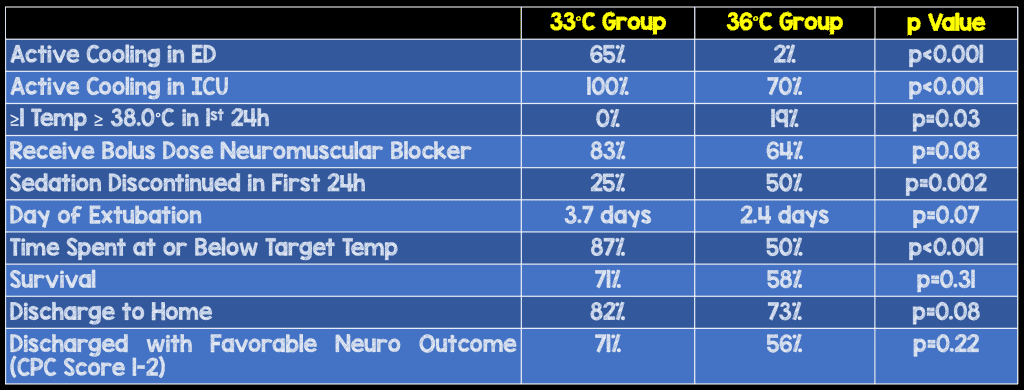
- Active cooling more likely started in ED during 33°C period. (65% vs. 2%, p<0.001)
- All patients in 33°C period received active cooling in the ICU compared to 70% in the 36°C period (p<0.001)
Critical Results:
- Patients in the 36°C target temperature group were more likely to have at least one temperature recording ≥ 38.0°C in the first 24 hours (0% vs. 19%, p = 0.03)
- Patients in the 36°C target temperature group spent significantly less time at or below target temperature (87% vs. 50%, p<0.001)
- Non-significant trend towards decrease in patient survival in the 36°C temperature group (71% vs. 58%, p = 0.31)
- Non-significant trend towards decrease proportion of patients discharged to home in the 36°C temperature group (82% vs. 73%, p = 0.08)
- Non-significant trend towards decrease proportion of patients discharged with a favorable neurological outcome in the 36°C temperature group (CPC score 1-2: 71% vs. 56%, p = 0.22)
Strengths:
- Consecutive enrollment
- Asks an important clinical question regarding the consequence of a change in protocol
Limitations:
- Retrospective, single center study
- Small sample size
- Compliance at 36°C temperature group seems less rigorous so the results may be due to poor compliance with the target, rather than the higher target temperature itself
- As this was a descriptive paper, the investigators looked at numerous variables between the two groups rather than identifying specific outcomes before starting their analysis. This could potentially have impacted the variables they chose to investigate and report.
Author’s Conclusions:
“After the change from TTM target of 33°C to 36°C, we report a low compliance target temperature, higher rates of fever, and a trend towards clinical worsening in patients outcomes. Hospitals adopting a 36°C target temperature need to be aware that this target may not be easy to achieve, and requires adequate sedation and muscle-relaxant to avoid fever.”
Our Conclusions:
A higher target temperature may, in of itself, be no worse for patient outcomes. However, it may encourage decreased compliance, higher rates of fever and potentially worsened patient outcomes.
Potential Impact to Current Practice:
Targeting a higher temperature for cooling post VF-OHCA is logistically difficult to implement. When targeting the higher hypothermia temperature, patients may need interventions such as sedation and paralysis to meet even the higher target temperature.
Clinical Bottom Line:
While it does not appear that a post-ROSC target of 33 degrees is superior to 36 degrees in VF-OHCA, it appears that maintaining 36 degrees is more difficult than maintaining 33 degrees. This should be taken into account when shaping a protocol. Whatever your hospital’s target temperature policy may be, act aggresively to reach and maintain the temperature
For More on This Topic Checkout:
- Ken Milne at The SGEM: SGEM #183 – Don’t RINSE, Don’t Repeat
References:
- Bernard SA et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med 2002;346:557-63. PMID 11856794
- Bray et al. Changing target temperature from 33°C to 36°C in the ICU management of out-of-hospital cardiac arrest: A before and after study. Resuscitation. 2017 Apr;113:39-43. PMID 28159575
- Casamento A et al. A comparison of therapeutic hypothermia and strict therapeutic normothermia after cardiac arrest. Resuscitation 2016;106:83-88. PMID 27350372
- Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med 2002;346:549-56. PMID 11856793
- Nielsen N et al. Targeted temperature management at 33 degrees C versus 36 degrees C after cardiac arrest. N Engl J Med 2013; 369: 2197-206. PMID 24237006
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami) and Salim Rezaie (Twitter: @srrezaie)
The post Targeted Temperature Management in Out-of-Hospital Cardiac Arrest: 33°C or 36°C? appeared first on REBEL EM - Emergency Medicine Blog.
