
 EMS rolls in with a 28 year-old male brought in for severe agitation after being found smashing glass bottles in the street. As police approached him, he cut himself with the broken glass and was bleeding significantly, though they could not fully evaluate his wounds due to his agitation. He was restrained by 6 officers and brought to you without IV access. He is thrashing around on the gurney in 4-point restraints, with blood soaking through the gauze bandages on his arms. What do you do?
EMS rolls in with a 28 year-old male brought in for severe agitation after being found smashing glass bottles in the street. As police approached him, he cut himself with the broken glass and was bleeding significantly, though they could not fully evaluate his wounds due to his agitation. He was restrained by 6 officers and brought to you without IV access. He is thrashing around on the gurney in 4-point restraints, with blood soaking through the gauze bandages on his arms. What do you do?
Excited Delirium Syndrome:
Best defined as “delirium associated with excited behavior or agitation.”[1] it is a dangerous, high‐morbidity, and high‐mortality condition that requires immediate and aggressive management.
No single comparative study has been performed to conclude whether one treatment approach is preferable to another in the management of excited delirium. Because patients with excited delirium can develop hyperthermia, hypoxia, acidosis, hypovolemia, rhabdomyolysis, hyperkalemia, traumatic injuries (including intracranial), seizures, coma, and death, the need for sedation to rapidly gain control of the patient is paramount. When the patient is covered in a spit-mask, with 900lbs of security guards holding him down, every minute that the patient is uncontrolled can lead to increased temperature, worsening acidosis, worsening of traumatic injuries, and progression toward seizure, coma, or death.
Benzodiazepines and antipsychotics such as haloperidol, the most commonly used sedative agents, have limitations including slow onset, respiratory depression, and variability in clinical response.[2-3] As such, there is a need for a rapid acting agent that can safely sedate patients with excited delirium.
Prehospital Studies:
The prehospital community led the way in reporting on ketamine for sedation of acutely agitated patients. One of the original case reports was of a suicidal patient considering jumping off a bridge. Police on the opposite side of a fence held the patient until he was sedated by ketamine and a fire crew could extricate him.[4]
A few years later authors from the Israeli military published their experience with using ketamine in combative trauma patients, as well as a proposed algorithm using ketamine to sedate agitated trauma patients.[5]
Fast forward to 2012 and we get data about ketamine to sedate severely agitated patients in the aeromedical setting and in 2015 within a fire-fighter based EMS system.[6-7]
These studies, and several others, set the stage for two prospective studies on ketamine in the pre-hospital setting, one in 2016 and one in 2018, both from the same group in Minnesota. In the 2016 study Cole, et al found that ketamine was significantly faster at inducing sedation compared with haloperidol (5 min vs 17 min, respectively) and patients who received ketamine required less redosing.[8] In the 2018 study, Cole, et al found the median time to adequate sedation with ketamine was 4.2 min and 90% of patients had adequate sedation prehospital. However, 57% (28/ 49) of patients were intubated.[9]
Whoa, what? 57% intubated? Yikes. This number was higher than other pre-hospital studies reporting intubation rates of 23% , 26% , 29%, 39%, and 63%.[7,10,11,8,12]
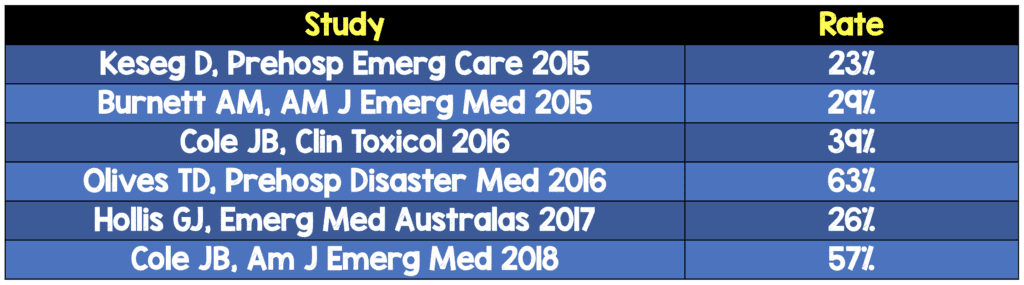
While the pre-hospital intubation rate with ketamine has been the source of much debate[13-15], it was clear that ketamine worked quickly in the prehospital setting.
Emergency Department Studies:
These pre-hospital studies paved the way for several recent studies of emergency department ketamine use. Hopper published a retrospective review in 2015 that described the use of ketamine to treat acute agitation in 27 patients. They found ketamine had few major adverse effects on vital signs in a population with almost 22% alcohol intoxication. No patients were intubated. However, a high proportion (62.5%) of patients required additional pharmacologic treatment for agitation, suggesting that ketamine was useful only for initial control of severe agitation.[16]
The following year a group from Australia published their experience using ketamine as a rescue treatment for patients who had already failed previous sedation attempts.[17] 49 patients were administered rescue ketamine. Five patients (10%) were not sedated within 2 hours or required additional sedation within 1 hour, and the median time to sedation post-ketamine was 20 minutes. No patients were intubated. The authors concluded that ketamine appeared effective and did not cause obvious harm in a small sample and is a potential option for patients who have failed previous attempts at sedation. They recommended ketamine doses of 4-5 mg/kg IM to achieve sedation.
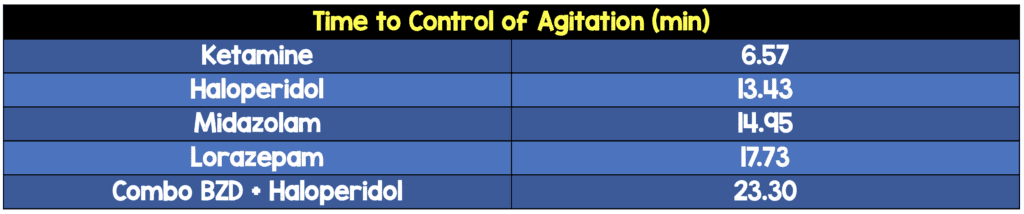
In 2017 we published the first prospective study of ketamine as a first-line agent for sedating acutely agitated emergency department patients.[18] We compared time-to-sedation in patients receiving ketamine, midazolam, haloperidol, lorazepam, and the combination of a benzodiazepine and haloperidol given together. 24 patients were given ketamine and their mean time to sedation was 6.5 minutes, compared with 13 minutes for Haldol, 15 minutes for midazolam, almost 18 minutes for lorazepam, and 23 minutes for the combination treatment. Significantly fewer patients receiving ketamine as a first line sedating agent were agitated at 5-, 10-, and 15-minutes. 8% of patients were intubated.
Another 2017 manuscript highlighted the use of ketamine in the sedation of agitated pediatric patients.[19] Kowalski et al present the successful use of ketamine in 5 agitated adolescent patients with underlying psychiatric disease and/or drug intoxication.
There is little doubt that ketamine is faster than traditional medications in achieving sedation of severely agitated emergency department patients. The questions that remain involve the side effects and risk profile of using ketamine in a population that often has underlying psychiatric disease and/or polysubstance abuse.
Adverse Events:
The high intubation rate seen in prehospital studies does not seem to correlate to the use of ketamine in the emergency department. A meta-analysis (that did not include the Heydari study) found the rate of intubation of agitated ED patients receiving ketamine was 1.8%.[20]
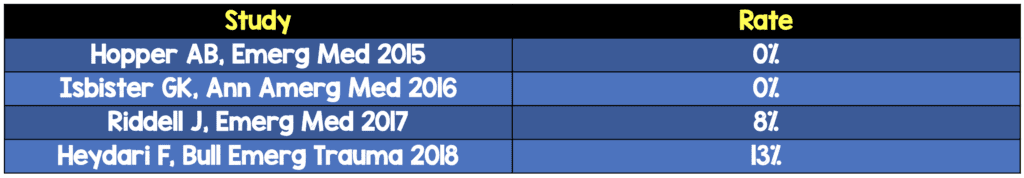
Some have argued that comparing pre-hospital intubation rates to those from the use of ketamine in the ED is an “apples and oranges” [13] comparison. It is important to note though that just because some studies found a high intubation rate, it does not necessarily mean that the patients intubated in those studies absolutely required endotracheal intubation. It is likely that some providers are uncomfortable with dissociated patients and may have chosen to intubate on EMS arrival for unfamiliarity with a “GCS 3K.”[15]
Another lingering concern revolves around the use of ketamine in patients with a history of psychiatric illness. Some fear that the N-methyl-D-aspartic acid (NMDA) receptor antagonist properties of ketamine can cause decompensation of psychiatric illness. The American College of Emergency Physicians Clinical Policy even lists psychiatric illness as an absolute contraindication for procedural sedation with ketamine.[21] While this contraindication has been questioned, a 2019 study by Lebin et al. was the first to provide evidence of psychiatric outcomes in emergency department patients who received pre-hospital ketamine for acute agitation.[22] Compared to patients who received benzodiazipines in the pre-hospital setting, those who were given ketamine had no statistically significant differences for psychiatric inpatient admission or ED psychiatric evaluation. Patients with schizophrenia who received ketamine did not require psychiatric inpatient admission or ED psychiatric evaluation significantly more than those who received benzodiazepines. It appears that in undifferentiated, highly agitated patients, receiving ketamine rather than benzodiazepines for sedation has a minimal impact on meaningful psychiatric outcomes. Our psychiatry colleagues, however, may still disagree.[23] See REBEL EM for a deeper discussion of this phenomenon.
We look forward to the results of an ongoing randomized control trial by a group in Vancouver, B.C. comparing intramuscular ketamine to a combination of intramuscular midazolam and haloperidol with regards to the time required for adequate behavioral control in agitated emergency department patients.[24]
Treatment Algorithm:
While we do not recommend ketamine as a first line agent for the treatment of mild to moderate agitation, it does have a role in the treatment of the combative excited delirium patient. In patients for whom rapid sedation is imperative, consider giving at least 1 mg/kg IV or 5 mg/kg IM of ketamine according to the following algorithm: [25]
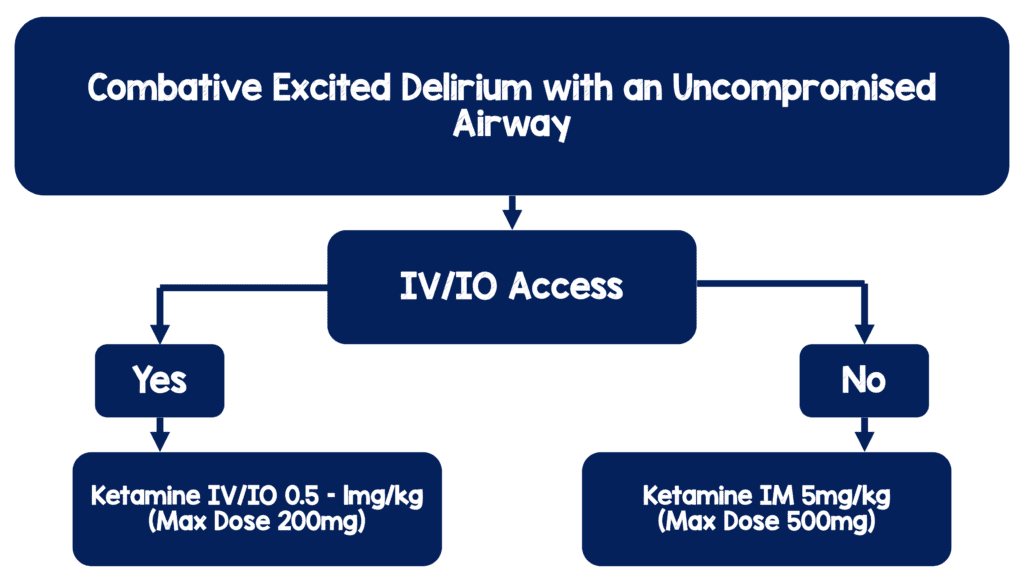
It is important to note that IV/IO access need not be established for the purposes of administering the initial dose of a calming medication. After administration, maintain appropriate oxygen saturation, monitor for side effects, treat injuries, and explore/treat the underlying cause of the patient’s severe agitation.
Guest Post Written By:

Jeff Riddell, MD
Assistant Professor of Clinical Emergency Medicine
Co-Director, Medical Education Fellowship
LA County + USC Emergency Medicine Residency
Department of Emergency Medicine
Keck School of Medicine of the University of Southern California
Los Angeles, CA
Twitter: @jeff__riddell
Expert Peer Review By:

Reuben J. Strayer, MD FRCPC FAAEM
Associate Medical Director
Department of Emergency Medicine
Maimonides Medical Center
Brooklyn, NY
Twitter: @emupdates
References:
- Gonin P, Beysard N, Yersin B, Carron PN. Excited delirium: a systematic review. Acad Emerg Med 2018;25:552–65. PMID: 28990246
- Rossi J, Swan MC, Isaacs ED. The violent or agitated patient. Emerg Med Clin North Am 2010;28(1):235–56. PMID: 19945609
- Battaglia J, Moss S, Rush J, et al. Haloperidol, lorazepam, or both for psychotic agitation? A multicenter, prospective, double-blind, emergency department study. Am J Emerg Med 1997;15(4):335–40. PMID: 9217519
- Hick JL, Ho JD. Ketamine chemical restraint to facilitate rescue of a combative “jumper.” Prehosp Emerg Care 2005;9(1):85–9. PMID: 16036834
- Melamed E, Oron Y, Ben-Avraham R, Blumenfeld A, Lin G. The combative multitrauma patient: a protocol for prehospital management. Eur J Emerg Med 2007;14(5):265–8. PMID: 17823561
- Le Cong M, Gynther B, Hunter E, Schuller P. Ketamine sedation for patients with acute agitation and psychiatric illness requiring aeromedical retrieval. Emerg Med J 2012;29(4):335–7. PMID: 21565879
- Keseg D, Cortez E, Rund D, Caterino J. The use of prehospital ketamine for control of Agitation in a metropolitan firefighter-based EMS system. Prehosp Emerg Care 2015;19:110–5. PMID: 25153713
- Cole JB, Moore JC, Nystrom PC, et al. A prospective study of ketamine versus haloperidol for severe prehospital agitation. Clin Toxicol 2016;54(7):556–62. PMID: 27102743
- Cole JB, Klein LR, Nystrom PC, Moore JC, Driver BE, Fryza BJ, Harrington J, Ho JD. A prospective study of ketamine as primary therapy for prehospital profound agitation. Am J Emerg Med. 2018 May;36(5):789-796. PMID: 29033344
- Hollis GJ, Keene TM, Ardlie RM, Caldicott DG, Stapleton SG. Prehospital ketamine use by paramedics in the Australian Capital Territory: A 12 month retrospective analysis. Emerg Med Australas. 2017 Feb;29(1):89-95. PMID: 27699989
- Burnett AM, Peterson BK, Stellpflug SJ, Engebretsen KM, Glasrud KJ, Marks J, Frascone RJ. The association between ketamine given for prehospital chemical restraint with intubation and hospital admission. Am J Emerg Med. 2015 Jan;33(1):76-9. PMID: 25455046
- Olives TD, Nystrom PC, Cole JB, Dodd KW, Ho JD. Intubation of Profoundly Agitated Patients Treated with Prehospital Ketamine. Prehosp Disaster Med. 2016 Dec;31(6):593-602. PMID: 27640730
- Cole JB, Driver BE, Klein LR, Moore JC, Nystrom PC, Ho JD. In reply: Ketamine is an important therapy for prehospital agitation – Its exact role and side effect profile are still undefined. Am J Emerg Med. 2018 Mar;36(3):502-503. PMID: 29229535
- Miner JR. Ketamine is a good first-line option for severely agitated patients in the prehospital environment. Am J Emerg Med. 2018 Mar;36(3):501-502. PMID: 29329930
- Strayer R. https://emupdates.com/jon-cole-on-ketamine-for-agitation/ Emergency Medicine Updates blog. Nov 2, 2017.
- Hopper AB, Vilke GM, Castillo EM, Campillo A, Davie T, Wilson MP. Ketamine use for acute agitation in the emergency department. J Emerg Med. 2015 Jun;48(6):712-9. PMID: 25843924
- Isbister GK, Calver LA, Downes MA, Page CB. Ketamine as Rescue Treatment for Difficult-to-Sedate Severe Acute Behavioral Disturbance in the Emergency Department. Ann Emerg Med. 2016 May;67(5):581-587. PMID: 26899459
- Riddell J, Tran A, Bengiamin R, Hendey GW, Armenian P. Ketamine as a first-line treatment for severely agitated emergency department patients. Am J Emerg Med. 2017 Jul;35(7):1000-1004. PMID: 28237385
- Kowalski JM, Kopec KT, Lavelle J, Osterhoudt K. A Novel Agent for Management of Agitated Delirium: A Case Series of Ketamine Utilization in the Pediatric Emergency Department. Pediatr Emerg Care. 2017 Sep;33(9):e58-e62. PMID: 26466151
- Mankowitz SL, Regenberg P, Kaldan J, Cole JB. Ketamine for Rapid Sedation of Agitated Patients in the Prehospital and Emergency Department Settings: A Systematic Review and Proportional Meta-Analysis. J Emerg Med. 2018 Nov;55(5):670-681. PMID: 30197153
- Green SM, Roback MG, Kennedy RM, Krauss B. Clinical practice guideline for emergency department ketamine dissociative sedation: 2011 update. Ann Emerg Med. 2011 May;57(5):449-61. PMID: 21256625
- Lebin JA, Akhavan AR, Hippe DS, Gittinger MH, Pasic J, McCoy AM, Vrablik MC. Psychiatric Outcomes of Patients With Severe Agitation Following Administration of Prehospital Ketamine. Acad Emerg Med. 2019 Mar 15. doi: 10.1111/acem.13725. [Epub ahead of print] PMID: 30873690
- Tian LL, Newman WJ. Psychiatric Considerations Regarding Prehospital Administration of Ketamine for Agitation. J Nerv Ment Dis. 2019 Jan;207(1):43-44. PMID: 30575708
- Barbic D, Andolfatto G, Grunau B, Scheuermeyer FX, MacEwan W, Honer WG, Wong H, Barbic SP. Rapid agitation control with ketamine in the emergency department (RACKED): a randomized controlled trial protocol. Trials. 2018 Nov 26;19(1):651. PMID: 30477544
- Linder LM, Ross CA, Weant KA. Ketamine for the Acute Management of Excited Delirium and Agitation in the Prehospital Setting. Pharmacotherapy. 2018 Jan;38(1):139-151. PMID: 29136301
The post The Evolution of Ketamine for Severe Agitation appeared first on REBEL EM - Emergency Medicine Blog.
