 Background: Getting the basics right in all illness is vital. In sepsis, this means appropriate use of antibiotics, judicious fluid resuscitation, and early identification. Vasopressor support is also essential in the sickest sepsis patients (i.e. septic shock). Should the metabolic cocktail (thiamine, vitamin C and hydrocrotisone) be part of that initial package? We’ve previously reviewed the key articles in this area: CITRIS-ALI, VITAMINS, and the original before and after Marik trial. Now we have our next RCT, the HYVCTTSSS trial.
Background: Getting the basics right in all illness is vital. In sepsis, this means appropriate use of antibiotics, judicious fluid resuscitation, and early identification. Vasopressor support is also essential in the sickest sepsis patients (i.e. septic shock). Should the metabolic cocktail (thiamine, vitamin C and hydrocrotisone) be part of that initial package? We’ve previously reviewed the key articles in this area: CITRIS-ALI, VITAMINS, and the original before and after Marik trial. Now we have our next RCT, the HYVCTTSSS trial.
From a pathophysiologic standpoint, Vitamin C levels are thought to be low in critically ill patients with sepsis. Vitamin C is an antioxidant that prevents vascular endothelial damage and helps maintain microvascular integrity. Additionally, it is a cofactor for catecholamine synthesis which helps maintain vascular tone and cardiac output. Glucocorticoids have been shown to reduce time to shock relief and length of ICU stay, but not mortality. The addition of thiamine can help promote oxalate decomposition, which reduces vitamin C metabolites from depositing and crystalizing in kidneys. While these medications are cheap, the more important question is do they improve patient-oriented outcomes? The previous literature on whether this translates to patient oriented benefits has been mostly negative thus far.
Paper: Chang P et al. Combined Treatment with Hydrocortisone, Vitamin C, and Thiamine for Sepsis and Septic Shock (HYVCTTSSS): A Randomized Controlled Clinical Trial. CHEST 2020. PMID: 32243943
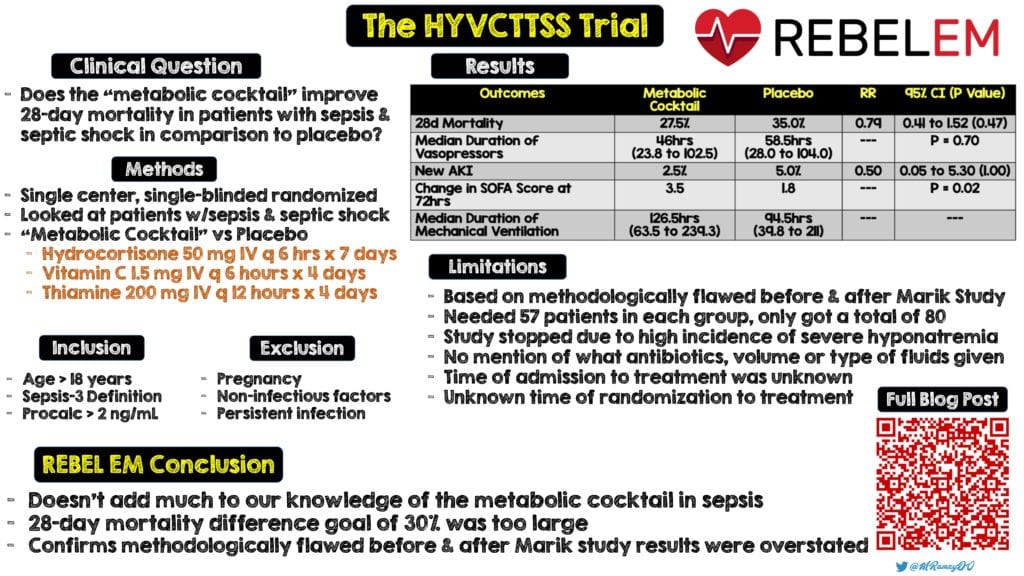
Clinical Question: Does the “metabolic cocktail” improve 28 day mortality in patients with sepsis and septic shock in comparison to placebo?
What They Did:
- Single center, single-blind, randomized, parallel, controlled trial of patients with sepsis and septic shock in China comparing:
- “Metabolic Cocktail” (This is the same cocktail used in the original Marik paper)
- Hydrocortisone 50mg IV q6hr x7d
- Vitamin C 1.5g IV q6hr x4d
- Thiamine 200mg IV q12hr x4d
- Placebo
- 0.9% saline
- “Metabolic Cocktail” (This is the same cocktail used in the original Marik paper)
Outcomes:
- Primary: 28 day all-cause mortality
-
Secondary:
- Duration of vasopressor use
- ICU LOS
- Change in SOFA score within 72hr
- Organ protection (i.e. AKI)
- Procalcitonin reduction within 72hrs
- Adverse events related to hydrocortisone, vitamin C, and thiamine
Inclusion:
- Meeting diagnostic criteria for sepsis using the sepsis-3 definition
- Age ≥18 years
- Procalcitonin ≥2ng/mL when entering the ICU
Exclusion:
- Pregnancy
- Limitations of care (discontinued treatment)
- Non-infectious factors (i.e. head injury, uncontrollable major bleeding, cardiogenic shock, advanced tumors, and paraquat poising)
- Persistent infection sources that could not be removed by puncture and drainage, debridement, or surgical procedures
Results:
- 80 patients randomized
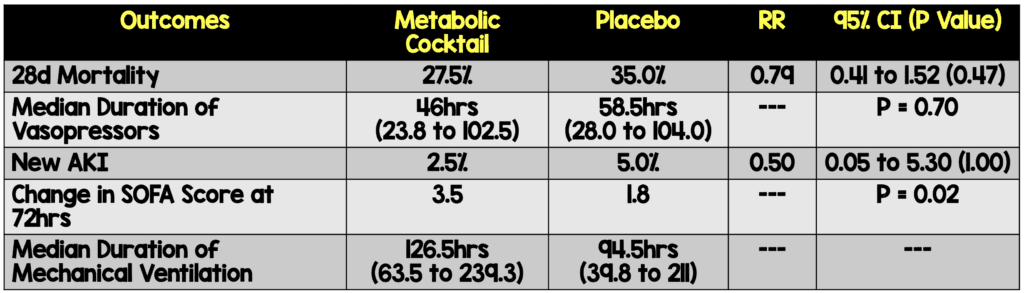
- The pre-specified subgroup analysis showed that in the subgroup of patients diagnosed with sepsis within a duration of ≤48hr at ICU admission, there was an improvement in mortality in the treatment group vs placebo (13.6% vs 47.6%; RR 0.29; 95% CI 0.09 to 0.90; p = 0.02)
- No difference in ICU LOS (7.5d in both groups)
-
Adverse Events:
- 23 side effects recorded
-
Severe Hypernatremia (≥160mmol/L)
- Metabolic Cocktail: 13pts
- Placebo: 3pts
- RR 4.33; 95% CI 1.34 to 14.1; p = 0.005
- GIB in 3 pts in treatment group vs 2 in control group
Strengths:
- Randomized clinical trial that evaluated the primary outcome in three prespecified subgroups that may affect mortality (i.e. age, APACHE II score, and duration of sepsis at enrollment)
- The primary outcome was evaluated with no patients lost to follow up
- Baseline characteristics of patients were similar
- Broad inclusion criteria which is great from a clinical practice standpoint
- Used the same cocktail as the original Marik study, trying to validate the original findings
Limitations:
- The statistical analysis was based on the methodologically flawed before and after Marik study looking for a 30% reduction in mortality, which is a big difference to find for any intervention
- The study required 57 patients in each group to provide a 90% power to detect a 30% difference in mortality and fell well short of this with only 80 patients recruited. There was an interim analysis when the sample size was 50% of total recruitment, which was prespecified within a stopping boundary (statistically significant primary outcome or any adverse events that may affect the treatment of patients). In this case study was stopped due to the high incidence of severe hypernatremia (>160mmol/L) and ineffectiveness of the combined treatment protocol
- 28 out of 40 patients in the control group received only routine treatment with non-administration of placebo due to physicians stating that the use of extra normal saline may not be conducive to volume management of patients. The bias introduced from unblinding in this study isn’t clear.
- It is unclear from this study what volume of fluid, type of fluid, and what antibiotics were used. These are essential elements in the management of sepsis that were not reported
- It is not clear from the paper what the time from admission to treatment and the time from randomization to starting the meds exactly was. For example, does ≤48 hours of sepsis identification mean patients developed sepsis within 48 hours of admission or sepsis was identified within 48 hours? (See Discussion)
- It is unclear from this publication the time from admission to therapy and time from randomization to therapy
Discussion:
- Baseline patient characteristics:
- Pulmonary infection was the most common site of infection in both groups (≈30%)
- Mechanical ventilation was necessary in ≈30% of patients and acute kidney injury was present in ≈20% of cases
- Only about 20% of patient required vasopressors
- Baseline SOFA scores were ≈10 (which equates to a mortality of about 50%) and APACHE II scores ≈22 (which equates to a mortality of about 40%)
- A smaller mortality difference goal would have been more useful. In this trial a 7.5% mortality difference is huge (Even a 3.5% mortality difference would be significant.). A smaller mortality difference would need a much larger trial to be powered correctly. The one thing this trial does tell us however is that the mortality benefit found in the original Marik study, was in fact, too good to be true.
- Septic patients identified in <48hours had a 34% improvement in 28day mortality. It is unclear what is meant by being identified within 48 hours. It is unfortunate that this was not cleared up prior to publication and leaves lots of questions about timing. This outcome needs to be clarified and researched further, but there may be benefit in using the metabolic cocktail at an earlier time window.
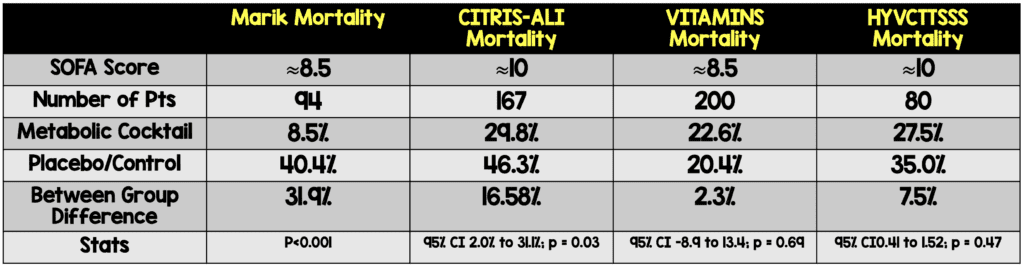
- When comparing the 3 RCTs a few points to mention:
- CITRIS-ALI most likely had the sickest patients when looking at placebo/control mortality rates. It also had the best improvement in mortality
- The VITAMINS trial gave the metabolic cocktail late (i.e. ≈24hrs of septic shock) where we see no improvement in mortality
- The HYVCTTSSS trial also had some fairly sick patients and it is unclear what is exactly meant in the subset of patients “given the metabolic cocktail early (≤48hrs).” There was a statistically significant improvement in mortality of ≈34%, but I am not sure what to do with this as the times are not clearly defined.
- I emailed the lead author to get clarification on ≤48hours and his response was:
- “48 hours means the duration from the time point of sepsis onset (identification by symptoms, signs, examination and tests) to ICU admission, and all the research-related measures were given within 24 hours from ICU admission.”
- PUTTING ALL THIS TOGETHER: Is it possible in the sickest patients (i.e. septic shock), receiving the metabolic cocktail earlier, we may see a significant decrease in mortality? This remains to be proven.
Author Conclusion: “Among patients with sepsis or septic shock, the combination of hydrocortisone, vitamin C, and thiamine did not reduce mortality compared with placebo.”
Clinical Take Home Point: This single center, small study doesn’t really add much to our knowledge of the metabolic cocktail in sepsis. The 28-mortality difference goal of 30% was too large and most likely confirms the methodologically flawed before and after Marik study results were overstated.
Infographic via Mark Ramzy, DO (Twitter: @MRamzyDO)
References:
- Chang P et al. Combined Treatment with Hydrocortisone, Vitamin C, and Thiamine for Sepsis and Septic Shock (HYVCTTSSS): A Randomized Controlled Clinical Trial. CHEST 2020. PMID: 32243943
For More Thoughts on This Topic Checkout:
- REBEL EM: The Marik Protocol – Have We Found a “Cure” for Severe Sepsis and Septic Shock?
- REBEL EM: REBEL Cast Ep 74.0 – Is it all About the VITAMINS in Sepsis?
- REBEL EM: CITRIS-ALI – Vitamin C in Patients with Sepsis and Severe Acute Respiratory Failure
- Journal Feed: HYVCTTSSS RCT – Vit C, Thiamine, Hydrocortisone Cocktail
- PulmCrit: HYVCTTSSS Trial – The Latest Chapter in the Vitamin C Saga
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post The HYVCTTSSS Trial: The “Metabolic Cocktail” in Another RCT appeared first on REBEL EM - Emergency Medicine Blog.